* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Intravenous magnesium for cardiac arrhythmias: jack of all trades
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Electrocardiography wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
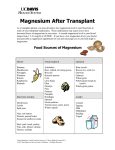
Magnesium Research 2008; 21 (1): 65-8 RECENT ADVANCES AND OPINIONS IN MAGNESIUM RESEARCH Intravenous magnesium for cardiac arrhythmias: jack of all trades Kwok-Ming Ho Department of Intensive Care, Royal Perth Hospital, Perth, Australia Copyright © 2017 John Libbey Eurotext. Téléchargé par un robot venant de 88.99.165.207 le 06/05/2017. Correspondence: K.-M. Ho, Department of Intensive Care, Royal Perth Hospital, Perth, WA 6000, Australia <[email protected]> Abstract. Intravenous magnesium has been used to prevent and treat many different types of cardiac arrhythmia. It has diverse electrophysiological actions on the conduction system of the heart; including prolonging sinus node recovery time, and reducing automaticity, atrioventricular nodal conduction, antegrade and retrograde conduction over an accessory pathway, and His-ventricular conduction. Intravenous magnesium can also homogenise transmural ventricular repolarisation. Because of its unique and diverse electrophysiological actions, intravenous magnesium has been reported to be useful in preventing atrial fibrillation and ventricular arrhythmias after cardiac and thoracic surgery; in reducing the ventricular response in acute onset atrial fibrillation, including for patients with Wolff-Parkinson-White syndrome; in the treatment of digoxin induced supraventricular and ventricular arrhythmias, multifocal atrial tachycardia, and polymorphic ventricular tachycardia or ventricular fibrillation from drug overdoses. Intravenous magnesium is, however, not useful in monomorphic ventricular tachycardia and shock-resistant ventricular fibrillation. Large randomised controlled studies are needed to confirm whether intravenous magnesium can improve patient centre outcomes in different cardiac arrhythmias. doi: 10.1684/mrh.2008.0130 Key words: antiarrhythmics, atrial fibrillation, rhythm control Magnesium has many significant physiological and pharmacological effects on different organ systems. Intravenous magnesium has a high therapeutic to toxic ratio and minimal negative inotropic effect [1], and as such, it has been used in the prevention and treatment of many different types of cardiac arrhythmia. Cardiac arrhythmia is, however, a common presentation of a diverse spectrum of diseases. Even within the same class of arrhythmia, such as atrial fibrillation or ventricular tachycardia, it can still be caused by different arrhythmogenic mechanisms from different underlying diseases. It is, therefore, unrealistic to expect intravenous magnesium to be useful in preventing or treating all types of cardiac arrhythmias. Furthermore, animal studies have shown that both the pro-arrhythmic effects of hypomagnesaemia and the anti-arrhythmic effects of magnesium depend on the underlying causes of the arrhythmia and the condition of the heart [2-4]. This review aims to briefly summarise the electrophysiological effects of intravenous magnesium and its effects on different types of cardiac arrhythmia. While intravenous magnesium chloride may have different actions from magnesium sulphate [5], magnesium sulphate is the most widely available intravenous preparation and almost exclusively used in many of the studies cited in this review. Electrophysiological effects of intravenous magnesium Intravenous magnesium has been shown to have a number of electrophysiological actions on the conduction system of the heart. The mechanism of its actions may include calcium antagonism at the L- and T-type calcium channels [6], regulation of energy transfer, and in supraphysiological doses, magnesium decreases the outward potassium current density resulting in membrane stabilisation and it also acts as an indirect antagonist of digoxin at the sarcolemma Na(+)-K(+)-ATPase pump [7, 8]. 65 K.