* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Genetics and Innate and Adaptive Immunity in IBD
Vaccination wikipedia , lookup
Herd immunity wikipedia , lookup
Plant disease resistance wikipedia , lookup
Molecular mimicry wikipedia , lookup
Gluten immunochemistry wikipedia , lookup
Complement system wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Inflammation wikipedia , lookup
DNA vaccination wikipedia , lookup
Social immunity wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Autoimmunity wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Adaptive immune system wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Innate immune system wikipedia , lookup
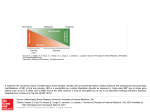
Genetics and Innate and Adaptive Immunity in IBD Galliano Zanello, David Kevans, Ashleigh Goethel, Mark Silverberg, Andrea Tyler and Kenneth Croitoru Inflammatory bowel disease (IBD) is thought to be due to an abnormal inflammatory response within the gut in response to a trigger that has yet to be identified. The strong family history in many patients, especially those with Crohn’s disease suggests a genetic predisposition. It has been hypothesized that the abnormal inflammatory response is due in part to genetically determined alterations in the normal homeostatic processes in play at the gut mucosa that normally serve to ensure a symbiotic relationship between the host and the ‘normal’ gut microbes. Genetic studies in patient cohorts have identified an increasing number of risk alleles that highlight a diverse series of molecular and cellular pathways that may be altered in these individuals. These pathways include: defects in epithelial barrier function, genes involved in autophagy, a cellular pathway not previously considered in studies of IBD, receptors of innate immune response, and immune and cytokine-related genes that are involved in the effector and regulatory arms of the adaptive immune response. Animal and human studies further highlight how altered innate immune responses can be involved in intestinal inflammation and how abnormal adaptive immune responses in IBD patients are directed against the intestinal microbiota. The loss of the normal homeostatic mechanisms with activation of both innate and adaptive immune responses may well be key to the initiation and propagation of IBD. The adaptive immune response has long been the focus of study in understanding the pathogenesis of IBD. Th1 and Th2 T cell subsets have been identified as mediators of immune inflammation in early studies, and antigen-specific responses key to their activation. Indeed, studies have shown bacterialderived antigens as initiators and drivers of T cell immune responses. More recently, Th17, regulatory T cells and unconventional innate-like T cells have been identified as important in the induction and regulation of intestinal inflammation, and efforts are in place to define their role in IBD. The seminal discoveries of pathogen recognition receptors including 8 Toll-like receptors and nucleotide-binding oligomerization domain receptors have changed our understanding of how immune cells without antigen-specific receptors respond to microbes and can lead to the secretion of inflammatory cytokines in the intestine. The role innate receptors play in intestinal inflammation and homeostasis has been supported by a number of animal studies; however, the role innate immune responses and the various innate receptors play in the development and perpetuation of IBD remains to be determined. In conclusion, understanding the role of genetically determined alterations in innate and adaptive immunity in patients with IBD will lead to new strategies for the prevention and treatment of IBD. 9