* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Rhythms That Go Bump in the Night
Remote ischemic conditioning wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
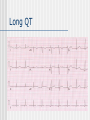
Rhythms That Go Bump in the Night Teresa Menendez Hood, M.D. FLB’s Creepy VF Eerie VT Scary AF Ghostly Torsade Sudden Cardiac Death Death within one hour of onset with an abrupt change in clinical status In the field: VF is present 40%, EMD 20% and Asystole 40% Order of survival: 25%, 6%, 1% Monomorphic VT is actually not that common This represents 50% of ALL cardiac deaths (300,000/year) It is the initial manifestation of CAD in ½ of all SCD victims. 20% will have no structural heart disease. CAD accounts for 80% of all SCD in Western societies Only 20% are due to an acute MI Risk Factors: coronary artery disease and its risk factors, LVH, certain cardiomyopathies and genetic diseases Transient risk factors include: ischemia, systemic abnormalities, autonomic factors and proarrythmic factors At EPS:54% will have inducible VT and 30% will have inducible PMVT Creepy VF Inventor of the external defibrillator! Paul Zoll, M.D. Original article: NEJM 1960 Ventricular Fibrillation: Treatment and Prevention by External Electric Currents Ventricular fibrillation, usually a rapidly fatal arrhythmia, occurs most commonly in coronary-artery disease, in patients with atrioventricular block and in toxic reactions to digitalis, quinidine and procaine amide. Occasionally, it succeeds ventricular tachycardia. This paper presents additional experiences confirming the clinical value of external countershock in terminating ventricular tachycardia and fibrillation and of external electric stimulation in preventing these arrhythmias. Alternating current (60 cycle, 0.15 second, 150 to 450 volts) was applied to the unopened chest with large electrodes. A cardiac pacemaker providing monophasic rounded impulses of 2 milliseconds duration over wide ranges of rate and amplitude was used to stimulate the heart externally. Ventricular tachycardia and fibrillation were terminated by externally applied electric countershock more than five hundred and thirty-two times in 8 patients; 5 have survived for one month to two and a half years. The technique is immediately effective, clinically feasible and safe. Prevention of recurrent ventricular tachycardia and fibrillation in patients with complete heart block remains an unsolved problem. Drugs are largely ineffective; external electric cardiac stimulation at rates above the basic idioventricular rate has been effective in preventing these recurrent ventricular arrhythmias, but long-term stimulation is difficult. Zoll PM, Linenthal AJ, Normal Zarsky LR. Ventricular Fibrillation: Treatment and Prevention by External Electric Currents. New Eng J Med 1960; 262:105-112. VF The primary arrhythmia responsible for SCD Acute treatment is with external defibrillation VT or SVT with Aberrancy? VF (or the EKG of JELLO) Ben Franklin would say electricity is a good thing! ICD shock Eerie VT in patients with CAD Usually seen in patients with a prior MI:extensive, healed, at least 2 weeks old May result in syncope or SCD Poor predictors: previous large MI that involves the septum and with low EF; if the MI involved CHF/hypotension or VF that is also not good; if you are left with an LV aneurysm or a wide QRS(>120ms) in NORMAL SINUS RHYTHM. VT with CAD VT with CAD Wide complex tachycardia If the patient has structural heart disease, then it is VT It does not matter what the BP is in your decision making Things that favor VT: • positive or negative concordance, visible AV dissociation, NW axis, absence of an RS complex in all the precordial leads(v1-v6), R:S interval >100ms in any precordial lead Things that favor SVT with aberrancy: • Looks like a classic LBBB/RBBB (know what this is in V1 and lead 1), has the same QRS as in NSR LBBB SVT with Aberrancy VT or SVT? A sixty-five-year-old female is POD #1 after appendectomy for acute appendicitis. She has a history of prior bypass surgery and hypertension; her medications include aspirin, atenolol, and lisinopril. The following asymptomatic arrhythmia is noted on telemetry: VT or SVT? Always err on side that is is VT because……… 1. VT is more common than SVT with aberrancy 2. In patients with structural heart disease, particularly prior infarction, VT is much, much more common than SVT with aberrancy 3. If SVT is misdiagnosed as VT for the purposes of acute treatment, no harm will come to the patient 4. If VT is misdiagnosed as SVT for the purposes of acute treatment, a cardiac arrest can be precipitated VT with CAD Mechanism is reentry which means that is can be induced by EP study using PES and can be entrained and reset Do not worry, only EP’s understand this Among patients with spontaneous VT and CAD , 95% will have it induced in the lab 22% will need 2 sites used for