-M. HO Copyright © 2017 John Libbey Eurotext. Téléchargé par un robot venant de 88.99.165.207 le 06/05/2017. In the supraventricular conduction pathway, magnesium can reduce automaticity [9], increase sinus node recovery time (at high doses) [10], and reduce atrioventricular nodal conduction without affecting atrial-atrial conduction [11]. Magnesium can also block the antegrade and retrograde conduction over an accessory pathway [12-14], and has a dominant effect on the slow atrioventricular nodal (AVN) pathway in patients with dual AVN physiology [15]. In the ventricular conduction pathway, magnesium suppresses prematurely triggered activity, prolongs the His-ventricular conduction [16], and homoge- nises transmural ventricular repolarisation [4, 17] without affecting autonomic nervous activity [18]. Homogenisation of ventricular repolarisation is believed to explain the anti-arrhythmic effect of magnesium in prolonged QT syndrome [17]. Magnesium appears to have no effect on excitable gap arrhythmias associated with a fixed anatomic substrate (e.g. monomorphic ventricular tachycardia) [4, 19]. Table 1. Possible indications for intravenous magnesium as an anti-arrhythmic agent. Rhythm and clinical condition Atrial fibrillation (AF) - Prevention in cardiac and thoracic surgery - Treatment of chronic AF - Digoxin toxicity with Wolff-Parkinson-White syndrome - Treatment of acute onsetAF Benefits Reference Reduces the incidence of AF Reduces rapid ventricular response Reduces rapid ventricular response [20, 21] [8] [14, 23] Reduces rapid ventricular response Improves conversion to sinus rhythm and reduces the incidence of torsades de points polymorphic ventricular tachycardia when used with ibutilide [22, 24, 25] Multifocal atrial tachycardia Reduces rapid ventricular response and converts some patients to sinus rhythm [26] Paroxysmal supraventricular tachycardia Converts to sinus rhythm (less effective than [12, 27, 28] adenosine but may help if no response to adenosine) Ventricular premature complexes - Prevention in cardiac surgery - Treatment in heart failure patients with hypomagnesaemia Ventricular tachycardia (VT) - Digoxin toxicity - Class Ic anti-arrhythmic toxicity (e.g. pilsicainide) Polymorphic VT (torsades de pointes) - Prolonged QT (congenital and acquired) (e.g. haloperidol, amiodarone) Ventricular fibrillation (VF) Amitriptyline poisoning Intravenous magnesium was reported to be not useful in the following conditions Community cardiac arrest with shock-resistant VF Monomorphic VT 66 Reduces the incidence Reduces the incidence [29, 30] [31] Converts to stable junctional rhythm Converts to sinus rhythm [32] [33] Converts to sinus rhythm [34-36] Converts to sinus rhythm [37] [38, 39] [4, 19] INTRAVENOUS MAGNESIUM FOR CARDIAC ARRHYTHMIAS: JACK OF ALL TRADES Copyright © 2017 John Libbey Eurotext. Téléchargé par un robot venant de 88.99.165.207 le 06/05/2017. Effects of intravenous magnesium on different types of cardiac arrhythmia Due to its unique but diverse electrophysiological effects, intravenous magnesium has been reported to be effective in the prevention and treatment of a variety of cardiac arrhythmias (table 1). Intravenous magnesium is useful in preventing atrial fibrillation and ventricular arrhythmias after cardiac and thoracic surgery [20, 21], reducing the ventricular response in acute onset atrial fibrillation [22] (including in patients with Wolff-ParkinsonWhite syndrome [23]), improving rhythm control with ibutilide [24, 25], treatment of digoxin induced supraventricular and ventricular arrhythmias, multifocal atrial tachycardia [26], polymorphic ventricular tachycardia with a prolonged QT interval, and ventricular fibrillation from amitriptyline overdoses. Intravenous magnesium can also be considered as a second line drug in the treatment of supraventricular tachycardia when adenosine is not effective [27]. Intravenous magnesium is, however, not useful in monomorphic ventricular tachycardia and shockresistant ventricular fibrillation. Apart from being effective in controlling many cardiac arrhythmias, intravenous magnesium also has less significant detrimental haemodynamic effects on the cardiovascular system compared to other anti-arrhythmic agents, including amiodarone or calcium channel blockers; although minor symptoms of flushing, tingling, and dizziness are common after intravenous magnesium [22]. Evidence that supports the use of intravenous magnesium in many different types of cardiac arrhythmias is, however, based on case reports, animal studies, and randomised controlled studies that evaluated physiological endpoints only [20, 