* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download transplantation
DNA vaccination wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Lymphopoiesis wikipedia , lookup
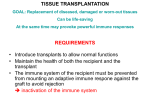
Human leukocyte antigen wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Immune system wikipedia , lookup
Major histocompatibility complex wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Innate immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Molecular mimicry wikipedia , lookup
Bo Gao, Ph.D. Email: [email protected] Tel: 54237379 DEPARTMENT OF IMMUNOLOGY INSTITUTE FOR IMMUNOBIOLOGY 2010-6-28 1 Transplantation is a Dream? • Dream of Paranoia • Dream of excellent surgeon who • wants to excel himself. Dream of excellent scientist who believe nothing is impossible. 2 Can you imagine? Can you imagine? Can you imagine? 3 Contents: Introduction Immunologic Basis of Allograft Rejection Classification and Effector Mechanisms of allograft rejection Prevention and Treatment of Allograft Rejection Xenotransplantation 4 Introduction 5 Transplantation: the process of taking cells, tissues, or organs called a graft (transplant), from one part of individual and placing them into another (usually different individual). Donor: the individual who provides the graft. Recipient or host: the individual who receives the graft. 6 7 8 Inbred mouse strains - all genes are identical 9 The cells of allograft will express alloantigens which are recognized as foreign by the recipient. 10 A xenograft is generally rapidly rejected by the recipient. 11 Experimental kidney transplantation -1912 Nobel Prize in Physiology or Medicine 1912 • Alexis Carrel (France) • Work on vascular suture and the transplantation of blood vessels and organs Great events in history of transplantation 12 Medawar (1945): the graft reaction is an immunity phenomenon Nobel Prize in Physiology or Medicine 1960 • Peter Brian Medawar (1/2) • Discovery of acquired immunological tolerance – The graft reaction is an immunity phenomenon – 1950s, induced immunological tolerance to skin allografts in mice by neonatal injection of allogeneic cells Great events in history of transplantation 13 Discovery of MHC Nobel Prize in Physiology or Medicine 1980 • George D. Snell (1/3), Jean Dausset (1/3) • Discoveries concerning genetically determined structures on the cell surface that regulate immunological reactions – H-genes (histocompatibility genes), H-2 gene – Human leukocyte antigens (HLA) ----MHC Great events in history of transplantation 14 1954 First long-term successful RT(Twin) Nobel Prize in Physiology or Medicine 1990 • Joseph E. Murray (1/2) • Discoveries concerning organ transplantation in the treatment of human disease – In 1954, the first successful human kidney transplant was performed between twins in Boston. – Transplants were possible in unrelated people if drugs were taken to suppress the body's immune reaction Great events in history of transplantation 15 Discovery of Immunosuppressant drug Nobel Prize in Physiology or Medicine 1988 • Gertrude B. Elion (1/3) , George H. Hitchings (1/3) • Discoveries of important principles for drug treatment – Immunosuppressant drug (The first cytotoxic drugs) ----- azathioprine Great events in history of transplantation 16 Today, kidney, pancreas, heart, lung, liver, bone marrow, and cornea transplantations are performed among non-identical individuals with ever increasing frequency and success. 17 Genetic basis of transplant rejection Inbred mouse strains - all genes are identical Transplantation of skin between strains showed that rejection or acceptance was dependent upon the genetics of each strain ACCEPTED Skin from an inbred mouse grafted onto the same strain of mouse REJECTED Skin from an inbred mouse grafted onto a different strain of mouse 18 Immunological basis of graft rejection • Grafts rejection is a kind of specific immune response – Specificity – Immune memory • Grafts rejection – First set rejection – Second set rejection 19 Immunological basis of graft rejection Primary rejection of strain skin