* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biol 155 Human Physiology
Neuroendocrine tumor wikipedia , lookup
Hypothyroidism wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Vasopressin wikipedia , lookup
Kallmann syndrome wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Pituitary apoplexy wikipedia , lookup
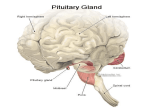
Pituitary Gland Pituitary development: The “Master Gland” The pituitary has been called the “Master” gland in the body. This is because most of the pituitary hormones control other endocrine glands Hormones of the anterior pituitary There are 6 main hormones which are secreted by the adenohypophysis: 1) Growth hormone (also known as somatotropin). 2) Thyroid-stimulating hormone (also known as thyrotropin). 3) Adrenocorticotropic hormone (also known as corticotropin). 4) Prolactin. 5) Follicle-stimulating hormone. 6) Luteinizing hormone. Control of pituitary gland secretion Secretion of each hormone by the adenohypophysis is controlled by neurohormones secreted by nerves in the hypothalamus. In most cases there are two neurohormones controlling the secretion of a pituitary hormone. One which stimulates pituitary secretion and one which inhibits pituitary secretion. Neurohormones: Are hormones secreted by nerve cells. These are true hormones, since they are secreted into the bloodstream. All are secreted by neurosecretory neurons in the hypothalamus. They are secreted into the hypophyseal portal system, which then carries the blood to the anterior pituitary. Pituitary portal system Arterioles break into capillaries in the hypothalamus. The axons of the neurosecretory cells form plexuses with these capillaries. Downstream, the capillaries combine into a vein which carries the blood to the pars distalis. The vein breaks into a capillary network which supplies all the cells of the anterior lobe. Thus, the neurohormones are carried directly (well, sort of) from the hypothalamus to the adenohypophysis. Portal system Growth hormone (GH) Growth hormone is secreted by somatotrophs. GH is a protein hormone consisting of a single peptide chain of 191 amino acids. GH secretion is stimulated by the secretion of Growth Hormone Releasing Hormone (GHRH) by the hypothalamus. GH secretion is inhibited by the secretion of somatostatin by the hypothalamus. GH activates a tyrosine kinase receptor. Functions of GH: GH has effects of every cell of the body, either directly or indirectly. Primarily, it decreases the uptake and metabolism of glucose. (Elevates plasma glucose) Increases the breakdown of fat. (Increases the blood levels of fatty acids) Increases the uptake of amino acids from the blood and increases protein synthesis in cell. (Decreases plasma amino acids) Actions of GH on specific cell types: Muscle cells: Increases amino acid uptake Increases protein synthesis Decreases glucose uptake Net result: Increased Lean body mass Chondrocytes: Increases uptake of sulfur increases chondroitin sulfate production increases DNA, RNA synthesis increases Protein synthesis increases Amino acid uptake increases Collagen synthesis increases Cell size and number Net result: Increased Linear growth Hepatocytes: Stimulates the production of somatomedins by the liver. These somatomedins directly regulate metabolic function in target cells. They are also called insulinlike growth factors, or IGFs. Adipocytes: Decreases glucose uptake Increases lypolysis Net result: Decreased Adiposity Other cell types in general: Increased protein synthesis Increased DNA, RNA synthesis Increased cell size and number Net result: Increased organ size Increased organ function Other considerations: GH has a short half-life of about 20 minutes. However, the IGFs are much longer lived (T1/2 of about 20 hours). GH and Insulin actions are correlated: When there is ample dietary intake of proteins and carbohydrates, then amino acids can be used for protein synthesis and growth. Under these conditions, both insulin and GH secretion are stimulated. Net result: Amino acids are shunted to protein synthesis and glucose is shunted to metabolism. However, under conditions where only carbohydrates are ingested, insulin secretion is increased, but GH secretion is decreased. Net result: Both glucose AND amino acids are shunted to metabolism. Pathophysiology of abnormal GH secretion: Hyposecretion: Pre-adolescents: Decreased GH secretion (or sensitivity) results in slow growth and delayed onset of sexual maturation. These children also tend to be slightly chubby. Post-adolescents: Generally, no serious problems are associated with hyposecretion of GH in mature individuals. However, in very severe cases there can be progeria (rapid and premature aging). Hypersecretion: Pre-adolescents: (before closure of epiphyseal plates) Hypersecretion results in gigantism, where affected individuals grow extremely rapidly and become abnormally tall (even over 2.4 