* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ALH 3205 Professor Cohen 9/02/2009 Cardiac Physiology Anatomy
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Aortic stenosis wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Artificial heart valve wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
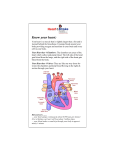
ALH 3205 Professor Cohen 9/02/2009 Cardiac Physiology Anatomy of Heart Middle portion of inferior mediastinum Separates ant/post portions of inferior mediastinum Hollow organ Base- broadest part, superiodorsally directed On top and tipped towards back Apex – pointed end is inferioventral Bottom toward anterior wall of body Origin of great vessels enclosed in Pericardium **Know sections of Pericardium** Fibrous, Pericardial, Visceral…etc. Developed from a pair of blood vessels – embryologically Blood vessels have 3 layers: tunica adventitia, media, interna Therefore, heart has 3 layers: (inside out) Endocardium (inside) – smooth, continuous with vessels that enter and leave the heart To prevent clot formations Myocardium (middle): muscle of the heart, bulkiest layer Myocardium of left ventricle is 4-5x thicker than that of the right ventricle Cardiac muscle is closely related to skeletal muscle – a thicker muscle can develop more force Force a muscle develops is directly related to its cross-sectional area Left ventricle has more force than right ventricle Left ventricle pumps blood to the entire system (thicker = greater force) Right ventricle only pumps blood to lungs (thinner = less force) Epicardium (outer): attached to (and sometimes referred to as) parietal pericardium Walls of heart: Lots of blood vessels, nerves and lymph vessels Collagen fibers w/in walls provide for attachment of cardiac muscles and valves RA RV = tricuspid valve LA LV = bicuspid valve RV and pulmonary trunk = pulmonary semilunar valve LV & aorta = aortic semilunar valve Entering RA = SVC & IVC Entering LA = 4 pulmonary veins Pulmonary trunk bifurcates into R/L arteries NO VALVES between SVC & IVC NO VALVES between the 4 pulmonary veins and the LA Flow into upper chambers in directly related to pressure Pressure > in veins (entering chambers) than LA will enter the LA *If bicuspid valve has stenosed and blood pools in the LA, blood can back up towards the lungs pulmonary edema Fibrous Skeleton – Made of collagen fibers – gives heart structure Electrically isolates the chambers from each other Any spontaneous electrical activity w/in a chamber is isolated in that chamber Electrical Conduction System (in a healthy heart) Origin of heart beat: SA Node (in post. Wall of RA, adjacent to where SJV & IJV enter) Has its own intrinsic rhythm of depolarizing every 8/10 of a second Responsible for the resting heart rate (72 bpm) Some pathways go through interatrial septum: conduct message to the L side of the heart electrical message spreads across very quickly AV Node: ( in RA, near septum) Receives electrical signal from SA Node AV Node holds the electrical message momentarily and releases message into the Bundle of His R Bundle Branch & L Bundle Branch L Bundle Branch (divides into 2 smaller branches) surround heart giving off Purkinje fibers Purkinje fibers – extensions of electrical network on both sides that help distribute electrical discharge through muscles of ventricles when released by AV Node Vasculature System: Capillaries are only exchange vessels in the system (From a classification standpoint) Arteries classified based on function Largest of the Arteries: Elastic arteries bc of high content of elastin in tunica media Closest to pumping action of the heart High content of elastin allows it the receive the high pressure of blood flow directly from heart and rebound that flow further down Ex: Aorta Moving further away from pumping action of the heart = progression of less elastin and more smooth muscle Transition gives rise to muscular arteries Less and less elastin + more smooth muscle (further down) = arteries distributing into capillaries Two major Vessels that supply Myocardium with O2 rich blood Coronary Arteries: L/R Each has a unique distribution Both arise from ascending aorta ONLY blood vessels that come off ascending aorta These arteries arise BEHIND the cusps of the aortic semi-lunar valve When Left Ventricle is in systole and blood is exiting the L ventricle through aortic semilunar valve (semilunar valve is open bc blood is leaving) Openings to coronary arteries are BLOCKED by the aortic valve When left ventricle is in diastole (relaxed)- aortic semilunar valve is closed Coronary arteries are profuse with blood Cardiac Muscle Tissue Similar to Skeletal Muscles Striated, composed of sarcomeres Sarcomeres contain all the same contractile proteins as skeletal muscle Troponin, tropomyosin, actin, myosin Troponin (slightly diff. in cardiac muscle, than skeletal muscle) – used to determine whether cardiac damage is present MAJOR DIFFERENCE: (from skeletal mm) Skeletal muscle stores all calcium it needs to initiate contractile process Cardiac muscle relies (to some degree) on extracellular calcium to excite contractile process IN BOTH: T/T complex blocks active site on actin – takes ionic Ca+ to move T/T sliding filament theory Ca+ channel blockers – reduce force at which the heart contracts, reduces contractile of vascular smooth muscle Both have Sarcomeres (Z Line to Z Line): thin & thick filaments (and cross bridges) Thick and thin filaments must interact Myosin cross bridges must be able to interact Length Tension Relationship – must be a certain length of a sarcomere to produce a contraction IN skeletal: sarcomere is longer Can’t stretch sarcomere out very long or else contraction will not occur DIFFERENCES: (from skeletal mm) Cardiac muscles are short, branched and interconnected Intercalated