e.g. 10 days Transfer lymphocytes from primed mouse Lyc Naïve mouse Transplant rejection is due to an antigenspecific immune response with immunological memory 6 months Secondary rejection of strain skin e.g. 3 days Primary rejection of strain skin e.g. 10 days 20 Immunologic Basis of Allograft Rejection 21 I. Alloantigens Major histocompatibility antigens (MHC molecules) Minor histocompatibility antigens Other alloantigens 22 1. Major histocompatibility antigens Main antigens of grafts rejection Difference of HLA types is the main cause of human grafts rejection Cause fast and strong rejection 23 2. Minor histocompatibility antigens Also cause grafts rejection, but slow and weak Mouse H-Y antigens encoded by Y chromosome HA-1~HA-5 linked with non-Y chromosome 24 25 3. Other alloantigens Human ABO blood group antigens Some tissue specific antigens Skin>kidney>heart>pancreas >liver VEC antigen (vascular endothelial cell) SK antigen 26 Alloantigens elicit both cell-mediated and humoral immune responses, eventually leading to the disruption of grafts. Why alloantigens can elicit strong rejection reactions ? 27 T cells of the recipient recognize the allogenetic MHC molecules Many T cells can recognize allogeneic MHC molecules. 10-5-10-4 of specific T cells recognize conventional antigens. 1%-10% of T cells recognize allogeneic MHC molecules. 28 T cells of the recipient recognize the allogeneic MHC molecules Direct Recognition Indirect Recognition 29 Direct Recognition T cell recognizes an intact allogeneic MHC molecule on graft. 30 Indirect recognition Uptake and presentation of allogeneic donor MHC molecules by recipient APC in “normal way” Recognition by T cells like conventional foreign antigens 31 Difference between Direct Recognition and Indirect Recognition Direct Recognition Indirect Recognition Allogeneic MHC molecule Intact allogeneic MHC molecule Peptide of allogeneic MHC molecule APCs Recipient APCs are not necessary Recipient APCs Roles in rejection Acute rejection Chronic rejection Degree of rejection Vigorous Weak 32 As mentioned above, alloreactive T cells in the recipient can be activated by both pathways, and these T cells will migrate into the graft. What role will these activated T lymphocytes play in the rejection response? 33 Role of CD4+T cells in the rejection response Activated CD4+T by direct and indirect recognition CK secretion MΦ activation and recruitment Damage grafts by reactions that resemble delayed-type hypersensitivity (DTH) 34 Role of CD8+T cells in the rejection response Activated CD8+T by direct recognition can directly Kill the graft cells, which express the allogeneic calss I MHC molecules. 35 36 Humoral immunity in rejection response Important role in hyperacute rejection (Preformed antibodies) Complements activation Antibody-dependent cellular cytotoxicity (ADCC) Opsonization 37 Role of NK cells • KIR can’t recognize allogeneic MHC on graft • CKs secreted by activated Th cells can promote NK activation 38 Classification and Effector Mechanisms of Allograft Rejection 39 Classification of Allograft Rejection Host versus graft reaction (HVGR) Conventional organ transplantation Graft versus host reaction (GVHR) Bone marrow transplantation Immune cells transplantation 40 I. Host versus graft reaction (HVGR) Hyperacute rejection Acute rejection Chronic rejection 41 1. Hyperacute rejection Occurrence time – Occurs within minutes to hours after host blood vessels are anastomosed to graft vessels Pathology – Thrombotic occlusion of the vasculature – Ischemia, denaturation, necrosis graft 42 1. Hyperacute rejection Mechanisms – Preformed antibodies • Antibody against ABO blood type antigen • Antibody against VEC antigen • Antibody against HLA antigen – Complement activation • Endothelial cell damage – Platelets activation • Thrombosis, vascular occlusion, ischemic damage 43 1. Hyperacute rejection 44 45 1. Hyperacute rejection Hyperacute rejection of a kidney allograft with endothelial damage, platelet and thrombin thrombi, and early neutrophil infiltration in a glomerulus. 