22]. None of the published randomised controlled studies on intravenous magnesium have demonstrated a significant reduction in mortality. Conclusion Intravenous magnesium appears to be useful in the prevention and treatment of a variety of cardiac arrhythmias. It is, however, not useful in monomorphic ventricular tachycardia and shock-resistant ventricular fibrillation. We must also be aware that the successful prevention or treatment of cardiac arrhythmias is only, at best, a surrogate end-point of effectiveness. Large randomised controlled studies are needed to confirm whether intravenous magnesium can improve patient centre outcomes in different cardiac arrhythmias. References 1. Crippa G, Sverzellati E, Giorgi-Pierfranceschi M, Carrara GC. Magnesium and cardiovascular drugs: interactions and therapeutic role. Ann Ital Med Int 1999; 14: 40-5. 2. Aupetit JF, Freysz M, Faucon G, Loufoua-Moundanga J, Coquelin H, Timour Q. Magnesium--a profibrillatory or antifibrillatory drug depending on plasma concentration, heart rate and myocardial perfusion. Acta Anaesthesiol Scand 1997; 41: 516-23. 3. Evans SJ, Levi AJ, Jones JV. Low magnesium enhances the pro-arrhythmic effect of low potassium in the hypertrophied rat heart but not in the normal rat heart. J Hypertens 1996; 14: 635-44. 4. Haigney MC, Berger R, Schulman S, Gerstenblith G, Tunin C, Silver B, Silverman HS, Tomaselli G, Calkins H. Tissue magnesium levels and the arrhythmic substrate in humans. J Cardiovasc Electrophysiol 1997; 8: 980-6. 5. Durlach J, Guiet-Bara A, Pagès N, Bac P, Bara M. Magnesium chloride or magnesium sulfate: a genuine question. Magnes Res 2005; 18: 187-92. 6. Wu JY, Lipsius SL. Effects of extracellular Mg2+ on T- and L-type Ca2+ currents in single atrial myocytes. Am J Physiol 1990; 259: 1842-50. 7. Fawcett WJ, Haxby EJ, Male DA. Magnesium: physiology and pharmacology. Br J Anaesth 1999; 83: 302-20. 8. Ingemansson MP, Smideberg B, Olsson SB. Intravenous MgSO4 alone and in combination with glucose, insulin and potassium (GIK) prolong the atrial cycle length in chronic atrial fibrillation. Europace 2000; 2: 106-14. 9. Iseri LT, Allen BJ, Ginkel ML, Brodsky MA. Ionic biology and ionic medicine in cardiac arrhythmias with particular reference to magnesium. Am Heart J 1992; 123: 1404-9. 10. DiCarlo Jr. LA, Morady F, de Buitleir M, Krol RB, Schurig L, Annesley TM. Effects of magnesium sulfate on cardiac conduction and refractoriness in humans. J Am Coll Cardiol 1986; 7: 1356-62. 11. Rasmussen HS, Larsen OG, Meier K, Larsen J. Hemodynamic effects of intravenously administered magnesium on patients with ischemic heart disease. Clin Cardiol 1988; 11: 824-8. 12. Christiansen EH, Frost L, Andreasen F, Mortensen P, Thomsen PE, Pedersen AK. Dose-related cardiac electrophysiological effects of intravenous magnesium. A double-blind placebo-controlled dose-response study in patients with paroxysmal supraventricular tachycardia. Europace 2000; 2: 320-6. 13. Viskin S, Belhassen B, Sheps D, Laniado S. Clinical and electrophysiologic effects of magnesium sulfate on paroxysmal supraventricular tachycardia and comparison with adenosine triphosphate. Am J Cardiol 1992; 70: 879-85. 14. Sideris AM, Galiatsu E, Filippatos GS, Kappos K, Anthopoulos LP. Effects of magnesium and potassium on Wolff-Parkinson-White syndrome. J Electrocardiol 1996; 29: 11-5. 67 K.-M. HO 15. Stiles MK, Sanders P, Disney P, Brooks A, John B, Lau DH, Shashidhar, Wilson L, Mackenzie L, Young GD. Differential effects of intravenous magnesium on atrioventricular node conduction in supraventricular tachycardia. Am J Cardiol 2007; 100: 1249-53. Copyright © 2017 John Libbey Eurotext. Téléchargé par un robot venant de 88.99.165.207 le 06/05/2017. 16. Satoh Y, Sugiyama A, Tamura K, Hashimoto K. Effect of magnesium sulfate on the haloperidol-induced QT prolongation assessed in the canine in vivo model under the monitoring of monophasic action potential. Jpn Circ J 2000; 64: 445-51. 17. Chinushi M, Sugiura H, Komura S, Hirono T, Izumi D, Tagawa M, Furushima H, Aizawa Y. Effects of intravenous magnesium in a prolonged QT interval model of polymorphic ventricular tachycardia focus on transmural ventricular repolarization. Pacing Clin Electrophysiol 2005; 28: 844-50. 