* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Part 1 - OoCities
Drug design wikipedia , lookup
Lipid signaling wikipedia , lookup
Citric acid cycle wikipedia , lookup
Biosynthesis wikipedia , lookup
Peptide synthesis wikipedia , lookup
Biochemistry wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Specialized pro-resolving mediators wikipedia , lookup
15-Hydroxyeicosatetraenoic acid wikipedia , lookup
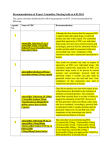
Group T Case Study #2, Part I CASE STUDY #2 GROUP T - PART I November 15, 2001 Group Members: James Morton Minhchau Nguyen Mariela Passarelli Shaun Riley Urhoy Tarzi Nhi Tran Hoa Vu Page 1 of 6 Group T Case Study #2, Part I Physicochemical Properties of Amoxicillin and Clavulanic Acid We have chosen amoxicillin as our -lactam antibiotic and clavulanic acid as our -lactamase inhibitor. The amoxicillin molecular formula is C16H19N3O5S and the molecular weight is 365.14. Chemically, amoxicillin is (2S,5R,6R)-6-[(R)-(-)-2-(p-hydroxyphenyl)acetamido]-3,3dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid. The clavulanic acid molecular formula is C8H9NO5 and the molecular weight is 199.16. Chemically, clavulanic acid is (Z)-(2R,5R)-3-(2-hydroxyethylidene)-7-oxo-4-oxa-1-azabicyclo[3.2.0]-heptane-2-carboxylate. Amoxicillin and clavulanic acid may be represented structurally as: HO HO O O OH O O H H N N NH2 N S H H H O O HO Clavulanic Acid Amoxicillin Amoxicillin contains the following six functional groups: phenol amine amide O HO -lactam HO O N N H NH2 carboxylic acid thiozole ring N O S Clavulanic acid contains the following four functional groups: ene primary alcohol -lactam carboxylic acid OH O N HO O Amoxicillin has three ionizable groups. Hammet-Taft calculations were performed to estimate the pKas of these groups. Our results were then compared with experimentally derived values (ref. 1). Table 1 below compares these values. Table 1: pKas of Amoxicillin Ionizable Functional Groups Ionizable Functional Groups Carboxylic Acid Amine Phenol Hammet-Taft Experimental 2.7 6.6 9.9 2.87 7.28 9.65 The calculated pKa (Hammet-Taft) for the carboxylic acid group of clavulanic acid is 3.9. Development of Resistance to -Lactam Antibiotics (ref. 2-5) The classification of -lactam antibiotics includes penicillin derivatives such as amoxicillin, which is found in the prescription drug Augmentin. These antibiotics inhibit bacterial enzymes Page 2 of 6 Group T Case Study #2, Part I known as penicillin-binding-proteins (PBP), which synthesize the bacterial cell wall layer. A great problem encountered through the years is antibiotic resistance. One of the major causes is the production of -lactamases by bacteria, which inactivate the administered antibiotic by the hydrolysis of the amide bond in the -lactam ring of the drug, thereby, creating resistance to the antibiotic. -lactamases can be plasmid or chromosomally mediated. Several details, such as the amount of -lactamase produced, the rate of breakdown of the antibiotic, and the affinity of lactamases for the drug, influences the mechanism of inactivation. Also, there could be problems penetrating the bacterial wall. Lipopolysaccharides and porin proteins such as OmpF which make up the membrane, undergo alterations and reduce the permeability of the drug, this leads to an increase in resistance with an increase in the expression of -lactamases and their efflux, having a greater effect on antibiotic resistance all together. Sometimes, the PBPs present on the outer membrane of the bacteria have a decreased affinity for the drug. This may be due to an increase in the quantity of PBPs, the presence of resistant to PBPs, or just the low affinity for PBPs. Antibiotic resistance has been known to be occurring for billions of years, this is what has led to the development of more specific antibiotics and man-made derivatives of already known antibiotics. With the help and education of health care providers as well as patients we can fight this problem by prescribing antibiotics only when needed and in moderation. Properties Affecting Drug Absorption in the Gastrointestinal Tract Solubility Plots of solubility versus pH for both amoxicillin and clavulanic acid were generated by ACD/Aqueous Solubility (v5.0) and obtained using the ACD/I-Lab service. To estimate the pH dependence of solubility, melting points of the drugs were required. The melting point (mp) of amoxicillin was found in literature to be 212˚C (ref. 6), while for clavulanic acid the mp is 165.0˚C (ref. 7). Plots of the resulting solubility data at 25˚C are in Figure 1 and Figure 2. FIGURE 2 CLAVULANIC ACID Solubility at Differnet pHs 900 1300 800 1200 700 1100 600 1000 