* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Ch22.Respiratory.System_1
Survey
Document related concepts
Transcript
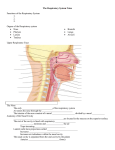
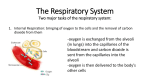
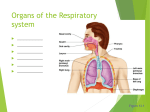
The Respiratory System Ch 22 Leonardo Da Vinci Human Anatomy Sonya Schuh-Huerta, Ph.D. The Upper Respiratory Tract Cribriform plate of ethmoid bone Frontal sinus Nasal cavity Nasal conchae (superior, middle and inferior) Sphenoid sinus Posterior nasal aperture Nasopharynx Pharyngeal tonsil Opening of pharyngotympanic tube Nasal meatuses (superior, middle, and inferior) Nasal vestibule Nostril Uvula Oropharynx Palatine tonsil Isthmus of the fauces Hard palate Soft palate Laryngopharynx Lingual tonsil Hyoid bone Esophagus Trachea Tongue Larynx Epiglottis Vestibular fold Thyroid cartilage Vocal fold Cricoid cartilage Thyroid gland Organs of the Respiratory System Nasal cavity Nostril Larynx Trachea Carina of trachea Right main (primary) bronchus Right lung Parietal pleura Oral cavity Pharynx Left main (primary) bronchus Bronchi Alveoli Left lung Diaphragm Bronchi in the Conducting Zone Superior lobe of right lung Trachea Superior lobe of left lung Left main (primary) bronchus Lobar (secondary) bronchus Segmental (tertiary) bronchus Inferior lobe of left lung Inferior lobe of right lung Middle lobe of right lung (a) The branching of the bronchial tree Structures of the Respiratory Zone Alveoli Alveolar duct Respiratory bronchioles Terminal bronchiole (a) Alveolar duct Alveolar sac Alveoli & the Respiratory Membrane Terminal bronchiole Respiratory bronchiole Smooth muscle Elastic fibers Alveolus Capillaries (a) Diagrammatic view of capillary-alveoli relationships Anatomy of Alveoli & the Respiratory Membrane Red blood cell Nucleus of type I (squamous epithelial) cell Alveolar pores Capillary O2 Macrophage Endothelial cell nucleus Alveolus Respiratory membrane Red blood cell in capillary Alveoli (gas-filled air spaces) Type I cell of alveolar wall Type II (surfactantsecreting) cell (c) Detailed anatomy of the respiratory membrane Capillary CO2 Alveolus Alveolar epithelium Fused basement membranes of the alveolar epithelium and the capillary endothelium Capillary endothelium The Respiratory System • Basic functions of the respiratory system – Supplies body with oxygen – Disposes of carbon dioxide • 4 processes involved in respiration: – Pulmonary ventilation – External respiration – Transport of respiratory gases – Internal respiration Functional Anatomy of the Respiratory System • Respiratory organs – Nose, nasal cavity, & paranasal sinuses – Pharynx, larynx, & trachea – Bronchi & smaller branches – Lungs & alveoli Organs of the Respiratory System • Divided into – Conducting zone – Respiratory zone The Nose • • • • • Provides an airway for respiration Moistens & warms air (humidifies air) Filters inhaled air Resonating chamber for speech Houses olfactory receptors (olfaction) The Nose • Size variation due to differences in nasal cartilages • Skin is thin contains many sebaceous glands Frontal bone Epicranius, frontal belly Nasal bone Root and bridge of nose Septal cartilage Maxillary bone (frontal process) Dorsum nasi Ala of nose Lateral process of septal cartilage Minor alar cartilages Apex of nose Dense fibrous connective tissue Naris (nostril) Major alar cartilages Philtrum (a) Surface anatomy (b) External skeletal framework The Nasal Cavity • External nares nostrils • Divided by nasal septum • Continuous with nasopharynx Nasal Cavity • 2 types of mucous membrane: – Olfactory mucosa • Near roof of nasal cavity • Houses olfactory receptors – Respiratory mucosa • Lines nasal cavity • Pseudostratified ciliated columnar epithelium The Upper Respiratory Tract Cribriform plate of ethmoid bone Frontal sinus Nasal cavity Nasal conchae (superior, middle and inferior) Sphenoid sinus