* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ch23.Digestive.System_1
Survey
Document related concepts
Transcript
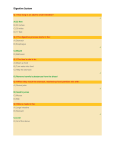
Topics for Student Presentations Presentations in lab on Mon, May 13; ~5-6 min, any style! 2-5 people per group Anatomy & Physiology (or Pathophysiology) of: •Heart Disease •Cleft Palate •AIDS •Leukemia •Crohn’s Disease •Pancreatic Cancer •Diabetes mellitus •Gut bacteria & the effects of antibiotics •Gall stones •The hepatic portal system •Liver Disease (cirrhosis) •Kidney Stones •Kidney Failure & Dialysis •Common cancers of GI tract •Competitive Eating •Addiction •Obesity •Effects of Exercise on the whole body •Fraternal, Identical, & Siamese Twins •Endometriosis •Cervical & Ovarian Cancer •Premature Ovarian Failure •Female causes of Infertility •Male causes of Infertility •Prostate Cancer and/or Breast Cancer •Androgen Insensitivity Syndrome •Klinefelter’s Syndrome (XXY) •Turner’s Syndrome (XO) •Kallman’s Syndrome •Growth Hormone Deficiency & Excess •Disorders of the thyroid (ie. Graves’) •Cushing’s Disease •Addison’s Disease The Digestive System Ch 23 Leonardo Da Vinci Human Anatomy Sonya Schuh-Huerta, Ph.D. Function of the Digestive System Digestion = the mechanical & chemical breakdown of food to allow absorption of nutrients into the bloodstream The Building Blocks Overview of the Digestive System • Organs are divided into 2 groups – Alimentary canal (= GI tract) • Mouth, pharynx, & esophagus • Stomach, small intestine, & large intestine – Accessory digestive organs • Teeth & tongue • Salivary glands, gallbladder, liver, & pancreas – Accessory organs are connected to the alimentary canal by ducts • Secretions contribute to breakdown of foodstuffs The Alimentary Canal & Accessory Digestive Organs Mouth (oral cavity) Tongue Esophagus Liver Parotid gland Sublingual gland Salivary glands Submandibular gland Pharynx Stomach Pancreas (Spleen) Gallbladder Duodenum Small intestine Jejunum Ileum Anus Transverse colon Descending colon Ascending colon Cecum Large intestine Sigmoid colon Rectum Vermiform appendix Anal canal Digestive Processes • 1.) Ingestion occurs in the mouth • 2.) Propulsion movement of food – Peristalsis major means of propulsion • 3.) Mechanical digestion physical breakdown of food, prepares food for chemical digestion – Chewing, churning of food in stomach • Segmentation rhythmic local constrictions of intestine Digestive Processes • 4.) Chemical digestion complex molecules broken down to chemical components – Mouth – Stomach – Small intestine • 5.) Absorption transport of digested nutrients into the blood • 6.) Defecation elimination of indigestible substances as feces Digestion in Action animation by www.encognitive.com Digestive Processes Ingestion Mechanical digestion • Chewing (mouth) • Churning (stomach) • Segmentation (small intestine) Chemical digestion Food Pharynx Esophagus Propulsion • Swallowing (oropharynx) • Peristalsis (esophagus, stomach, small intestine, large intestine) Stomach Absorption Lymph vessel Small intestine Large intestine Defecation Blood vessel Mainly H2O Feces Anus Figure 23.2 Peristalsis • Major means of propulsion • Adjacent segments of the alimentary canal relax & contract Segmentation • Rhythmic local contractions of the intestine • Mixes food with digestive juices Microscopic Anatomy of the Digestive Tract clipartguide.com Histology of the Alimentary Canal Wall • Same 4 layers from esophagus to anus • The mucosa innermost layer (lines the lumen) • Consists of: – Epithelium – Lamina propria (many capillaries & lymphoid tissue) – Muscularis mucosae (2 layers of smooth m.) • The submucosa external to the mucosa – Contains blood & lymphatic vessels, nerve fibers, glands, etc. Histology of the Alimentary Canal Wall • The muscularis externa (or muscularis) external to the submucosa – 2 layers •Circular muscularis inner layer •Longitudinal muscularis outer layer • The serosa the outermost layer *Is the visceral peritoneum (remember this?