* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Which Patients with Coronary Artery Disease are at Greater Risk for
Survey
Document related concepts
Heart failure wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Drug-eluting stent wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Transcript
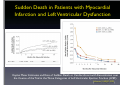
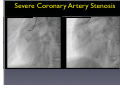
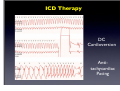
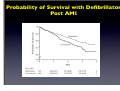
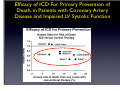
Which Patients with Coronary Artery Disease are at Greater Risk for Sudden Cardiac Death, and What Can We Do To Lower the Risk? Dr Stanley Chia MB ChB, MD, MRCP, FAMS Consultant Cardiologist National Heart Centre Singapore Sudden Cardiac Death (SCD) • • • Catastrophic and unpredictable event resulting from an abrupt loss of cardiac function Occurs within minutes after symptoms appear • To reduce the incidence of SCD, accurate and timely prediction of risk is of paramount importance. Most common underlying reason for SCD is coronary artery disease and is frequently the consequence of an acute ischaemic event • However, no tests have been proven to predict SCD accurately Who is at Risk? • Although SCD often occurs in active, outwardly healthy people with no known heart disease, but the truth is that SCD is not random and most victims do have underlying heart diseases or other health problems, albeit unknown • There are numerous contributors to cardiac arrest, but two of the most important ones are: • Previous myocardial infarction: 75% of people who die of SCD show signs of a previous MI. • Coronary artery disease: 80% of SCD’s victims have signs of coronary artery disease. Atherosclerosis: an Inflammatory Disease Fig 1 Fig 2 Fig 3 Fig 4 Ross R. NEJM 1999 Decades Years-Months Healthy Subclinical Months-Days Symptomatic Intima Lumen Media Lumen narrowing Plaque Progression Compensatory expansion preserves lumen diameter Normal Vessel Minimal CAD Moderate CAD Expansion overcome: lumen narrows Severe S CAD Identifying Patients with Silent Coronary Artery Disease Smoking Diabetes Mellitus Hypertension Obesity Sedentary lifestyle Depression Diet Emotional stress Investigations to Detect Significant Coronary Artery Disease, Myocardial Ischaemia and LVEF ECG & Stress ECG test Calcium Score and CT Coronary Angiography Echo & Stress Echocardiography Myocardial Perfusion Study Coronary Angiography Risk Stratification for SCD • Studied primarily in patients with • • History of acute myocardial infarction Congestive heart failure Both recognized to be at increased risk for SCD • Most randomized trials with Implantable Cardioverter Defibrillator (ICD) therapy have shown reduction in SCD and mortality, but most patients (2/3) enrolled in these trials did not receive therapy (ICD shock or antitachycardia pacing) • Hence, in addition to left ventricular ejection fraction (LVEF), how can we determine who will benefit from ICD?? Assessment of SCD Risk • Left Ventricular Ejection Fraction (LVEF) • Symptoms of Heart Failure: NYHA class • Other Tests to predict SCD vulnerability? • Non-sustained Ventricular tachycardia, Microvolt Twave alternans, measures of cardiac autonomic modulation, QT interval, Signal-averaged ECG, Electrophysiology study and Imaging studies, Genetic studies Normal Left ventricular systolic function Echocardiogram Impaired Left ventricular systolic function Left Ventriculogram Left Ventriculogram Left Ventricular Ejection Fraction • LVEF is well recognized as a predictor of allcause mortality in patients with CAD • In the VALIANT trial (I=14 609), LVEF was a strong predictor of SCD or cardiac arrest • Risk of SCD or cardiac arrest increased by 21% for every 5% decrease in LVEF • Low LVEF (35%) was the main entry criterion in large randomized trials of primary prevention ICD therapy (MADIT-II and SCD-HeFT ICT studies). • However, 2/3 of patients randomized to ICD therapy in did not use their ICD during 3-5 year follow-up