Posterior nasal aperture Nasopharynx Pharyngeal tonsil Opening of pharyngotympanic tube Nasal meatuses (superior, middle, and inferior) Nasal vestibule Nostril Uvula Oropharynx Palatine tonsil Isthmus of the fauces Hard palate Soft palate Laryngopharynx Lingual tonsil Hyoid bone Esophagus Trachea Tongue Larynx Epiglottis Vestibular fold Thyroid cartilage Vocal fold Cricoid cartilage Thyroid gland Respiratory Mucosa • Consists of: – Pseudostratified ciliated columnar epithelium – Goblet cells within epithelium – Underlying layer of lamina propria • Cilia move contaminated mucus posteriorly Nasal Conchae • Superior & middle nasal conchae – Part of the ethmoid bone • Inferior nasal conchae – Separate bone • Project medially from the lateral wall of the nasal cavity • Particulate matter: – Deflected to mucus-coated surfaces The Pharynx • Funnel-shaped passageway • Connects nasal cavity & mouth • Divided into 3 sections by location: – Nasopharynx – Oropharynx – Laryngopharynx • Type of mucosal lining changes along its length The Nasopharynx • • • • Superior to the point where food enters Only an air passageway Closed off during swallowing Pharyngeal tonsil (adenoids) – Located on posterior wall – Destroys pathogens that enter • Contains the opening to the pharyngotympanic tube (auditory or eustachian tube) – Tubal tonsil • Provides some protection from infection The Oropharynx • Arch-like entrance-way fauces – Extends from soft palate to epiglottis • Epithelium – Stratified squamous epithelium • 2 types of tonsils in the oropharynx – Palatine tonsils in lateral walls of the fauces – Lingual tonsils covers the posterior surface of the tongue The Laryngopharynx • Passageway for both food & air • Epithelium – Stratified squamous epithelium • Continuous with the esophagus & larynx The Larynx • 3 functions – Voice production – Provides an open airway – Routes air & food into the proper channels • Superior opening (epiglotis) is: – Closed during swallowing – Open during breathing 9 Cartilages of the Larynx • Thyroid cartilage – Shield-shaped, forms laryngeal prominence (= Adam’s apple) • 3 pairs of small cartilages – Arytenoid cartilages – Corniculate cartilages – Cuneiform cartilages • Epiglottis – Tips inferiorly during swallowing The Larynx • Vocal ligaments of the larynx – Vocal folds (= true vocal cords) • Function in sound production – Vestibular folds (= false vocal cords) • No role in sound production • Epithelium of the larynx: – Stratified squamous superior portion – Pseudostratified ciliated columnar inferior portion Anatomy of the Larynx Body of hyoid bone Laryngeal prominence (Adam’s apple) Cricoid cartilage Sternal head Clavicular head Sternocleidomastoid Clavicle Jugular notch (a) Surface view Epiglottis Thyrohyoid membrane Body of hyoid bone Thyroid cartilage Laryngeal prominence (Adam’s apple) Cricothyroid ligament Cricoid cartilage Cricotracheal ligament Tracheal cartilages (b) Anterior view Anatomy of the Larynx Epiglottis Thyrohyoid membrane Hyoid bone Corniculate cartilage Thyroid cartilage Arytenoid cartilage Cricoid cartilage Glottis Tracheal cartilages (c) Photograph of cartilaginous framework of the larynx, posterior view Epiglottis Thyrohyoid membrane Body of hyoid bone Thyrohyoid membrane Cuneiform cartilage Fatty pad Corniculate cartilage Arytenoid cartilage Vestibular fold (false vocal cord) Arytenoid muscle Cricoid cartilage Thyroid cartilage Vocal fold (true vocal cord) Cricothyroid ligament Cricotracheal ligament Tracheal cartilages (d) Sagittal section (anterior on the right) Movements of the Vocal Cords Anterior Thyroid cartilage Cricoid cartilage Vocal ligaments of vocal cords Glottis Lateral cricoarytenoid muscle Arytenoid cartilage Corniculate cartilage Posterior cricoarytenoid muscle Posterior Base of tongue Epiglottis Vestibular fold (false vocal cord) Vocal fold (true vocal cord) Glottis