…) Histology of the Alimentary Canal Intrinsic nerve plexuses Myenteric nerve plexus Submucosal nerve plexus Glands in submucosa Mucosa Epithelium Lamina propria Muscularis mucosae Submucosa Muscularis externa Longitudinal muscle Circular muscle Serosa Epithelium Connective tissue Mesentery Nerve Artery Gland in mucosa Vein Duct of gland outside Lymphatic vessel alimentary canal (a) Longitudinal and cross-sectional views through the small intestine Lumen Mucosa-associated lymphoid tissue Histology of the Alimentary Canal Mucosa Submucosa Muscularis externa Serosa (b) Light micrograph cross section through the small intestine (30) Smooth Muscle • • • • Primarily found in walls of viscera Fibers elongated Have one centrally located nucleus Grouped into sheets – Longitudinal layer parallel to long axis of organ – Circular layer deeper layer, fibers run around circumference of organ Smooth Muscle Longitudinal layer of smooth muscle (shows smooth muscle fibers in cross section, 145) Small intestine (a) Location and plane of section shown in (b) Mucosa (b) Cross section of the intestine showing the smooth muscle layers (one circular and the other longitudinal) running at right angles to each other Circular layer of smooth muscle (shows longitudinal views of smooth muscle fibers, 145) Smooth Muscle Contraction • Myofilaments operate by interaction with cytoskeleton • Dense bodies similar to Z-discs of skeletal muscle • No sarcomeres (but Ca2+ is a key player) Intermediate filament Caveolae Gap junctions Dense bodies Nucleus (a) Relaxed smooth muscle fiber (note that adjacent fibers are connected by gap junctions) Nucleus Dense bodies (b) Contracted smooth muscle fiber Exercising Your Muscle Memory Innervation of Smooth Muscle • Innervated by ANS (remember this..?) • Few fibers per sheet innervated – Sheet of smooth muscle contracts as a unit • Exceptions – Iris of eye – Arrector pili muscles in skin Innervation of Smooth Muscle Varicosities Autonomic nerve fibers innervate most smooth muscle fibers. Smooth muscle cell Synaptic vesicles Mitochondrion Varicosities release their neurotransmitters into a wide synaptic cleft (a diffuse junction) Nerve Plexuses • Myenteric nerve plexus • Lies in muscularis externa • Controls peristalsis & segmentation • Submucosal nerve plexus – Lies in submucosa – Signals glands to secrete • Innervation – Sympathetic & parasympathetic motor fibers – Visceral sensory fibers Nerve Plexuses Intrinsic nerve plexuses Myenteric nerve plexus Submucosal nerve plexus Glands in submucosa Mucosa Epithelium Lamina propria Muscularis mucosae Submucosa Muscularis externa Longitudinal muscle Circular muscle Serosa Epithelium Connective tissue Mesentery Nerve Artery Gland in mucosa Vein Duct of gland outside Lymphatic vessel alimentary canal Lumen Mucosa-associated lymphoid tissue (a) Longitudinal and cross-sectional views through the small intestine Gross & Microscopic Anatomy of Organs of the Digestive Tract Use as a Lab Guide (both lecture & lab material!) The Mouth & Associated Organs • The mouth oral cavity – Mucosal layer • Stratified squamous epithelium • Lamina propria • The lips & cheeks – Formed from orbicularis oris & buccinator muscles, respectively (remember these?