Sudden Death in Patients with Myocardial Infarction and Left Ventricular Dysfunction Kaplan Meier Estimates and Rate of Sudden Death or Cardiac Arrest with Resuscitation over the Course of the Trial in the Three Categories of Left Ventricular Ejection Fraction (LVEF). Solomon S. NEJM 2005 Heart Failure Symptoms: NYHA Class • Functional class provide a potent risk stratification tool • Patients with NYHA class II and III symptoms are at higher risk for SCD than death from progressive pump failure, and are more likely to benefit from ICD. (Improvement in survival for class III: HR=0.66) • In contrast, patients with NYHA class IV symptoms are more likely to die of pump failure. • No clinical trials done exclusively for patients with class 1 symptoms, although they are well represented in primary prevention trials Other Specific tests that may potentially predict SCD • Presence of nonsustained ventricular tachycardia (NSVT) post myocardial infarction • • In a large study of post-AMI patients, NSVT predicted SCD, but could not discriminate between risk of SCD and non-SCD. Furthermore, it was not a predictor for patients with LVEF35% Microvolt T-wave Alternans • • • Change in T-wave amplitude, width or shape in alternate beats High negative predictive value, but low positive predictive value Major limitations: High percentage of indeterminate tests and absence of prospective data on treatment guided by MTWA. Other Specific tests • • • • Measures of cardiac autonomic modulation • Heart rate variability, Baroreflex sensitivity, QT interval, QT dispersion and QT variability • May be predictive of all-cause or cardiac mortality, but do not predict SCD, and have not been proven to be clinically useful Signal-averaged ECG • To detect low amplitude, high-frequency electrical signals at the end of QRS complex, known as late potentials • Associated with higher rate of arrhythmia in patients with CAD and poor LVEF, but poor predictive value on its own. Invasive Electrophysiology study: not predictive of SCD Imaging studies, Genetic testing , Serum markers • Exploratory Although many tests of SCD vulnerability have been examined in patients with IHD, current data do not support the consistent use of any test, other than LVEF, to risk stratify these patients. How to lower the risk of SCD? • Optimal Management of Coronary Artery Disease • Lifestyle Modification: Healthy Diet, Exercise, Smoking cessation, Reduce Stress • Pharmacotherapy: Anti-platelet agents (Aspirin/ ticlopidine/clopidogrel), Anti-anginal agents (blockers, calcium channel blockers, nitrates), ACE inhibitors, Lipid lowering therapy • Revascularization to Relieve Ischaemia and Improve LVEF: Percutanenous Coronary Intervention or Coronary Artery Bypass Grafting Surgery Severe Coronary Artery Stenosis Definitive Therapy: Implantable Cardioverter-Defibrillator ICD Therapy DC Cardioversion Antitachycardiac Pacing MADIT II: All-cause mortality Endpoint ICD group Conventional therapy group Hazard ratio (95% CI) p value All-cause 105 97 (19.8%) 0.65 (0.51 – 0.93) 0.016 mortality (14.2%) MADIT II: Mortality events Cause of death ICD group Conventional therapy group Noncardiac 26 20 Cardiac 74 67 27 (3.6%) 46 (9.4%) 41 18 Arrhythmic Nonarrhythmic Patients with LVEF30%, 1 mth after AMI Randomized to ICD or medical therapy Moss et al. N Engl J Med 2002;346(12):877-83. Probability of Survival with Defibrillator Post AMI Efficacy of ICD For Primary Prevention of Death, in Patients with Coronary Artery Disease and Impaired LV Systolic Function Summary • Sudden cardiac death occurs most frequently in • • • patients with prior MI, Heart Failure and underlying CAD Current available tests are unable to predict SCD accurately LVEF remains the best predictor of SCD Management is targeted at treating the underlying CAD and heart failure • Consider ICD for patients with LVEF 30-35% • Most patients with ICD, however, do not receive any therapy from the ICD over the initial 3-5 years Thank you