Solubility (g/L) Solubility (g/L) FIGURE 1 AMOXICILLIN Solubility at Different pHs 500 400 900 800 300 700 200 600 100 500 400 0 0 2 4 6 8 10 12 14 0 2 4 6 8 10 12 pH pH For clavulanic acid (Fig. 2), the solubility greatly increases when its carboxylic acid group becomes ionized (pKa = 3.9, Hammet-Taft calculation). Note that even when clavulanic acid is predominately uncharged (pH < 1), it is still intrinsically soluble (438 g/L). For amoxicillin at Page 3 of 6 14 Group T Case Study #2, Part I pH less than 9 , the ionic charges of the carboxylic acid (negative, pKa = 2.87) and the amine (positive, pKa = 7.28) will counteract each other (i.e., zwitterion ion effect), causing the antibiotic to be less soluble. At pH 9 and higher, the effect of the negative charge of the carboxylic acid can predominate since the amine will mostly be deprotonated and uncharged. Additionally, at pH 11, amoxicillin’s phenol will become predominately ionized, yielding yet more negative charge, adding to the solubility of amoxicillin. Rate of Solution Figures 1 and 2 demonstrate that the solubility of amoxicillin in pHs corresponding to the stomach (pH 1 – 2) and small intestine (pH 6 – 7) is quite low (< 1 g/L). On the other hand, clavulanic acid, at these same pHs, is quite soluble (> 438 g/L), especially at pHs > 3 (solubilty > 1150 g/L). Because of the low solubility of amoxicillin, it will intrinsically have a low rate of solution. According to Saismaa, et. al. (ref. 8), the dissolution rate constant of amoxicillin trihydrate was experimentally found to be 1 x 10-6 mol*cm2/minute at 37C and pH 6 (intestinal conditions). In contrast, clavulanic acid at the similar physiological conditions will have a higher rate of solution due to a significantly higher solubility (see Figure 2). Therefore, the ratelimiting step of the absorption of amoxicillin in the GI tract is its dissolution, while the ratelimiting step for clavulanic acid in its absorption into plasma membrane. It is also known that, in part, the rate of solution can be influenced by the particle size before dissolution begins; the smaller the particle size, the faster the rate of solution due to the increased amount of drug exposed to the diluent (i.e., much larger surface area). Degradation Properties Since amoxicillin and clavulanic acid are both -lactams, they are susceptible to acid- and basecatalyzed hydrolysis of the four-membered -lactam ring. According to Zia (ref. 1), amoxicillin’s maximum stability has been measured at 35C to be at pH 5.77, with a rate constant of 55 hours-1. It is noted that amoxicillin is more stable at lower pH conditions because at these pHs the amine group is protonated, thereby utilizing the free electron pair of the nitrogen. When the amine is deprotonated at higher pH (pH > 8), a pair of free electrons is available for nucleophilic attack of the cyclic amide (-lactam) and generates a tri-cyclic compound identified in an article by Bundgaard (ref. 9): HO O NH HN S N H COOH Partition Coefficients The Syracuse Research Corporation (SRC) has produced a program on their website (esc.syrres.com) that calculates log P (or log Ko/w). Log P results were obtained for the compounds in Table 1 by entering the indicated CAS RN. It is apparent that uncharged amoxicillin, P = 9.33 (i.e., 9.33 times more likely to be in hydrophobic environment than in water), is quite soluble is hydrophobic media such as the Page 4 of 6 Group T Case Study #2, Part I plasma membrane of intestinal epithelial cells. This calculated result is the intrinsic partition coefficient, which does not account for ionic charges arising from ionization of the carboxylic acid, amine and phenol groups. On the other hand, clavulanic acid yields P = 0.00912, which indicates that intrinsically it is not lipophilic (i.e., will not dissolve well in hydrophobic environments). Table 2: Estimated Partition Coefficients Drug Amoxicillin Clavulanic Acid Ampicillin Ampicillin Sodium Penicillin G Sodium CAS RN 26787-78-0 (1) 58001-44-8 69-53-4 69-52-3 69-57-8 Log P 0.97 (2) -2.04 (3) 1.45 -3.41 -3.01 P 9.33 9.12 x 10-3 28.2 3.89 x 10-4 9.77 x 10-4 (1) Another CAS RN for amoxicillin, 61336-70-7, yields the same Log P results. (2) An experimental amoxicillin result, log P = 0.87 (P = 7.41), was identified in Sangster, 1994 by the SRC partition coefficient software. (3) Log P for clavulanic acid of –2.23 (P = 5.88 x 10-3) was also calculated from a 2nd source (ACD/LogP, v5.0, using the ACD/I-Lab serive). The salt of amoxicillin could not be found, but the sodium salts of ampicillin, an antibiotic similar in structure to amoxicillin, and penicilllin G, another aminopenicillin, illustrate the fact that the presence