…) Anatomy of the Mouth Soft palate Palatoglossal arch Hard palate Oral cavity Palatine tonsil Tongue Oropharynx Lingual tonsil Epiglottis Hyoid bone Laryngopharynx Esophagus Trachea (a) Sagittal section of the oral cavity and pharynx Uvula Anatomy of the Mouth • The labial frenulum – Connects lips to gums • The palate – Forms the roof of the mouth Gingivae (gums) Palatine raphe Upper lip Superior labial frenulum Soft palate Palatoglossal arch Palatopharyngeal arch Uvula Palatine tonsil Posterior wall of oropharynx Hard palate Tongue Sublingual fold with openings of sublingual ducts Lingual frenulum Opening of submandibular duct Gingivae (gums) Vestibule Lower lip (b) Anterior view Inferior labial frenulum The Tongue • • • • • • Interlacing fascicles of skeletal muscle Grips food & repositions it – aids in mastication Helps form some consonants in speaking Intrinsic muscles within the tongue Extrinsic muscles external to the tongue Lingual frenulum – Secures tongue to floor of mouth The Superior Surface of the Tongue • Tongue papillae – Filiform papillae No taste buds – Fungiform & vallate papillae Taste buds • Posterior 1/3 of tongue lingual tonsil Superior Surface of the Tongue Epiglottis Palatopharyngeal arch Palatine tonsil Lingual tonsil Palatoglossal arch Terminal sulcus Vallate papilla Midline groove of tongue Fungiform papilla Filiform papilla The Teeth • Deciduous (“milk”) teeth 20 teeth – Begin to appear at 6 months of age • Permanent teeth 32 teeth – Most erupt by the end of adolescence • Dental formula shorthand – Way to indicate number & position of teeth • 2I, 1C, 2P, 3M The Teeth Deciduous teeth Permanent teeth Tooth Structure Enamel Dentin • Longitudinal section of tooth in alveolus Crown Dentinal tubules Pulp cavity (contains blood vessels and nerves) Neck Gingiva (gum) Cementum Root Root canal Periodontal ligament Apical foramen Bone The Salivary Glands • Exocrine glands (= have ducts) • Produce saliva & secrete amylase enzyme breaks down starch (complex carbs) into maltose 1st stage of chemical digestion! • Compound tubuloalveolar glands – Parotid glands – Submandibular glands – Sublingual glands The Salivary Glands Tongue Teeth Ducts of sublingual gland Frenulum of tongue Sublingual gland Mylohyoid muscle (cut) Anterior belly of digastric muscle Parotid gland Parotid duct Masseter muscle Body of mandible (cut) Posterior belly of digastric muscle Submandibular duct Submandibular gland Mucous cells Serous cells forming demilunes The Pharynx • Oropharynx & laryngopharynx – Passages for air & food – Lined with stratified squamous epithelium – External muscle layer • Consists of superior, middle, & inferior pharyngeal constrictors (…remember these?) The Pharynx Cribriform plate of ethmoid bone Frontal sinus Nasal cavity Nasal conchae (superior, middle and inferior) Sphenoid sinus Posterior nasal aperture Nasopharynx Pharyngeal tonsil Opening of pharyngotympanic tube Nasal meatuses (superior, middle, and inferior) Nasal vestibule Nostril Uvula Oropharynx Palatine tonsil Isthmus of the fauces Hard palate Soft palate Laryngopharynx Lingual tonsil Hyoid bone Esophagus Trachea Tongue Larynx Epiglottis Vestibular fold Thyroid cartilage Vocal fold Cricoid cartilage Thyroid gland The Esophagus • Gross anatomy muscular tube – Begins as a continuation of the pharynx – Joins the stomach inferior to the diaphragm – Hole through diaphragm that allows esophagus through hiatus • Cardiac sphincter closes lumen to prevent stomach acid from entering esophagus The Esophagus • Microscopic anatomy – Stratified squamous epithelium – When empty, mucosa & submucosa in longitudinal folds – Mucus glands – Muscularis externa • Skeletal muscle first 1/3 of length – Adventitia most external layer Microscopic Structure of Esophagus Mucosa (contains a stratified squamous epithelium) Submucosa (areolar connective tissue) Lumen Muscularis externa Circular layer Longitudinal layer Adventitia (fibrous connective tissue) (a) Cross section through esophagus (5) (b) Gastroesophageal junction, longitudinal section (85) The Stomach • Site where food is churned into chyme • Secretion of pepsin begins protein digestion – Functions under acidic conditions • Food remains in stomach ~1–4 hours • Rugae ridges of stomach mucosa • Regions of the stomach: – – – – Cardiac region Fundus Body Pyloric region The Stomach Cardiac region Fundus Esophagus Muscularis externa Longitudinal layer Circular layer Oblique layer Serosa Body Lumen Lesser curvature Rugae of mucosa Greater curvature Duodenum Pyloric canal Pyloric sphincter (valve) at pylorus Pyloric antrum The Stomach Liver (cut) Fundus Body Spleen Lesser curvature Greater curvature Microscopic Anatomy of the Stomach • Muscularis has 3 layers – Circular & longitudinal layers AND oblique layer • Epithelium is simple columnar epithelium • Mucosa dotted with gastric pits – Gastric glands deep to gastric pits Microscopic Anatomy of the Stomach • Gastric glands of fundus & body – Mucous neck cells • Secrete a special mucus – Parietal cells • Secrete HCl & gastric intrinsic factor – Chief cells • Secrete pepsinogen – Pepsinogen is activated to pepsin when it encounters acid in the gastric glands The Stomach – Microscopic Anatomy Gastric pits Surface epithelium (mucous cells) Gastric pit Mucous neck cells Parietal cell Gastric gland Chief cell Enteroendocrine cell (b) Enlarged view of gastric pits and gastric glands The Stomach – Microscopic Anatomy Pepsinogen Pepsin HCl Mitochondria Parietal cell Chief cell Enteroendocrine cell (c) Location of the HCl-producing parietal ells and pepsin-secreting chief cells in a gastric gland The Stomach – Microscopic Anatomy Mucus-secreting cells Gastric pits Surface mucous cell Mucus neck cells Gastric gland HCl secreting parietal cells Enzyme secreting chief cells Muscularis mucosae (d) Micrograph of the stomach mucosa (115) The Small Intestine • Longest portion of GI tract • Site of most enzymatic digestion & absorption chyme here ~3–6 hrs • 3 subdivisions: 16 ft long! – Duodenum – Jejunum – ileum 200 square meters! • Innervation – Parasympathetic fibers from vagus nerve – Sympathetic from thoracic splanchnic nerves • Small & large intestine site of quadrillions of microorganisms!!! The Gut Flora • 10X as many microbes as there are cells of the human body!!! • Perform many metabolic activities “forgotten organ” • Bacteria most of the flora, also fungi & protozoa • Makes up 60% of the dry mass of feces! • About 500 species in gut (small & large intestines) • 99% of bacteria from about 30–40 species • Symbiotic Relationship! – Fermenting unused substrates (carbs SCFAs) – Training Immune System – Preventing growth of harmful pathogenic bacteria – Regulating development of the gut – Producing vitamins (biotin/B vitamins, vit K, etc.) – Producing hormones (that mediate fat storage) The Duodenum • Receives digestive enzymes & bile from pancreas & gallbladder • Main pancreatic duct & common bile duct enter duodenum – Sphincters control entry of bile & pancreatic juices The Duodenum & Related Organs Right & left hepatic ducts of liver Liver Common hepatic duct Cystic duct Common Bile duct & sphincter Accessory pancreatic duct Mucosa with folds Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter Duodenum Tail of pancreas Pancreas Jejunum Main pancreatic duct & sphincter Head of pancreas Small Intestine – Adaptations for Absorption – Circular folds (plicae circulares) • Transverse ridges of mucosa & submucosa – Villi • Finger-like projections of the mucosa • Covered with simple columnar epithelium – Microvilli • Many tiny microvilli on apical surface of cells • Villi & microvilli further increase surface area for absorption Microscopic Anatomy of Small Intestine • Absorptive cells – Uptake digested nutrients • Goblet cells – Secrete mucus that lubricates chyme & forms protective barrier • Enteroendocrine cells – Secrete hormones that stimulate pancreas & gallbladder • Intestinal crypts – Epithelial cells secrete intestinal juice – Rapidly dividing epithelial cells (stem cells) replace epithelium every 3–6 days!!! Without these, you would lose your entire intestine