discs (Gap Junctions) – located between adjacent cells Have electrical resistance about 400 times less than electrical resistance that exists between cells where there is no Gap Junction As a result: electrical impulse can spread quickly across all cells interconnected by Gap Junctions (no delay) Starts in SA Node *Cardiac muscle functions as a syncitium – one large cell* No motor units in Cardiac Muscle Either ALL cells get the signal to contract or none – ALL OR NONE Hearts can contract w/various amounts of force: Can vary the force by changing the thickness of the walls athletes have a thicker left ventricle = slower Stroke Volume Resting sarcomere is must shorter! Can stretch the sarcomere of a cardiac muscle out further and still get a contraction EDV (end diastolic volume): If increased volume in ventricle (before it contracts) it stretches out the walls a little have a greater distance to contract = greater force of contraction All areas of heart are auto-rhythmic – SA Node is spontaneously active Pacemaker Potential – bc membranes of cells that make up the SA Node are not effective at keeping NA+ ions out When NA+ ions enter a cell – change transmembrane potential (In skeletal muscle and in nerve tissue – membrane can keep ions out) Cells of SA Node cannot keep the NA+ out – gradually leak in At Threshold – Fires an action potential Tries to recover (resting membrane potential) – but Na+ is still leaking in so action potential gets fired again what produces the hearts’ beating All cells of heart do this, but SA Node does it at a faster rate Atrial tissue is spontaneously active approx. 60x per min (every 1 sec) As you get further down the heart the rate of action gets lower Action potential Skeletal mm Cardiac mm Rises to about +20 to +30 mv after initial spike exhibits a plateau that lasts bw .25 and .3 seconds the presence of the plateau causes the muscle contraction to have a duration that is somewhere bw 20 and 50 times longer in cardiac mm than in skeletal mm. then rapid repolarization Major differences bw cardiac and skeletal muscle that is responsible for the prolonged muscle contraction and the plateau in the cardiac mm. In skeletal mm. the spike is due to the rapid opening of fast sodium channels Na+ ions rush in a produce Channels close very quickly and Na+ pumped out In cardiac muscle, this electrical activity is due to the opening of TWO type of channels First type are responsible for the upward movement are the same as the open Na+ channels Second type of channels, slow Na+ Ca+ channels open up as soon as the fast Na+ channels begin to close Open later but they stay open longer During this time lasrge amounts of Ca+ and Na+ enter the cell prolonging the depolarization Positives rushing in keeping it in depolarized state At the same time, these Ca+ ions are exciting the contractile process by affect the sarcomeres Immediately after the beginning of the depolarization, the permeability of cardiac muscle cell membrane to K+ decreases about 5 fold At rest more Na+ outside than more K+ inside When you prevent K+ from leaving you trap K+ inside Also contributes to plateau and preventing early recovery When slow Ca+ channels do close, there is a stop to the influx of those ions and the permeability of the membrane returns to normal Refractory period Absolute An excitable tissue when it is absolutely refractory it will not respond to another stimulus Membranes potential is reversed During cardiac plateau it is absolute refractory Relative Membrane will respond to another stimulus iF it is stronger than the normal stimulus Membrane potential is blow zero and returning to -80 The absolute refractory period of ventricular tissue is bw .25 and .3 seconds which is directly equal to the duration of the action potential Due to the calcium channels and the plateau The relative refractory period of ventricular tissue is approx .05 seconds When it can respond to a stronger than normal stimulus Tetanus refraction: short absolute refractory and relative refractory longer where skeletal mm can respond to a stronger and stronger stimulus but in cardiac muscle there is long absolute refractory due to low Na+ Ca+ channels that stay open longer and decreased permeability of K+ Cardiac cycle Repeating pattern of contraction and relaxation of the heart Consists of electrical, mechanical, and acoustical events in that order Electrical always preceeds mechanical, has to be stimulated before an action, then mechanical produces sounds Contraction- systole not depolarization Depolarization results in systole Relaxation- diastole Repolarization leads to diastole Atrial systole occurs is ventricular diatole and ventricular systole occurs during atrial diastole The upper chambers and lower chambers not in systole at the same time CAN be in diastole at the same time Atrial and ventricular diastole Venous return of blood (SVC & IVC into right atrium or pulmonary vein into LA) fills the atrium and bc the AV valves are open fills the ventricles Ventricles are 80% filled with blood due to venous return before atrial systole Atrial systole adds final amount of blood ventricle produce the end diastolic volume [EDV] Volume of blood in the ventricle following atrial systole Contraction of the ventricles at rest ejects about 2/3 of the EDV laving 1/3 behind called the end systolic volume[ESV] Amount left after ventricular systole EDV – ESV= stroke volume The amount of blood left after each beat 100mL – 34mL= 66 mL being ejected from the heart Ejection fraction = SV/EDV= 66% number may be decreased in myopathies LOOK AT THE CHART ON CARDIAC CYCLE!!!!!!!!! QuickTime™ and a decompressor are needed to see this picture. Remember if a pressure above a valve is higher above it opens, if higher below its closed When ventricles loaded with EDV Phase 1: Isovolumetric