18. Chinushi M, Izumi D, Komura S, Ahara S, Satoh A, Furushima H, Washizuka T, Aizawa Y. Role of autonomic nervous activity in the antiarrhythmic effects of magnesium sulfate in a canine model of polymorphic ventricular tachyarrhythmia associated with prolonged QT interval. J Cardiovasc Pharmacol 2006; 48: 121-7. 19. Farouque HM, Sanders P, Young GD. Intravenous magnesium sulfate for acute termination of sustained monomorphic ventricular tachycardia associated with coronary artery disease. Am J Cardiol 2000; 86: 1270-2. 20. Miller S, Crystal E, Garfinkle M, Lau C, Lashevsky I, Connolly SJ. Effects of magnesium on atrial fibrillation after cardiac surgery: a meta-analysis. Heart 2005; 91: 618-23. 21. Sedrakyan A, Treasure T, Browne J, Krumholz H, Sharpin C, van der Meulen J. Pharmacologic prophylaxis for postoperative atrial tachyarrhythmia in general thoracic surgery: evidence from randomized clinical trials. J Thorac Cardiovasc Surg 2005; 129: 997-1005. 22. Ho KM, Sheridan DJ, Paterson T. Use of intravenous magnesium to treat acute onset atrial fibrillation: a meta-analysis. Heart 2007; 93: 1433-40. 23. Merrill JJ, DeWeese G, Wharton JM. Magnesium reversal of digoxin-facilitated ventricular rate during atrial fibrillation in the Wolff-Parkinson-White syndrome. Am J Med 1994; 97: 25-8. 24. Kalus JS, Spencer AP, Tsikouris JP, Chung JO, Kenyon KW, Ziska M, Kluger J, White CM. Impact of prophylactic i.v. magnesium on the efficacy of ibutilide for conversion of atrial fibrillation or flutter. Am J Health Syst Pharm 2003; 60: 2308-12. 25. Tercius AJ, Kluger J, Coleman CI, White CM. Intravenous magnesium sulfate enhances the ability of intravenous ibutilide to successfully convert atrial fibrillation or flutter. Pacing Clin Electrophysiol 2007; 30: 1331-5. 26. McCord JK, Borzak S, Davis T, Gheorghiade M. Usefulness of intravenous magnesium for multifocal atrial 68 tachycardia in patients with chronic obstructive pulmonary disease. Am J Cardiol 1998; 81: 91-3. 27. LeDuc TJ, Carr JD. Magnesium sulfate for conversion of supraventricular tachycardia refractory to intravenous adenosine. Ann Emerg Med 1996; 27: 375-8. 28. Wesley Jr. RC, Haines DE, Lerman BB, DiMarco JP, Crampton RS. Effect of intravenous magnesium sulfate on supraventricular tachycardia. Am J Cardiol 1989; 63: 1129-31. 29. England MR, Gordon G, Salem M, Chernow B. Magnesium administration and dysrhythmias after cardiac surgery. A placebo-controlled, double-blind, randomized trial. JAMA 1992; 268: 2395-402. 30. Parikka H, Toivonen L, Verkkala K, Järvinen A, Nieminen MS. Ventricular Arrhythmia Suppression by Magnesium Treatment after Coronary Artery Bypass Surgery. Int J Angiol 1999; 8: 165-70. 31. Ceremuzyński L, Gebalska J, Wolk R, Makowska E. Hypomagnesemia in heart failure with ventricular arrhythmias. Beneficial effects of magnesium supplementation. J Intern Med 2000; 247: 78-86. 32. Kinlay S, Buckley NA. Magnesium sulfate in the treatment of ventricular arrhythmias due to digoxin toxicity. J Toxicol Clin Toxicol 1995; 33: 55-9. 33. Nakata K, Moriwaki R, Yamaguchi A, Takenouchi S, Mato T, Tsutsumi H. Case in which magnesium sulfate effectively treated ventricular tachycardia due to overdose of pilsicainide hydrochloride. Chudoku Kenkyu 2006; 19: 49-53. 34. Gupta A, Lawrence AT, Krishnan K, Kavinsky CJ, Trohman RG. Current concepts in the mechanisms and management of drug-induced QT prolongation and torsade de pointes. Am Heart J 2007; 153: 891-9. 35. Winters SL, Sachs RG, Curwin JH. Nonsustained polymorphous ventricular tachycardia during amiodarone therapy for atrial fibrillation complicating cardiomyopathy. Management with intravenous magnesium sulfate. Chest 1997; 111: 1454-7. 36. Sarisoy O, Babaoglu K, Tugay S, Barn E, Gokalp AS. Efficacy of magnesium sulfate for treatment of ventricular tachycardia in amitriptyline intoxication. Pediatr Emerg Care 2007; 23: 646-8. 37. Knudsen K, Abrahamsson J. Magnesium sulphate in the treatment of ventricular fibrillation in amitriptyline poisoning. Eur Heart J 1997; 18: 881-2. 38. Allegra J, Lavery R, Cody R, Birnbaum G, Brennan J, Hartman A, Horowitz M, Nashed A, Yablonski M. Magnesium sulfate in the treatment of refractory ventricular fibrillation in the prehospital setting. Resuscitation 2001; 49: 245-9. 39. Hassan TB, Jagger C, Barnett DB. A randomised trial to investigate the efficacy of magnesium sulphate for refractory ventricular fibrillation. Emerg Med J 2002; 19: 57-62.