within a week! The Small Intestine – Structural Features Vein carrying blood to hepatic portal vessel Muscle layers Microvilli (brush border) Lumen Circular folds Absorptive cells Villi Lacteal Goblet cell Blood capillaries (a) Mucosa associated lymphoid tissue Intestinal crypt Muscularis mucosae (b) Duodenal gland Absorptive cells Vilus Goblet cells Villi Enteroendocrine cells Venule Lymphatic vessel Submucosa Stem cells (c) Intestinal crypt The Large Intestine • • • • Digested residue contains few nutrients In large intestine ~12–24 hrs Some digestion by bacteria Main functions: – Absorb water & electrolytes (NaCl) • Mass peristaltic movements force feces toward rectum Gross Anatomy of Large Intestine • Subdivided into: – Cecum, vermiform appendix, colon, rectum, anal canal • Special features of large intestine: – Teniae coli • Thickening of longitudinal muscularis – Haustra • Puckering created by teniae coli – Epiploic appendages • Fat-filled pouches of visceral peritoneum Gross Anatomy of Large Intestine Left colic (splenic) flexure Transverse mesocolon Right colic (hepatic) flexure Epiploic appendages Transverse colon Superior mesenteric artery Descending colon Haustrum Ascending colon Cut edge of mesentery IIeum IIeocecal valve Teniae coli Cecum Sigmoid colon Vermiform appendix Rectum Anal canal External anal sphincter Gross Anatomy of Large Intestine • Cecum – Blind pouch – Beginning of large intestine • Vermiform appendix – Contains lymphoid tissue – Neutralizes pathogens • Colon – Divided into distinct segments • Ascending, transverse, descending, & sigmoid colon Gross Anatomy of Large Intestine Left colic (splenic) flexure Transverse mesocolon Right colic (hepatic) flexure Epiploic appendages Transverse colon Superior mesenteric artery Descending colon Haustrum Ascending colon Cut edge of mesentery IIeum IIeocecal valve Teniae coli Cecum Sigmoid colon Vermiform appendix Rectum Anal canal External anal sphincter Gross Anatomy of Large Intestine • Rectum – Descends along the inferior half of the sacrum • Anal canal – The last subdivision of the large intestine – Lined with stratified squamous epithelium Gross Anatomy of Rectum & Anal Canal Rectal valve Rectum Hemorrhoidal veins Levator ani muscle Anal canal External anal sphincter Internal anal sphincter Anal columns Anal valves Pectinate line Anal sinuses Anus Microscopic Anatomy of Large Intestine • Villi are absent • Contains numerous goblet cells (mucus) • Intestinal crypts • Lined with simple columnar epithelium – Epithelium changes at anal canal Looks “fern-like” • Becomes stratified squamous epithelium Microscopic Anatomy of Large Intestine Absorptive cells Lamina propria Goblet cells Intestinal crypts Looks “fern-like” Muscularis mucosae The Liver • Largest gland in the body – Performs over 500 functions… – Digestive function: • Bile production • Bile emulsifies (breaks up) fats into tiny particles that are more accessible to digestive enzymes – Performs many metabolic functions! – Body storage site of glucose (as glycogen) – Processes fats, amino acids, & stores vitamins – Detoxifies many poisons & toxins in the blood – Makes & breaks down blood proteins The Liver Sternum Nipple Bare area Liver Falciform ligament Left lobe of liver Right lobe of liver Gallbladder Round ligament (ligamentum teres) Visceral Surface of the Liver Lesser omentum (in fissure) Caudate lobe of liver Left lobe of liver Porta hepatis containing hepatic artery (left) and hepatic portal vein (right) Quadrate lobe of liver Bare area Sulcus for inferior vena cava Hepatic vein (cut) Bile duct (cut) Right lobe of liver Ligamentum teres Gallbladder Visceral Surface of the Liver Hepatic portal vein Caudate lobe Hepatic veins Inferior vena cava Bare area Left lobe Ligamentum venosum in fissure Porta hepatis Right hepatic artery Left hepatic artery