m). Body proportions remain relatively normal. Usually, there are cardiovascular complications later in life. Post- adolescents: (after epiphyseal closure). Hypersecretion results in tissue enlargement. This is particularly true of the bones, which get heavier and thicker. They cannot elongate since the epiphyseal plates are closed. A common symptom is a coarsening of the facial features and enlargement of the hands and feet. This condition is known as acromegaly. Treatments of GH secretion disorders: Hypersecretion is usually caused by a tumour in the pituitary gland. Treatment consists of surgical or radiation ablation of the tumour mass. Hyposecretion is usually treated in children by hormone replacement therapy. This is generally not required in adults, unless GH secretion is completely abolished. Prolactin (PRL) Structurally, very similar to growth hormone (single peptide chain of 198 amino acids). PRL is secreted by mammotrophs (also referred to as lactotrophs). Secretion of PRL is also under dual control by the hypothalamus. Primarily under inhibitory control. This means that if there is an injury to the hypophyseal portal system which blocks hypothalamic regulation of the pituitary gland, PRL levels increase. All other pituitary hormone levels decrease when this happens. Dopamine is secreted by neuroendocrine cells in the hypothalamus and inhibits PRL release. PRL release is stimulated by thyrotropin releasing hormone (TRH), vasoactive intestinal peptide (VIP) and at least one other as yet unidentified factor. PRL activates a tyrosine kinase receptor. Functions of PRL: In humans, the only effects of PRL so far identified are on reproduction and nursing. PRL is important in stimulating differentiation of breast tissue during development. Stimulates further development of mammary glands during pregnancy. Stimulates milk production (lactation) after pregnancy. PRL has a role in regulation of the female reproductive cycle. However, its precise role has not be delineated yet. Excess PRL secretion is know to block synthesis and release of gonadotropins, disrupting menstruation and causing infertility. PRL also can regulate male fertility, but how it does so remains unclear. Pathophysiology of PRL secretion: Hyposecretion is never seen. However, hyperprolactinemia (excess secretion of PRL) is a fairly common disorder. Symptoms in women usually include amenorrhea (cessation of menstruation), galactorrhea (abnormal lactation) and infertility. In men, infertility and galactorrhea are the most common symptoms. Treatment usually consists of administration of a dopaminergic agonist, such as bromocriptine. Cellular mechanism of pulsatile LHRH release. 1998. E. Terasawa. General and Comparative Endocrinology. vol. 112:283-295 Thyroid Stimulating hormone (TSH) TSH is a glycoprotein hormone composed of 2 peptide chains a and b. The a subunit is called “unspecific” because it is also incorporated into two other unrelated pituitary hormones (LH and FSH). The b subunit contains the biologically active sites. However, it must be combined with the a subunit in order for the hormone to be active. TSH secretion is controlled very tightly by the hypothalamus. TSH secretion is stimulated by Thyrotropinreleasing hormone (TRH). TRH is a tripeptide, meaning it is composed of three amino acids. TRH secretion is stimulated by thermal and caloric signals in the brain. Control of TSH secretion Negative control of TSH secretion occurs in two ways: Triiodothyronien or T3 (which will be discussed later) feeds back on the hypothalamus to stimulate secretion of dopamine and somatostatin. These two factors both function as TSH-release inhibiting factors. T3 can feed back directly onto the thyrotrophs to directly inhibit TSH secretion. Function of TSH: TSH stimulates the follicular cells of the thyroid to induce a number of responses: TSH activates both the cAMP and PIP pathways: Increased cAMP Increased [Ca2+]i TSH can stimulate both cell growth (of follicular cells) and secretion of T3 and thyroxine ( T4 ). Adrenocorticotropic hormone (ACTH) ACTH is a single peptide chain which is relatively small (30 amino acids). ACTH secretion is primarily under stimulatory control (i.e. there isn’t an ACTH-release inhibitory factor). ACTH secretion is stimulated by corticotropin releasing hormone (CRH). CRH secretion can be stimulated by a large number of factors, most of which would be considered stress factors. Examples; infection, trauma, sleep cycle, anxiety, depression and others. (Just remember stress). Functions of ACTH: ACTH stimulates the adrenal gland to secrete cortisol. ACTH levels are associated with the sleep cycle. ACTH stimulates the cAMP pathway in adrenocorticol cells. ACTH can directly inhibit CRH secretion (negative feedback). Follicular-Stimulating hormone (FSH) Luteinizing Hormone (LH) These are generally grouped together and called gonadotropines. Gonadotropins are