* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download MR-Imaging in diagnosis and follow-up post corrective
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Myocardial infarction wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Aortic stenosis wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Congenital heart defect wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
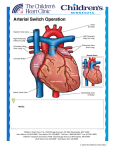
MR-Imaging in diagnosis and follow-up post corrective surgery of congenital heart disease A.G. Opitz¹, P. Fries¹, A. Lindinger², H.-J. Schaefers³, A. Buecker¹, G. Schneider¹ ¹Clinic of Diagnostic and Interventional Radiology ²Dept. of Pediatrics ³Dept. of Cardiac and Thoracic Surgery Saarland University Hospital, Homburg / Saar, Germany Background In neonates and infants with congenital heart disease (CHD) detailed imaging of vascular and cardiac anatomy is required for planning treatment and to follow up surgical procedures. Background One of the well-established applications of MRI is the evaluation of congenital heart disease. Accurate determination of cardiac anatomy and function is crucial for patient management at initial diagnosis as well as during follow-up of patients after repair of cardiovascular malformations. Background In addition to echocardiography, cardiac MRI is non-invasive diagnostic tool in children with CHD that does not require radiation exposure. Combination of cross-sectional and functional imaging together with CE MRA studies may give a complete overview on pre- and post surgical status and give important information for patient management. Learning objectives • In this educational exhibit we will review the use of MR imaging in the diagnosis of the different forms of congenital heart disease in pediatric patients. • An overview of common forms of CHD along with treatment procedures will be given. • Special interest is taken on technical issues and particularities in post surgical evaluation will be highlighted. Congenital heart disease (CHD) Classification of CHD: • Left - to - right shunts (acyanotic conditions) • Right- to- left shunts (cyanotic conditions) • Valvular and aortic anomalies Congenital heart disease Congenital heart disease Acyanotic conditions 60% Ventricular septal defect (VSD) 15 - 30 % Atrial septal defect (ASD) 5 - 10 % Patent Ductus Botalli (PDA) 10% Atrioventricular septal defect (AVSD) 2-4% Truncus arteriosus 1% Aortopulmonal window 1% Congenital heart disease Cyanotic conditions 20% Tetralogy of Fallot 6% TGA 4% Tricuspid atresia 2% Pulmonal atresia 2% Total anomalous pulmonary venous 2% return Univentricular heart 1% Congenital heart disease Valvular / aortal anomalies 20% Pulmonary stenosis 7% Coarction of aorta 7% Valvular aortic stenosis 6% Surgical shunts in CHD Shunt Classic Blalock-Taussig Modified Blalock-Taussig Procedure Subclavian artery to pulmonary artery end-to-side anastomosis Tube graft from subclavian artery to pulmonry artery Bidirectional Glenn SVC to RPA Fontan Procedure IVC to RPA to complete venous circulatic to PAS Waterson Ascending aorta to RPA Potts Descending aorta to LPA Surgical procedures in CHD Procedure Surgery Rastelli Procedure Transposition with a VSD Norwood Procedure Hypoplastic LV syndrome Mustard Procedure Arterial Switch (Senning) TGA: SVC/IVC baffled to LA/LV/PA, Pulmonary Veins baffled to RA/RV/Ao TGA: aorta and MPA are switched, coronary arteries are re-implanted Imaging technique • Combination of cross-sectional imaging and CEMRA provides functional evaluation and dynamic information • Examination should include: - Measurements of biventricular volumes, EF, mass - RVOT Cine sequences - Aortic root +/- aortic regurgitation quantification - Pulmonary regurgitant fraction - Assessment of LPA and RPA Atrial Septal Defect (ASD) • Most common CHD in adults • All connections between right and left atrium • 1/1500 live births • Majority repaired in childhood Asymptomatic / Symptomatic (dyspnea, heart failure, emboli, atrial fibrillation) Atrial Septal Defect (ASD) Classification: • Secundum – most common CHD (6-10%) – RAD • Primum – associated with other endocardial cushion defects (cleft AVvalves, inlet type, VSD) – LAD • Sinus Venosus – large, associated with anomalous pulmonary venous drainage (usually R superior PV) • Coronary sinus (rare) – associated with unroofed coronary sinus Atrial Septal Defect (ASD) Treatment: • Percutaneous Closure: only for secundum defect • Surgical Closure: Good prognosis if closure age < 25 and PA pressure <40 Atrial Septal Defect (ASD) Sinus venosous defect Atrial Septal Defect (ASD) Four chamber view of Ostium secundum defect ( CINE Sequence ) Atrial Septal Defect (ASD) Four chamber view of Septum primum defect ( CINE Sequence ) Ebstein´s anomaly and Atrial Septal Defect (ASD) Four chamber view ( CINE Sequence ) Ventricular Septal Defect (VSD) • Most common cardiac defect seen in infants and children (1.5-3.5 live births, 20% of CHD) Classification: • Perimembranous VSD (75-80%) • Muscular VSD (ca.15%) • Double commited subarterial VSD (5%) Ventricular Septal Defect (VSD) Four chamber view ( phase contrast sequence shows a flow signal traversing the ventricular septum (arrow) from right to left indicating “Eisenmengerreaction“). Patent Ductus arteriosus • Physiologic shunt between MPA and descending aorta • DA is substantially closed within 12-24 hours after birth • Usually completely sealed after to four