* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download cellulitis care map
Survey
Document related concepts
Transcript
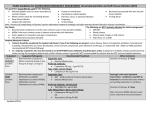
Hôpital régional de Sudbury Regional Hospital CELLULITIS CARE MAP INCLUSION CRITERIA: Acute Mild/Moderate Cellulitis (inflammation & redness) Fever (temperature greater than/equal to 38.0°C) Mild/Moderate Pain associated with Cellulitis EXCLUSION CRITERIA: Chronic Cellulitis Suspected necrotizing fasciitis, osteomyelitis, or septic arthritis Infected diabetic or decubitis ulcers Postoperative wound infections Orbital Cellulitis TESTS (Medical Directive # EDOS01) Bloodwork: CBCD, Electrolytes, Urea, Creatinine, Random Glucose, Calcium Blood Cultures X 2 if temperature greater than/equal to 38.0°C Wound Care swab from infected site Baseline & daily INR level if patient on Warfarin (Coumadin) and receiving fluoroquinolones antibiotics ASSESSMENT Vital Signs (temperature, pulse, blood pressure, respiration, oxygen saturation) Postural Vitals – Lying down for full 5 minutes and Standing (High Fowler’s if unable to stand) for full 2 minutes Mental Status including any changes from baseline Hydration Status (mucus membranes) C/O pain, type and location Affected area of Cellulitis (mark & measure area, drainage) TREATMENT OPTIONS (Medical Directive # EDOS04) Saline lock Intervenous therapy MEDICATIONS*********CHECK ALLERGIES & MEDICATION COMPATIBILITY****** (Medical Directive # EDOS03) FIRST LINE Cephalexin Ceftriaxone SECOND LINE Cloxacillin Clindamycin ORAL 500mg QID X 7 days (max) or until physician r/a PARENTERAL --1gm daily X 7-10 days 500mg QID X 7 days (max) or until physician r/a 300 – 450 mg QID X 7 days (max) or until physician r/a ----- MEDICATIONS*********CHECK ALLERGIES & MEDICATION COMPATIBILITY****** (Medical Directive # EDOS03) Acetaminophen (Tylenol) 325-975mg po (650mg pr) q4hrs prn Hôpital régional de Sudbury Regional Hospital ONGOING MEASURES Review wound care C&S results & adjust medications accordingly Monitor and mark the border of the affected area daily. Notify LTC if affected area is increasing Nutrition – Regular diet or as ordered (encourage fluids unless contraindicated) Activity as tolerated – if non-ambulatory patient ensure repositioning q2hrs Physiotherapy Occupational Therapy REFERENCES Dong, S., Kelly, K., Oland, R., Holroyd, B., Rowe, B. (2001). ED Management of Cellulitis: A review of Five Urban Centers. American Journal of Emergency Medicine, 19(7), 535-540). Murray, H., Stiell, I., & Wells, G. (2005). Treatment failure in emergency department patients with cellulitis. Canadian Journal of Emergency Medicine, 7(4), 228-234. Rosser, W., Pennie, R., Pilla, N., and the Anti-infective Review Panel. (2005). Anti-infective guidelines for community-acquired infections. Toronto: MUMS Guideline Clearinghouse. Seaton, R., Bell, E., Gourlay, Y., & Semple, L. (2005). Nurse-led management of uncomplicated cellulitis in the community: evaluation of a protocol incorporating intravenous ceftriaxone. Journal of Antimicrobial Chemotherapy, 55, 764-767.