Right hepatic duct Left hepatic duct Cystic duct Common hepatic duct Gallbladder Fissure Falciform ligament Ligamentum teres Right lobe Quadrate lobe Microscopic Anatomy of the Liver • Hepatocyte = functional cell of the liver • Portal triad composed of: – Bile duct tributary – Branch of hepatic portal vein – Branch of hepatic artery Portal triad Lobule Central vein Microscopic Anatomy of the Liver (a) (b) Lobule Central vein Connective tissue septum Interlobular veins (to hepatic vein) Central vein Sinusoids Bile canaliculi Plates of hepatocytes Bile duct (receives bile from bile canaliculi) Fenestrated lining (endothelial cells) of sinusoids Hepatic macrophages in sinusoid walls Portal vein (c) Bile duct Portal venule Portal arteriole Portal triad Functions of Hepatocytes • Some functions of hepatocytes: – – – – – – – Rough ER manufactures blood proteins Smooth ER produces bile salts, detoxifies poisons Peroxisomes detoxify poisons (alcohol) Golgi apparatus packages secretory products Mitochondria provide energy for liver processes Glycosomes store sugar (as glycogen) Great capacity for regeneration! The Gallbladder • Stores & concentrates bile • Expels bile into duodenum • Cholecystokinin – Released from enteroendocrine cells of small intestine in response to fatty chyme – Causes contraction of gallbladder & entry of bile into duodenum The Gallbladder & Related Organs Right & left hepatic ducts of liver Liver Common hepatic duct Cystic duct Common Bile duct & sphincter Accessory pancreatic duct Mucosa with folds Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter Duodenum Tail of pancreas Pancreas Jejunum Main pancreatic duct & sphincter Head of pancreas The Pancreas • Exocrine function (exocrine pancreas) – Acinar cells make, store, & secrete pancreatic enzymes (get dumped into duodenum) – Enzymes are activated in duodenum • Endocrine function (endocrine pancreas) – Cells of pancreatic islets (Islets of Langerhans) Produce insulin & glucagon & somatostatin Regulate blood sugar The Exocrine Pancreas – Histology Diaphragm Liver Spleen Pancreas Tail Body Head Duodenum Acinar cells (b) Photomicrograph of the exocrine acinar cells of the pancreas (160) Small duct Acinar cells (a) Dissection illustrating the pancreas and its relationship to surrounding organs in the superior abdomen Basement membrane Zymogen granules Rough endoplasmic reticulum (c) Illustration of the pancreatic acinar cells Morphology & Function of GI Organs Morphology & Function of GI Organs Abdominal Regions • 4 lines divide abdominal wall into 9 regions – Midclavicular lines vertical lines of grid – Subcostal plane superior horizontal line • Connects inferior points of costal margin – Transtubercular plane inferior horizontal line • Connects tubercles of iliac crests 9 Regions of Anterior Abdominal Surface Right hypochondriac region Right lumbar region Right iliac (inguinal) region Epigastric region Left hypochondriac region Umbilical region Left lumbar region Hypogastric (pubic) region Left iliac (inguinal) region (a) Nine regions delineated by four planes 9 Regions of Anterior Abdominal Surface • How regions relate to abdominal viscera Liver Diaphragm Gallbladder Stomach Ascending colon of large intestine Small intestine Cecum Appendix Transverse colon of large intestine Descending colon of large intestine Initial part of sigmoid colon Urinary bladder (b) Anterior view of the nine regions showing the superficial organs Abdominal Quadrants • A simpler method of sectioning the anterior abdominal wall – Right upper quadrant – Left upper quadrant – Right lower quadrant – Left lower quadrant The Peritoneal Cavity & Peritoneum • Peritoneum a serous membrane – Visceral peritoneum surrounds digestive organs – Parietal peritoneum lines the body wall • Peritoneal cavity a slit-like potential space The Peritoneal Cavity & Peritoneum • Mesentery a double layer of peritoneum – Holds organs in place – Sites of fat storage – Provides a route for circulatory vessels & nerves The Peritoneal Cavity & Peritoneum Abdominopelvic cavity Liver Alimentary canal organ Ventral mesentery Alimentary canal organ Alimentary canal organ in a retroperitoneal position Parietal peritoneum Visceral peritoneum Peritoneal cavity Vertebra Dorsal mesentery (a) Schematic cross sections of abdominal cavity illustrating the peritonea and mesenteries Falciform ligament Anterior Visceral peritoneum Peritoneal cavity (with serous fluid) Liver Stomach Parietal peritoneum Kidney (retroperitoneal) Posterior Wall of body trunk (b) Illustration of the peritonea in a cross section through the superior abdomen, inferior view Mesentery resorbed and lost (c) Some organs lose their mesentery and become retroperitoneal during development. The Peritoneal Cavity & Peritoneum • Retroperitoneal organs – Behind the peritoneum • Peritoneal organs – Digestive organs that keep their mesentery Mesenteries • Superficial view of abdominal organs Falciform ligament Liver Gallbladder Spleen Stomach Ligamentum teres Greater omentum Small intestine Cecum (a) Mesenteries • Greater omentum a “fatty apron” of peritoneum • Greater omentum & transverse colon reflected Greater omentum Transverse colon Transverse mesocolon Descending colon Jejunum Mesentery Sigmoid mesocolon Sigmoid colon Ileum Mesenteries • Lesser omentum attaches to lesser curvature of stomach Liver Gallbladder Lesser omentum Stomach Duodenum Transverse colon Small intestine Cecum Urinary bladder Mesenteries • Sagittal section through the abdominopelvic cavity • Mesenteries attach to posterior abdominal wall Liver Lesser omentum Pancreas Stomach Duodenum Transverse mesocolon Transverse colon Mesentery Greater omentum Jejunum Ileum Visceral peritoneum Parietal peritoneum Urinary bladder Rectum Secondarily Retroperitoneal Organs • Initially formed within peritoneum • Become retroperitoneal – Fuse to posterior abdominal wall Summary of Intraperitoneal & Secondarily Retroperitoneal Organs Disorders of the Digestive System • Peptic Ulcers Are erosions of the mucosa of a region of the alimentary canal Gastric ulcers Occur in pyloric region of the stomach Duodenal ulcers Occur in duodenum of the small intestine Peptic Ulcers • Caused by Helicobacter pylori • H. pylori – Acid-resistant – Binds to gastric epithelium • Induces oversecretion of acid & inflammation Peptic Ulcers Bacteria Mucosa layer of stomach (a) A gastric ulcer lesion (b) H. Pylori bacteria Disorders of the Digestive System • Intestinal obstruction – Mechanical obstructions • Adhesions, tumors, or foreign objects – Nonmechanical obstruction • Halt in peristalsis – Trauma – Intestines touched during surgery Disorders of the Digestive System • Inflammatory bowel disease – Inflammation of intestinal wall • Crohn’s disease • Ulcerative colitis • Viral hepatitis – Jaundice & flu-like symptoms – Major types A, B, C, & G • Liver Disease acute hepatitis, cirrhosis, liver failure, etc. Disorders of the Digestive System • Cystic fibrosis & the pancreas – Pancreatic ducts become blocked with mucus • Prevent pancreatic juices from entering sm. intest • Leads to malabsorption of fats & other nutrients • Many cancers of the GI tract The Digestive System with Age • Middle age gallstones & ulcers, also acid reflux • Old age activity of digestive organs decline – – – – Fewer digestive juices & enzymes produced Absorption is less efficient Dehydration of fecal mass leads to constipation Diverticulosis & cancer of digestive organs more common • Healthy diet/nutrition, hydration throughout life can help greatly! Questions…? What’s Next? Lab: Finish GI Tract & Start Urinary System Wed Lecture: Urinary Sys & Reprod System Wed Lab: Reprod System Leonardo Da Vinci