* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Human microbiota wikipedia , lookup
Adjustable gastric band wikipedia , lookup
Hepatotoxicity wikipedia , lookup
Cholangiocarcinoma wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Intestine transplantation wikipedia , lookup
Bariatric surgery wikipedia , lookup
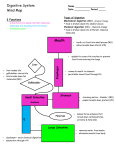
Ch. 25: The Digestive System Medical treatment = gastroenterology. I. General Anatomy and Processes (A) Digestive Functions -1- ingestion -2- digestion: mechanical and chemical (enzymes) -3- absorption, into blood or lymph -4- defecation (B) General Anatomy – Digestive tract (most = GIT: gastrointestinal) and accessory organs. Wall with mucosa, submucosa, muscularis, serosa. Enteric nervous system regulates motility, secretions and blood flow. Parasympathetic. (C) Peritoneum – forms extensions = mesenteries and omenta (lesser and greater). (D) Regulation – neural, hormonal, paracrine. II. Mouth through esophagus (A) Mouth = buccal cavity. Ingests, tastes, masticates (chews), chemically digests (starch), deglutinates (swallows) food; speech, respiration. -1- cheeks and lips: mastication, speech. -2- tongue: lingual papillae with taste buds. Muscular, with glands. -3- palate: hard, soft, uvula (seals nasopharynx during swallow). -4- teeth: incisors, canines, premolars, molars. First deciduous, then adult. Connected to alveolar sockets by periodontal ligaments, covered by gingiva. Crown and root. Dentin covered by enamel, cementum. Pulp cavity in crown extends into root canal. (B) Mastication begins mechanical digestion. (C) Saliva – moistens, for starch and fat digestion, cleanses, inhibits bacteria, forms bolus. Contains water, salivary amylase, lingual lipase, mucus, lysozyme, IgA, electrolytes. pH 6.8-7.0. Produced from intrinsic and extrinsic glands: parotids (infected in mumps), submandibular and sublingual. 1.0 – 1.5 L/ day. 34 (D) Pharynx – swallow initiated. (E) Esophagus – 25 – 30 cm long. (F) Swallowing = deglutition. More than 22 muscles involved. Coordinated by medulla and pons. Continues into peristalsis. III. Stomach Mostly for food storage. May hold up to 4 L. Mechanical digestion, some chemical. Creates chyme. (A) Gross Anatomy: lesser and greater curvatures. Regions: cardiac, fundic, body, pyloric (with sphincter). Parasympathetic (vagus) and sympathetic innervation. (B) Wall – lined with rugae. Ample mucus. Pits lead into glands. Cell types: mucous, stem, parietal (HCl, intrinsic factor), chief (pepsinogen), enteroendocrine (hormones and paracrine secretions). (C) Gastric Secretions 2-3 L gastric juice/ day. -1- HCl: created in gastric lumen. Chloride shift exchanges bicarbonate for Cl-, leads to alkaline tide in blood. Low pH activates enzymes, liquefies food, transforms iron for better absorption, antimicrobial. -2- pepsin: from pepsinogen and HCl. Infants have gastric lipase and chymosin (= rennin). -3- intrinsic factor: for vitamin B12 absorption. -4- chemical messengers: approximately 20. Most are hormones. (D) Gastric Motility – chyme squirted in small amounts to small intestine. Average time in stomach four hours, more with fatty meal. (E) Vomiting – due to extensive stretching, psychological stimuli, irritants and toxins. Medullary emetic center. (F) Digestion & Absorption – very little digestion. Some drug absorption. 35 (G) Protection – thick mucus, rapid epithelial cell replacement, tight junctions. Failure results in peptic ulcers: most due to H. pylori bacteria (in small intestine). (H) Regulation – in phases -1- cephalic: stimulated by sights, sounds, smells. -2- gastric: after ingestion. Protein most stimulatory. -3- intestinal: results from duodenal response. Inhibitory. IV. Liver, Gallbladder, Pancreas All connect to small intestine. (A) Liver – largest gland. Most functions not digestive. -1- gross anatomy: four lobes, surface ligaments. -2- microscopic anatomy: hepatic lobules with central veins. Surrounded by hepatocytes. Peripheral hepatic arteries, portal veins connected via sinusoids to central vein, and bile ductules. -3- functions a. general – removes glucose, amino acids, iron and vitamins for processing and storage. Removes and degrades hormones, toxins, drugs, bile pigments. Secretes albumin, lipoproteins, clotting factors. Macrophages = Kupffer cells. b. digestive – releases bile into canaliculi, to common hepatic duct, joins cystic duct (from gallbladder) to bile duct to duodenum. Regulated by sphincter of Oddi. (B) Gallbladder and Bile Gallbladder stores and concentrates bile- contains minerals, cholesterol, bile pigments (mostly bilirubin) from Hb breakdown, bile acids (salts). Bilirubin coverts to urobilinogen (brown) in large intestine. Much of bile reabsorbed from small intestine –recycled. Gallstones may result from excessive cholesterol. (C) Pancreas 1200 – 1500 ml pancreatic juice/ day. Exocrine portion = acini, lead to pancreatic duct to duodenum. Near bile duct, regulated together. Pancreatic juice with water, enzymes (amylase, lipase, nucleases), sodium bicarbonate, electrolytes; alkaline. 36 (D) Regulation of Secretion – vagal stimulation, also stimulated by CCK, gastrin, secretin. CCK promotes gallbladder contraction, secretion of pancreatic enzymes, relaxes sphincter of Oddi. Gastrin stimulates gallbladder contraction and pancreatic secretions. Secretin promotes bicarbonate secretion. V. Small Intestine Most chemical digestion and absorption. ~2 meters long. Average diameter 2.5 cm. (A) Gross Anatomy - duodenum, jejunum, ileum, ileocecal junction with valve. (B) Microscopic Anatomy – circular folds = plicae circularis, lined with villi and microvilli. Absorptive and goblet cells. Villi contain capillaries and lacteals. Microvilli form brush border, contains enzymes. Brunners Glands create bicarbonate-rich mucus; Peyer Patches with lymph nodules. (C) Intestinal Motility – segmentation and peristalsis. VI. Chemical Digestion and Absorption (A) Carbohydrates – Most is starch and glycogen (minimal) convert to maltose, then glucose. Absorbed by SGLT: sodium-glucose transport protein. Lactose intolerance common. (B) Proteins digested to amino acids, absorbed via sodium-dependent cotransporters (like glucose). (C) Lipids more complicated. Bile creates emulsification droplets, convert to micelles (coated with bile acids), then chylomicrons in intestinal cells, absorbed into lymph. 37 (D) Other e.g. RNA, DNA. Vitamins and minerals require no digestion. Water reabsorption varies, diarrhea vs. constipation. VII. Large Intestine (A) Gross Anatomy – cecum with appendix, colon: ascending, transverse, descending, sigmoid, rectum and anus (lined with hemorrhoidal veins). Longitudinal teniae coli create pouches = haustra. Internal and external (skeletal muscle) anal sphincters. (B) Microscopic Anatomy – simple columnar epithelium. Intestinal crypts for abundant mucus production. Site of bacterial flors, mostly E. coli: process undigested carbohydrates, release Vitamins (Bs and K). (C) Physiology Water and electrolyte absorption. Feces with 75% water, bacteria, fiber, fat, cells, mucus, secretions. Haustral contractions (segementation) and mass movements. 38