46 2. Acute rejection Occurrence time Occurs within days to 2 weeks after transplantation, 80-90% of cases occur within 1 month. Pathology Acute rejection is a process of vascular and parenchymal injury mediated by T cells and antibodies. CD4+ T cells , CD8+ T cells and antibodies may contribute to acute rejection. 47 2. Acute rejection Mechanisms Parenchymal cell damage DTH-like reaction mediated by CD4+Th1 Killing of graft cells by CD8+Tc Vasculitis Antibodies can also mediate acute rejection if a graft recipient mounts a humoral immune response to vessel wall antigens. The antibodies that are produced bind to the vessel wall and activate complement. 48 49 2. Acute rejection Acute rejection of a kidney with inflammatory cells in the interstitium and between epithelial cells of the 50 tubules. 3. Chronic rejection Occurrence time – Develops months or years after acute rejection reactions have subsided Pathology – Fibrosis and vascular abnormalities with loss of graft function 51 3. Chronic rejection Mechanisms – Not clear – Extension and results of cell necrosis in acute rejection – Chronic inflammation mediated by CD4+T cell/MΦ – Organ degeneration induced by non immune factors 52 1.Macrophage-T cell mediated 2. Chronic DTH reaction injury of vessel wall 3. Proliferation of smooth muscle cell and luminal occlusion 53 Kidney Transplantation----Graft Rejection 54 56 II.Graft versus host reaction (GVHR) Graft versus host reaction (GVHR) – Allogeneic bone marrow transplantation – Rejection to host alloantigens – Mediated by immune competent cells in bone marrow Graft versus host disease (GVHD) A disease caused by GVHR, which can damage the host 57 II.Graft versus host reaction (GVHR) Graft versus host disease 58 II.Graft versus host reaction (GVHR) Conditions Enough immune competent cells in grafts Immunocompromised host Histocompatability between host and graft differences 59 II.Graft versus host reaction (GVHR) Bone marrow transplantation Thymus transplantation Spleen transplantation Blood transfusion of neonate In most cases the reaction is directed against minor histocompatibility antigens of the host. 60 1. Acute GVHD Endothelial cell death in the skin, liver, and gastrointestinal tract Rash, jaundice, diarrhea, gastrointestinal hemorrhage Mediated by mature T cells in the grafts 61 Acute graft-versus-host reaction with vivid palmar erythema 62 2. Chronic GVHD Fibrosis and atrophy of one or more of the organs without evidence of acute cell death. Eventually complete dysfunction of the affected organ and may be fatal. 63 Prevention and Therapy of Allograft Rejection 65 • Tissue Typing • Immunosuppressive Therapy • Induction of Immune Tolerance 66 I. Tissue Typing • ABO and Rh blood typing • Crossmatching (Preformed antibodies) • HLA typing – HLA-A and HLA-B – HLA-DR 67 II. Immunosuppressive Therapy • Cyclosporine(CsA), FK506 – Inhibit NFAT transcription factor • Azathioprine, Cyclophosphamide – Block the proliferation of lymphocytes • Ab against T cell surface molecules – Anti-CD3 mAb----Deplete T cells • Anti-inflammatory agents – Corticosteroids----Block the synthesis and secretion of cytokines 68 Removal of T cells from marrow graft 69 III. Induction of Immune Tolerance • Inhibition of T cell activation – Soluble MHC molecules – CTLA4-Ig – Anti-IL2R mAb • Th2 cytokines – Anti-TNF-α,Anti-IL-2,Anti-IFN-γ mAb • Microchimerism – The presence of a small number of cells of donor, genetically distinct from those of the host individual 70 Part IV Xenotransplantation 71 • Lack of organs for transplantation 72 From which animals are we able to transplant organs 1. The Chimpanzee: Its DNA sequence differs from ours by only 2% 2. The Baboon: Its organs are too small for a large adult human 3. The Pig: Surprisingly similar to our anatomy and physiology 73 • Hyperacute xenograft rejection (HXR) – Human anti-pig nature Abs reactive with Galα1,3Gal – Construct transgenic pigs expressing human proteins that inhibit complement activation • Delayed xenograft rejection (DXR) – Acute vascular rejection – Incompletely understood • T cell-mediated xenograft rejection 74 75