* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
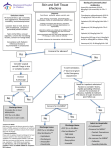
Download PAMC Guideline for OUTPATIENT/EMERGENCY DEPARTMENT
Hepatitis B wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Marburg virus disease wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Leptospirosis wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Schistosomiasis wikipedia , lookup
Antibiotics wikipedia , lookup
Onchocerciasis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Candidiasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Neonatal infection wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
PAMC Guideline for OUTPATIENT/EMERGENCY DEPARTMENT Uncomplicated Skin and Soft Tissue Infection (SSTI) This guideline should NOT be used for the following: Infected diabetic ulcers or ulcers secondary to Human or animal bites Bacteremia associated with skin and soft vascular disease tissue infection Periorbital or orbital cellulitis When concern exists for necrotizing fasciitis IV drug abuse Perineal, vulvar, or perianal infections Deep tissue infection Pregnancy Surgical site infections Critical Illness Note: Presence of complicating risk factors requires alternative treatment strategies and often warrants formal infectious disease consultation. Key Points: The following are NOT routinely indicated for initial management: Beta-hemolytic streptococci are the most common cause of non-purulent cellulitis ESR/CRP MRSA is the most common cause of abscess and purulent skin infections Blood cultures Gram-negative or anaerobic coverage is unnecessary Wound swab, fungal, or AFB cultures The affected area should be elevated Plain films, CT, or MRI Hospital Admission Criteria: Patients should be considered for inpatient admission if any of the following are present: severe disease, failure of outpatient antibiotics, hemodynamic instability, elevated CPK, low serum bicarbonate, severe immune compromise, poor adherence to therapy, or marked left shift. (Refer to PAMC Inpatient Uncomplicated SSTI Clinical Pathway) In a majority of patients who may be treated on an OUTPATIENT basis antibiotics should be given orally. Outpatient IV antibiotic therapy administered via home nursing, the emergency department, and/or infusion centers is generally NOT recommended for patients who do NOT warrant hospital admission. Outpatient Suspected Pathogen(s) Recommended Treatment Other Comments Cellulitis Beta-hemolytic Streptococci Supportive Care: Duration of therapy: 5-7 days WITHOUT (Most commonly Group A, also Elevate affected area purulent Group B, Group C, Group G) Preferred Antibiotic: focus Cephalexin 500 mg – 1 gm PO TID Type-1 Beta-Lactam Allergy: Clindamycin 450 mg PO TID Cellulitis Beta-hemolytic streptococci, Supportive Care: Drainage is the most important WITH Methicillin susceptible intervention. Antibiotics may NOT be I&D - Send purulence for gram-stain/culture purulent Staphylococcus aureus (MSSA), necessary for drained abscesses without Elevate affected area focus Methicillin resistant surrounding induration or erythema. Staphylococcus aureus (MRSA) Preferred Antibiotic: (If Indicated) Duration of therapy: 5-7 days TMP/SMX DS 1 tab PO BID Sulfa Allergy/Type-1 Beta-Lactam Allergy: Note: Recurrent MRSA infections need Clindamycin 450 mg PO TID not be cultured at every presentation. OR Doxycycline 100 mg PO BID Updated 9/2014