contraction The volume in the ventricle not changing but it is contracting No blood is moving so AV valves and semilunar valves are closed The pressure inside the ventricle is building bc there is contraction The pressure below the valves is higher so valves stay closed Phase 2: Ejection The moment the pressure in the ventricle exceeds the pressure in the aorta bc then the semilunar valve will open and blood will start to flow out The pressure in the ventricle will reach 120 mmHg even as the ventricular volume decreases and blood is leaving Phase 3: As the pressure of the ventricle eventually starts to falls, back pressure in the aorta closes the semilunar valves and the pressure in the aorta falls to 80 mmHg which the pressure in the ventricle continues to decline all the was to 0mmHg Phase 4: Isovolumetric relaxation All valves closed again and ventricle is relaxing Phase 5: rapid filling Occurs when pressure in the ventricle falls below the pressure in the atrium allowing the bicuspid valve to open and venous return will fill atria and fall through the open AV valves into the ventricles Phase 6: Atrial systole Final volume of blood into ventricles Back at EDV Waves associated with P wave Atrial depolarization Atrial systole after depolarization QRS complex Ventricle depolarization Larger because ventricle is larger than the atria Ventricular systole after depolarization T wave Ventricular repolarization Ventricular diastole after repolarization ST segment is critical During this time is when the ventricles are contracting If there is an ischemic attack then there will be an abnormality in the ST segment Isoelectric: in normal EKG the base line will be fairly even but if problem wont be ELECTRICAL ACTIVITY BEFORE MECHANICAL 5 things you can determine from and EKG Rate Rhythm Axis Electrical position of the heart Depends on circmstance Pregnancy- large abdomen pute pressure on diaphragm and tips heart slightly Hypertrophy Athletic vs clinical Athletes heart thicker due to its working harder Clinical heart is getting thinner even though it looks bigger MI- infarction Acousticals Produced by closing of valves not opening “Lub Dupp” Heart sound number one caused by the closing of the AV valves Ventricles are contracting in systole Heart sound number two caused by closing in semilunar valved Associated with ventricular diastole Sounds of heart bounch of bones and muscles Murmurs- abnormal heart sounds: Produce an abnormal flwo of bloos and an abnormal sound upon auscultation Graded on a 1-6 scale One= nonsignificant 6= extreme Stenosis Valve doesn’t open properly Regurgitation Valve doesn’t close properly Cardiac output= stroke volume [mL/beat] x HR [bpm] Volume of blood ejected by the heart each minute Measured in mL/min Average HR= 72 bpm Average SV = 70-80 mL/beat Average CO = 5000 mL/min Can change Any increase of decrease correlated to a change in HR and/or SV Regulating heart rate Normally both division of the ANS are continuously active to the heart If the nerves are cut completely the heart would continue to beat on own Has auto-rhymicity NE and E: Both increase the rate of the SA node hence they are said to be + chronotropic agents Inc the rate of diastolic repolarization Increase conduction rate through the AV node These same agents also increase the force of both atrial and ventricular contraction making them + inotropic agents Increasing EDV ACH [parasympatheric] Hyperpolarizies the cells of the SA node Decreases the rate Brings further way from threshold Decreases the rate of diatoic repolarization Decreases the rate through the AV node Negative chronotropic agent and negative inotrope Decreases the force of atrial contraction but have no significant effect on the ventricles Regulation of stroke volume EDV: referred to as the preload The volume of blood the ventricle has to work against when it become active SV is directly proportional to preload More blood in ventricle before it contracts the more blood it will be able to pump out SV directly related to contractility Inc blood in ventricle before it contracts the more force it will contract with To effect blood: pressure generated but eh L ventricle must be greater than the average pressure in the arterial system That pressure is a blockade working against ejection bc it is holding the aortic semilunar valve closed Afterload- pressure in the aorta placed on ventricle after they begin to contract SV indirectly proportional to afterload: greater afterload less SV Venous return is important to everything EDV, SV, and Q are all associated with this The mean [average] venous pressure is about 2 mmHg but the pressure at the junction of the SVC and IVC is about .5-0 mmHg Pressure lowest near the right atrium and blood flows from high pressure to low so will move into atrium ANS contracts smooth mm in the walls of large veins Venous pressure will increase facilitation venous return Large veins run through muscles when feeling faint can do muscle exercises to facilitate venous pumping Flow dynamics Flow= change in pressure [P]/resistance [R] Directly related to the change in pressure and indirectly related to its resistance Narrow tube= more resistance=decreased flow Pasallies equation: As the length of a blood vessel increases, we increase the resistance to flow As resistance increases, flow decreases The value cant change Lambda=viscosity of a fluid As viscosity increases the resistance increases flow decreases This value can change bc it is homeostatically regulated Radius of a blood vessel As radius increasesthe resistance will decrease the flow will increase Variable and exponential so has a HUGE effect on the flow The single most powerful flow regulatory mechanism we have is vasoregulation [constriction or dilation] Done by ANS Flow regulated and shunted to necessary areas