Inner lining of trachea Cuneiform cartilage Corniculate cartilage (a) Vocal folds in closed position; closed glottis (b) Vocal folds in open position; open glottis The Larynx • Voice production – Length of the vocal folds changes with pitch – Loudness depends on the force of air across the vocal folds • Sphincter function of the larynx – Valsalva’s maneuver straining • Innervation of the larynx – Recurrent laryngeal nerves (branch of vagus) The Trachea • Descends into the mediastinum • C-shaped cartilage rings keep airway open! • Carina – Marks where trachea divides into 2 primary bronchi – Epithelium • Pseudostratified ciliated columnar epithelium ~remember this? The Trachea Mucosa Pseudostratified ciliated columnar epithelium Lamina propria (connective tissue) Submucosa Seromucous gland in submucosa Posterior Hyaline cartilage Mucosa Esophagus Trachealis muscle Submucosa Lumen of trachea Seromucous gland in submucosa Hyaline cartilage Adventitia Anterior (a) Cross section of the trachea and esophagus (b) Photomicrograph of the tracheal wall (250) Bronchi in the Conducting Zone • Bronchial tree – Extensively branching respiratory passageways • Primary bronchi (main bronchi) – Largest bronchi • Right main primary bronchi – Wider & shorter than the left – Right lung also bigger than the left Bronchi in the Conducting Zone Superior lobe of right lung Trachea Superior lobe of left lung Left main (primary) bronchus Lobar (secondary) bronchus Segmental (tertiary) bronchus Inferior lobe of left lung Inferior lobe of right lung Middle lobe of right lung (a) The branching of the bronchial tree Bronchi in the Conducting Zone • Secondary (lobar) bronchi – Three on the right – Two on the left • Tertiary (segmental) bronchi – Branch into each lung segment • Bronchioles – Little bronchi, less than 1 mm in diameter • Terminal bronchioles – Less than 0.5 mm in diameter Bronchi in the Conducting Zone Mucosa Pseudostratified epithelium Lumen Lamina propria Fibromusculocartilaginous layer Cartilage plate Smooth muscle (b) Photomicrograph of a bronchus (13) Changes in Tissue Along Conducting Pathways • Supportive connective tissues change – C-shaped rings replaced by cartilage plates • Epithelium changes – First, pseudostratified ciliated columnar – Replaced by simple columnar, then simple cuboidal epithelium • Smooth muscle becomes important: – Airways widen with sympathetic stimulation – Airways constrict with parasympathetic stim. Structures of the Respiratory Zone • Consists of air-exchanging structures • Respiratory bronchioles branch from terminal bronchioles – Lead to alveolar ducts • Lead to alveolar sacs Structures of the Respiratory Zone Alveoli Alveolar duct Respiratory bronchioles Terminal bronchiole (a) Alveolar duct Alveolar sac Structures of the Respiratory Zone Respiratory bronchiole Alveolar pores Alveolar duct Alveoli Alveolar sac (b) Structures of the Respiratory Zone • Alveoli – ~300 million alveoli account for tremendous surface area of the lungs! • Surface area of alveoli is ~140 square meters!!! • Why such a large surface area? Structures of the Respiratory Zone • Structure of alveoli – Type I cells single layer of simple squamous epithelial cells • Surrounded by basal lamina – Alveolar & capillary walls plus their basal lamina form • The Respiratory membrane Anatomy of Alveoli & the Respiratory Membrane Terminal bronchiole Respiratory bronchiole Smooth muscle Elastic fibers Alveolus Capillaries (a) Diagrammatic view of capillary-alveoli relationships Structures of the Respiratory Zone • Structures of alveoli (cont.) – Type II cells scattered among type I cells • Are cuboidal epithelial cells • Secrete surfactant (very important!) – Detergent-like molecule, that reduces surface tension within alveoli (prevents them from collapsing) – Alveolar macrophages also present Anatomy of Alveoli & the Respiratory Membrane Red