of ionic charge (negative in these two cases) greatly reduces the drugs ability to absorb into hydrophobic environments. Ampicillin (uncharged) has P = 28.2, but decreases to P = 0.000389 when charged (ampicillin sodium), a 72,000-fold decrease! Penicillin G yields a similar result of P = 0.000977. Therefore, based upon these two examples, amoxicillin would also follow the same trend when having an overall net charge, as when the pH > 9.5. There is an inverse relationship between the solubility of a drug and its partition coefficient. When highly soluble in water, a drug will have little solubility in hydrophobic media such as plasma membrane. Take amoxicillin as an example. When it has little overall charge (net charge), the solubility is quite low (between pH of 2.0 and 8.0) and the partition coefficient is rather high (P = 9.33). But when it is has a substantial net charge (pH > 9.5), amoxicillin becomes quite soluble in water and insoluble in a hydrophobic environment (P = 10 -4). According to Goodman & Gilman (ref. 10), amoxicillin has “excellent” absorption in the GI tract relative to other antibiotics, especially ampicillin, which has “good” absorption. Active Transport According to Bretschneider, et. al. (ref. 11), many -lactam antibiotics are transported by the peptide transporter, PEPT1. This is a rather general transporter. It recognizes naturally occurring dipeptide and tripeptide substrates. -lactam antibiotics possess peptide-like structures such as the amino group and the carboxylic acid group. -lactam antibiotics resemble the backbone of physiologically occurring tripeptides, and is therefore, recognized and actively transported by PEPT1. This transporter is driven by a transmembrane H+ gradient, and it catalyzes the simultaneous transport of its substrates with H+. Although the PEPT1 actively transports many -lactam antibiotics, it has not been specifically established as an active transport mechanism for amoxicillin. Page 5 of 6 Group T Case Study #2, Part I According to Westphal, et. al. (ref. 12), an active transport mechanism does exist for amoxicillin because its intestinal absorption kinetics follows a zero-order process. Also, the existence of a transporter helps to explain the efficiency of amoxicillin absorption despite its physiochemical properties. Amoxicillin and other aminopenicillins have been shown to by transported by a dipeptide carrier-mediated process in vitro. This transport process is energized by an inward pumping of protons across the membrane. This gradient is induced by the exchange of sodium ions and protons, and calcium ions are involved in the control of this gradient. Using calcium channel blockers, like nifedipine, has been shown to significantly enhance absorption of amoxicillin. References 1. Zia, H. Shalchian, N. and Borhanian, F. Kinetics of amoxicillin degradation in aqueous solutions. Can. J. Pharm. Sci. 12(3): p 80-83 (1977). 2. Essack S. The Development of B-Lactam Antibiotics in Response to the Evolution of BLactamases. Pharmaceutical Research. Vol. 18, No. 10, October 2001. 3. Abrutyn E, Fraimow H, and Kaye S. Pathogens Resistant to Antimicrobial Agents. Infectious Disease Clinics of North America. Vol. 14, No. 2, June 2000. W.B. Saunders Company. 4. Rosenbloom H. Drug-Resistant Pathogens. RT Magazine. The Journal of Respiratory Care Practitioners. June 2000. CurAnt Communications, Inc. 5. http://www.rtmagazine.com/ 6. Patent: Dobfar, DE 2755903, 1978; Chemical Abstracts, Vol. 89, #146896. 7. Patent: Beecham Group, LTD. DE 2733230, 1978; Chemical Abstracts, Vol. 88, #136605. 8. Saismaa, T. and Totterman, A.M. Dissolution Studies on Ampicillin Embonate and Amoxycillin Embonate. Journal of Pharmaceutical & Biomedical Analysis, Vol. 8, No. 1 (1990), pages 61 – 65. 9. Bundgaard H. Polymerization of penicillins. II. Kinetics and mechanism of dimerization and self-catalyzed hydrolysis of amoxycillin in aqueous solution. Acta Pharmaceutica Suecica,14(1):47-66 (1977). 10. Petri, W.A., Jr. Chapter 45: Antimicrobial Agents (Continued); Penicillins, Cephalosporins, and Other -Lactam Antibiotics. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics, Tenth Edition (2001). 11. Bretschneider, B., Brandsch, M., Neubert, R. “Intestinal transport of -lactam antibiotics: analysis of the affinity at the H+/Peptide symporter (PEPT1), the uptake into caco-2 cell monolayers and the transepithelial flux.” Pharmaceutical Research. 16(1): 55-61, 1999. 12. Westphal, J., Trouvin, J., Deslandes, A., Carbon, C. “Nifedipine enhances amoxicillin absorption kinetics and bioavailability in humans.” Journal of Pharmacology and Experimental Therapeutics. 255(1):312-17, 1990. Page 6 of 6