induction of VT (RVA and RVOT) VT with CAD The key feature that predicts how well tolerated it will be is the rate and thus dictates the initial strategy If not well tolerated? SYNCH CVN Little data that Lidocaine does anything..may be helpful if patient is having an MI IV amiodarone is the drug of choice for acute stable VT or VT recurrences Long term treatment should be an ICD with or without AAD therapy(amiodarone or Class III drugs) VT with Idiopathic Dilated Cardiomyopathy IDC:Can have multiple etiologies and 1/3 are familial Arrhythmogenesis may be due to extensive subendocardial scarring and patchy fibrosis which can lead to areas of reentry Other triggers may be microvascular ischemia,electrolyte abnormalities, geometric alterations and changes in catecholamines. VT with IDCM Bundle Branch Reentry VT-this is a VT that occurs in up to 30% of patients and is a reentrant circuit in the His Purkinje system.This VT tends to be fast (~300 beats per minute) and result in syncope and degenerate to VF. This VT is treated with ablation on the RBB and not an ICD! IDCM These patients tend to have EMD or Bradyarrythmias along with VT/VF as a mode of SCD (especially in those with Functional Class 4 CHF) Syncope should be taken seriously and is an indication for ICD EP studies are not as predictive as in patients with CAD Amiodarone appears to be more helpful than in patients with CAD VT with Arrhythmogenic Right Ventricular Dysplasia 17% cause of SCD in the young in the US Familial in 30% More common in men and with exercise VT’s usually come from the RV Fibrous tissue and fat in the RV (the epicardial layer) and replaces normal myocardial cells EKG usually may show an epsilon wave in the RV leads or t wave inversion and see ST elevation on stress testing of the RV leads Positive signal average EKG Treatment is ICD +/- Ablation EPSILON WAVE-can you see it? This is called an epsilon wave, and reflects delayed conduction in the right ventricle, a right ventricular “late potential”. This is a classic ECG for arrhythmogenic right ventricular cardiomyopathy. VT in Hypertrophic Cardiomyopathy HCM is when there is hypertrophy in the absence of a cardiac or systemic cause Due to genetic mutations in the cardiac sarcomere proteins and autosomal dominant in 45% Can get AFIB which is not tolerated well VT/VF is often preceded by AFB or ST Those who are young and male have the worst prognosis They tend to also have microvascular ischemia, autonomic dysfunction and abnormal response to exercise VT with HCM 40% of the SCD occurs during or after exercise They also have enhanced AV nodal conduction which makes their atrial fibrillation conduct faster and 5% have an accessory pathway Those at highest risk are those with positive FH of SCD, NSVT, Syncope, Inducible VT/VF at EP study, and abnormal BP to exercise. EKG in HCM It varies from normal to significantly abnormal. Left ventricular hypertrophy is common. Often has left anterior hemiblock. Q waves in anterolateral leads which can simulate recent myocardial infarction is not unusual. Many times deep Q in II, III , AVF with ST segment elevation can be seen. Other causes of scd Valvular Congenital Heart Disease MVP Neurological Disease- “cerebral T waves” Congenital Long QT Myocarditis WPW, Brugada, Short QT Coronary anomalies-anomalous artery passes between the aorta and the pulmonary trunk • “A congenital heart defect caused the death of an Everman High School football player who collapsed Thursday morning on the school track, according to preliminary findings released Friday by the Tarrant County medical examiner’s office. “ DMN 10/17/03 Intracerebral Hemorrhage Short QT Syndrome A Familial Cause of Sudden Death The short QT syndrome is characterized by familial sudden death, short refractory periods, and inducible ventricular fibrillation. It is important to recognize this ECG pattern because it is related to a high risk of sudden death in young, otherwise healthy subjects. Normal Heart VT:Idiopathic Yes……it does exist RVOT VT-catecholamine sensitive LVOT VT-catecholamine sensitive Fascicular VT-from left anterior or posterior fascicle-Belhassen's VT. Due to microreentry and adenosine sensitive and can respond to verapamil. These are treated with ablation and NOT AN ICD! RVOT VT Long QT Mutations in potassium-channel genes KCNQ1 (LQT1 locus) and KCNH2 (LQT2 locus) and the sodium-channel gene SCN5A (LQT3 locus) are the most common causes of the congenital long-QT syndrome Long QT WPW WPW WPW with AFIB Brugada Brugada Polymorphic VT Need to look at the QT interval and decide whether it is long or normal… If it is long? Is it due to acquired or congenital long QT? If it is normal, then must rule out ischemia and once you have done that, consider Brugada syndrome or Short QT syndrome … Drug induced Long QT TdP Treatment would be…remove the culprit drug, temporary pace at 100 and give magnesium! The End