blood cell Nucleus of type I (squamous epithelial) cell Alveolar pores Capillary O2 Macrophage Endothelial cell nucleus Alveolus Respiratory membrane Red blood cell in capillary Alveoli (gas-filled air spaces) Type I cell of alveolar wall Type II (surfactantsecreting) cell (c) Detailed anatomy of the respiratory membrane Capillary CO2 Alveolus Alveolar epithelium Fused basement membranes of the alveolar epithelium and the capillary endothelium Capillary endothelium The Respiratory Zone • Features of alveoli – Surrounded by elastic fibers – Interconnect by way of alveolar pores – Internal surfaces • A site for free movement of alveolar macrophages Gross Anatomy of the Lungs • Major landmarks of the lungs – Apex, base, hilum, & root • Left lung – Superior & inferior lobes • Right lung – Superior, middle, & inferior lobes Gross Anatomy of the Lungs Anterior View of Thoracic Structures Intercostal muscle Rib Lung Apex of lung Parietal pleura Pleural cavity Visceral pleura Pulmonary artery Trachea Thymus Apex of lung Left superior lobe Left superior lobe Left main bronchus Oblique fissure Oblique fissure Pulmonary vein Left inferior lobe Impression of heart Right inferior lobe Heart (in mediastinum) Hilum Oblique fissure Diaphragm Aortic impression Right superior lobe Horizontal fissure Right middle lobe Left inferior lobe Oblique fissure Base of lung Cardiac notch (a) Anterior view. The lungs flank mediastinal structures laterally. Lobules (b) Photograph of medial view of the left lung Bronchial Tree Right lung Right superior lobe (3 segments) Left lung Left superior lobe (4 segments) Right middle lobe (2 segments) Right inferior lobe (5 segments) Left inferior lobe (5 segments) Blood Supply & Innervation of the Lungs • Pulmonary arteries – Deliver oxygen-poor blood to the lungs • Pulmonary veins – Carry oxygenated blood to the heart • Innervation – Sympathetic, parasympathetic, & visceral sensory fibers • Parasympathetic constrict airways • Sympathetic dilate airways Transverse Cut Through Lungs Vertebra Right lung Parietal pleura Visceral pleura Pleural cavity Posterior Esophagus (in mediastinum) Root of lung at hilum Left main bronchus Left pulmonary artery Left pulmonary vein Left lung Thoracic wall Pulmonary trunk Pericardial membranes Sternum Heart (in mediastinum) Anterior mediastinum Anterior (d) Transverse section through the thorax, viewed from above. Lungs, pleural membranes, and major organs in the mediastinum are shown. The Pleurae (review) • A double-layered sac surrounding each lung – Parietal pleura – Visceral pleura • Pleural cavity – Potential space between the visceral & parietal pleurae • Pleurae help divide the thoracic cavity – Central mediastinum – 2 lateral pleural compartments Diagram of the Pleurae & Pleural Cavities Intercostal muscle Rib Parietal pleura Pleural cavity Visceral pleura Lung Trachea Thymus Apex of lung Left superior lobe Right superior lobe Oblique fissure Horizontal fissure Left inferior lobe Right middle lobe Oblique fissure Right inferior lobe Heart (in mediastinum) Diaphragm Base of lung Cardiac notch (a) Anterior view. The lungs flank mediastinal structures laterally. The Mechanisms of Ventilation • 2 phases of pulmonary ventilation – Inspiration inhalation – Expiration exhalation Inspiration • Volume of thoracic cavity increases – Decreases internal gas pressure – Action of the diaphragm • Diaphragm flattens – Action of intercostal muscles • Contraction raises the ribs Inspiration • Deep inspiration requires – Scalenes – Sternocleidomastoid – Pectoralis minor – Erector spinae extends the back Expiration • Quiet expiration chiefly a passive process! – Inspiratory muscles relax – Diaphragm moves superiorly – Volume of thoracic cavity decreases • Forced expiration an active process – Produced by contraction of • Internal & external oblique muscles • Transverse abdominis