secreted by the gonadotrophs, which synthesize and secrete both LH and FSH. Both LH and FSH are peptide hormones. Secretion of gonadotropins is mainly under positive control. Hypothalamus secretes gonadotropin-releasing hormone (GnRH) which stimulates gonadotrophs to secrete both LH and FSH. Functions of LH and FSH: LH and FSH stimulate secretion of the sex steroids by the gonads. Mainly estrogen in women and testosterone in men. FSH also stimulates gonadal release of inhibin, which serves as a negative feedback factor to block release of FSH by pituitary. LH and FSH stimulate the gonadal release of activin, which can have positive feedback on gonadotropin secretion by the pituitary. Gonadal secretion of estrogen and testosterone can negatively feedback on both the hypothalamus, to reduce GnRH secretion, and the gonadotrophs directly, to reduce gonadotropin secretions. Hormones of the posterior pituitary: Remember that the neurohypophysis serves as a storage organ for hormones produced by neurosecretory cells in the hypothalamus. There are two hormones secreted by the neurohypophysis: 1) antidiuretic hormone (ADH) 2) oxytocin Both hormones are peptide hormones containing 9 amino acid residues. They differ in only 2 amino acids, but have very different functions. ADH Term: diuresis means production of urine. ADH inhibits urine production, i.e. conserves water in the body. Main target for ADH are the cells in the kidney which reabsorb water (will be covered in detail in the section on renal physiology). ADH secretion is stimulated by either an increase in the osmotic concentration of the blood, or by a decrease in blood volume usually sensed by a decrease in blood pressure. Secretion of ADH causes retention of water, which will tend to counteract both an increase in blood concentration and/or decrease in blood volume. Cannot overcome serious blood loss. Conversely, excess consumption of water will have two effects: increase blood volume (and pressure). decrease blood concentration. Under these conditions ADH secretion is inhibited. This results in formation of more urine, which is usually fairly dilute. Blood loses water and thus volume. Oxytocin Release of oxytocin is under neural control (like with ADH). However, unlike ADH, the release of oxytocin is largely controlled by emotional state. Oxytocin specifically stimulates certain smooth muscles to contract. Primarily those of the reproductive tract and mammary glands. Oxytocin is required for nursing. Principally know as the “milk letdown factor”. It is secreted within seconds of the onset of suckling. Sensory receptors in the nipples generate afferent impulses that stimulate the hypothalamus, triggering oxytocin secretion. Can actually be secreted in response to auditory input, i.e. in nursing mothers in response to hearing their babies cry. Effects of Oxytocin Oxytocin stimulation at low doses causes rhythmic contractions of the uterus. Oxytocin stimulation at high dose causes sustained tetanic uterine contractions. Oxytocin is often used to induce labour. It is now generally believed that oxytocin believed that oxytocin produced by the fetus plays a critical role in labour. Oxytocin is also used to stop post-partum bleeding. The number of oxytocin receptors in uterine smooth muscles increases towards the end of pregnancy. Oxytocin affects smooth muscle cells in uterus and vagina of non-pregnant women. There is clear evidence that oxytocin is involved in sexual arousal and orgasm in both men and women. What role it plays in men is unknown. However, it may play a strong role in reinforcing the pair-bond. The role in women is only slightly better known. Oxytocin is secreted in response to vaginal distention during intercourse. Oxytocin is also secreted in response to stimulation of the nipples. Emotional considerations Oxytocin secretion during sexual intercourse probably serves to reinforce the male-female pair-bond. Often referred to as the “the cuddle hormone” or “the love hormone” in the popular press. Secretion of oxytocin during and after labour may play an important role in the formation of the mother-child pair-bond. Oxytocin secreted during suckling may serve to reinforce this pair-bond. Recent studies with knock out mice has shown that oxytocin is critical in initiating and maintaining maternal care. Oxytocin secreted in response to suckling can cause uterine contractions which may play a role in the recovery of uterine muscle tone after pregnancy and may serve to shrink the uterus back to normal. Pituitary evolution Teleost Pituitary Bichir (Paleonisci) Sturgeon (Ascipenseridae) Bowfin (Amiformes) Gar (Amiformes) Bass (Teleostei) Sarcopterygii (Fleshy finned fishes) Made up of two extant groups: Dipnoi Lungfish Crossopterygii Lobe finned fishes Coelacanths Lungfish (Dipnoi) Ceolocant (Crossopterygii) Fire Salamander (Urodel) Bullfrog (Anuran) Lizards and snakes (Squamata) Albatross (Aves)