three weeks Patent Ductus arteriosus Patent Ductus arteriosus • If DA remains patent, left to right shunt occurs • Untreated risk of Eisenmenger´s reaction • In complex heart disease (TGA) PDA is the only way to supply oxygenated blood Coarctation of the Aorta • Focal aortic narrowing close to ligamentum arteriosum (postductal type) • Presence of collaterals • in 30 - 50% associated with bicuspid aortic valve Coarctation of the Aorta Differential diagnosis: • tubular hypoplasia (preductal type) • interrupted aortic arch • pseudocoarctation • Takayasu arteritis Coarctation of the Aorta Operative technique Comment Resection with end-to-end anastomosis patients older than 1 year Resection with extended anastomosis enlargement of hypoplastic aortic arch Prosthetic patch aortoplasty high incidence of late aneurysms Interposition (tube) graft if long segment of CoA is present Subclavian flap aortoplasty primarily used in younger children Coarctation of the Aorta MIP shows coarctation of the aorta with subsequent subtotal stenosis of the vessel Coarctation of the Aorta Coarctation of the Aorta Coarctation of the Aorta Coarctation of the Aorta Sag. MRI post intervention Tetralogy of Fallot Most commom cyanotic condition,composed of four features: • • • • • subpulmonary infundibular stenosis ventricular septal defect (VSD) overrriding of the aortic valve right ventricular hypertrophy Variability correlates with degree of RVOT obstruction and size/anatomy of PA Tetralogy of Fallot Treatment Reparative • takedown of prior shunt • closing the VSD • relieving the RVOT: pulmonary valvotomy, resecion of infundibular muscle, transannular or RVOT patch Tetralogy of Fallot Treatment: Palliative • Blalock-Taussig-Shunt: End-to-side anastomosis between subclavian artery and ipsilateral pulmonary artery Tetralogy of Fallot Complications following surgery: • Shunt obstruction or stenosis • Pseudoaneurysms • Pulmonary hypertension and/or left ventricular dysfunction • "Pseudo RVOT" from endothelial overgrowth and obstruction of the conduit Tetralogy of Fallot Tetralogy of Fallot Tetralogy of Fallot MRI post surgery (CINE ax.) Tetralogy of Fallot MRI post surgery (MPR, MIP cor.) Tetralogy of Fallot 6yo patient with surgically corrected TOF. CE CINE short axis view shows subvalvular RVOT dilatation. Transposition of the great arteries (TGA) • TGA approximately 5% of all congenital heart disease, • CCTGA in approx. 0.6-1.4%. Classification • D-TGA 1. Simple TGA (isolated TGA): with intact ventricular septum 2. Complex TGA: with VSD or other defects Transposition of the great arteries (TGA) Classification: L-TGA (“congenitally corrected” TGA) 1. Isolated: without other defects 2. CCTGA with other defects: • • • Tricuspid valve anomalies (90%) VSD (75%) Pulmonary valve stenosis (75%) D-TGA Systemic and pulmonary circulations consist of two parallel circuits: • • IVC+SVC→ RA→ RV→ transposed aorta→ systemic circulation→ IVC+SVC PV→ LA→ LV→ transposed PA→ pulmonary circulation D-TGA • Cocordant atrioventricular and disocordant ventriculoarterial connections • PA from LV, Aorta from RV and anterior/right of PA • corrected initially with prostaglandin to keep DA open and balloon, atrial septostomy to improve systemic saturation • repair via “atrial switch” Mustard procedure – SVC/IVC baffled to LA/LV/PA – Pulmonary Veins baffled to RA/RV/Ao – repair via “arterial switch” D-TGA post surgery 5yo patient after arterial switch procedure. CE-MRA shows aneurysm of the ascending aorta. D-TGA post surgery 5yo patient after arterial switch procedure. MIP shows aneurysm of the ascending aorta. L-TGA • • Double discordance: Discordant atrioventricular and discordant ventriculoarterial connections Without associated anomalies asymptomatic until adulthood L-TGA Complications after atrial redirection surgery (Mustard or Senning procedure): • Bradyarrhythmia • Tachyarrhythmia • Baffle obstruction • Baffle leak • Ventricular dysfunction • Sudden cardiac death Pulmonary veins / arteries: • • • • Anomalous pulmonary venous return (APVR) - Total APVR (2% of patients with CHD) - Partial APVR (0.3 - 0.5% of patients with CHD) Pulmonary Sequestration Scimitar Syndrome Pulmonary Atresia (with and without VSD) Pulmonary veins / arteries: • PAPVR Pulmonary veins / arteries: • PAPVR post surgery Note the surgical connection of the SCV to the left atrium (arrow). Pulmonary veins / arteries: Coronary MIP shows partial anomalous venous return. Note on the left side a so-called vertical vein draining to the superior caval vein and on the right side the superior pulmonary vein draining to the SCV adjacent to the acygos vein. Pulmonary veins / arteries: • Anomalous venous return of upper right pulmonary vein in the SCV adjacent to the drainage of the acygos vein. Pulmonary veins / arteries: Pulmonary Atresia • with ventricular septal defect (VSD) and • multiple aortopulmonary collateral arteries (MAPCAs), hypoplastic pulmonary arteries • with intact VS, normal sized pulmonary arteries supplied by ductus arteriosus and patent foramen ovale Pulmonary veins / arteries: • Imaging post surgery - Blalock-Taussig shunt - Glenn shunt - Hemi-Fontan - Kawashima operation - Fontan Pulmonary veins / arteries: Functionally univentricular heart and Glenn shunt Pulmonary veins / arteries: Kawashima operation Bilateral Glenn shunt and incorporation of the azygos vein in cavopulomonary anastomosis. Thank you very much for your attention!