muscles Changes in Thoracic Volume (a) Inspiration Diaphragm and intercostal muscles contract (diaphragm descends and rib cage rises). Thoracic cavity volume increases. Changes in superiorinferior and anteriorposterior dimensions Ribs are elevated and sternum flares as external intercostals contract. Diaphragm moves inferiorly during contraction. Changes in lateral dimensions (superior view) External intercostals contract. (b) Expiration Inspiratory muscles relax (diaphragm rises and rib cage descends due to recoil of the costal cartilages). Thoracic cavity volume decreases. Ribs and sternum are depressed as external intercostals relax. Diaphragm moves superiorly as it relaxes. External intercostals relax. Changes in Thoracic Volume 1 At rest, no air movement: Air pressure in lungs is equal to atmospheric (air) pressure. Pressure in the pleural cavity is less than pressure in the lungs. This pressure difference keeps the lungs inflated. Trachea Main bronchi Thoracic wall Pleural cavity Lung Lung 3 Expiration: Inspiratory muscles relax, reducing thoracic volume, and the lungs recoil. Simultaneously, volumes of the pleural cavity and the lungs decrease, causing pressure to increase in the lungs, and air flows out. Resting state is reestablished. Pleural Thoracic cavity wall Diaphragm Air 2 Inspiration: Inspiratory muscles contract and increase the volume of the thoracic and pleural cavities. Pleural fluid in the pleural cavity holds the parietal and visceral pleura close together, causing the lungs to expand. As volume increases, pressure decreases and air flows into the lungs. Parietal pleura Visceral pleura At rest V P Expanded V P Air flows in Air V P Air flows out V P Neural Control of Ventilation • Respiratory center – Generates baseline respiration rate – In the reticular formation of the medulla oblongata • Chemoreceptors – Sensitive to rising & falling oxygen levels – Central chemoreceptors located in medulla – Peripheral chemoreceptors • Aortic bodies • Carotid bodies Location of Peripheral Chemoreceptors Brain Sensory nerve fiber in cranial nerve IX (pharyngeal branch of glossopharyngeal) External carotid artery Internal carotid artery Carotid body Common carotid artery Cranial nerve X (vagus nerve) Sensory nerve fiber in cranial nerve X Aortic bodies in aortic arch Aorta Heart Disorders of Lower Respiratory Structures • Bronchial asthma – A type of allergic inflammation • Hypersensitivity to irritants in the air or to stress – Asthma attacks characterized by • Contraction of bronchiole smooth muscle • Secretion of mucus in airways Disorders of Lower Respiratory Structures • Cystic fibrosis (CF) inherited disease – Exocrine gland function is disrupted – Respiratory system affected by • Oversecretion of viscous mucus • Pneumonia infectious disease – Accumulation of fluid in alveoli – Interferes with gas exchange (drowning) Disorders of Lower Respiratory Structures • Chronic obstructive pulmonary disease (COPD) – Airflow into & out of the lungs is difficult • Obstructive emphysema • Chronic bronchitis – History of smoking usually associated Disorders of Lower Respiratory Structures Figure 22.18 Alveolar Changes with Emphysema Figure 22.19 Lung Cancer • Most common cause of cancer-related death! – 1.3 million deaths/year worldwide – Treated by surgery, radiation, and/or chemotherapy – Symptoms shortness of breath, coughing (up blood), weight loss – History of smoking or 2ndhand smoke usually associated – 14% survival rates Aging of the Respiratory System • The number of glands in nasal mucosa declines • Nose dries – Produces thickened mucus • Thoracic wall becomes more rigid • Lungs lose elasticity • Oxygen levels in the blood may fall • Again…Exercise throughout life is important for respiratory health! Questions…? What’s Next? Tonight’s Lab: Lab Exam 4! Wed Lecture: Lecture Exam 4! Wed Lab: Start Digestive System