* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 2016 Derm Case Studies
African trypanosomiasis wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Antibiotics wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Neonatal infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
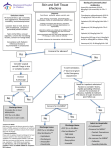
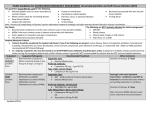
CASE STUDIES IN DERMATOLOGY 2016 NURSING 870 CASE • J.T., A 32 YEAR OLD CAUCASIAN MALE PRESENTS TO HIS PRIMARY CARE PROVIDER WITH C/O A “SPIDER BITE.” THE PATIENT NOTED A REDDENED, PAINFUL AREA UNDER HIS RIGHT ARM X 2 DAYS AGO. HISTORY • WHAT QUESTIONS SHOULD YOU ASK IN THE HISTORY AND ROS? HISTORY • PATIENT NOTED A PAINFUL LUMP IN HIS RIGHT AXILLA X 2 DAYS AGO. THE LUMP APPEARS TO BE GETTING LARGER AND IS NOW PAINFUL AND RED. HE DOES NOT RECALL BEING BIT BY AN INSECT. THERE ARE NOT OTHER SKIN LESIONS AND HE HAS NEVER HAD A LUMP LIKE THIS IN THE PAST. THERE HAVE BEEN NO FEVERS, CHILLS, SWEATS, RASH, JOINT PAIN. OTHER HISTORY • JT HAS NO MEDICAL HISTORY, TAKES NO DAILY MEDICATIONS OR SUPPLEMENTS AND HAS NO KNOWN ALLERGIES TO MEDICATIONS. • SMOKES 1 PPD, DRINKS ALCOHOL ON WEEKENDS, DOES NOT USE ILLICIT DRUGS • LIVES WITH WIFE AND 2 YOUNG CHILDREN; AGES 3 AND 5. • WORKS AS A AN ELECTRICIAN ROS • ALL NEGATIVE IN THE ROS PE • WHAT COMPONENT OF THE PE WOULD YOU PERFORM? PE • VS: 99-88-16, BP 132/82 • SKIN: R AXILLA WITH 4 CM ERYTHEMATOUS LESION, WARM, TENDER. CENTER OF LESION IS RAISED, FLUCTUANT AND POINTING. NO DRAINAGE IS PRESENT • ALL OTHER SYSTEMS WITH NORMAL FINDINGS PE DIFFERENTIAL • WHAT’S YOUR DIFFERENTIAL AT THIS POINT? DIFFERENTIAL • CELLULITIS • ABSCESS • INSECT BITE WHAT’S THE TREATMENT? TREATMENT • I & D IF ABSCESS • POSSIBLE ANTIBIOTICS • HOW IS THE ANTIBIOTIC SELECTED? • WHAT’S THE MOST LIKELY ORGANISM? Purulent skin and soft tissue infections (SSTIs). Dennis L. Stevens et al. Clin Infect Dis. 2014;cid.ciu296 © The Author 2014. Published by Oxford University Press on behalf of the Infectious Diseases Society of America. All rights reserved. For Permissions, please e-mail: [email protected]. TREATMENT IDSA ANTIBIOTIC SUGGESTIONS BY ORGANISM: • GROUP A STREP AND /OR MSSA (METHICILLIN SENS. STAPH AUREUS) CEPHALEXIN 500 MG PO TID X 10 DAYS OR CLINDAMYCIN 300 MG PO TID X 10 DAYS • MRSA: TMP/SMX (BACTRIM DS) 1 PO BID X 10 DAYS OR DOXYCYCLINE 100 MG PO BID X 10 DAYS (PLEASE AVOID CLINDA ALONE AS WE ARE SEEING MRSA RESISTANCE. CAN BE USED AS ADD-ON). • TO COVER BOTH STREP AND MRSA: KEFLEX 500 MG PO TID X 10 DAYS (STREP COVERAGE) PLUS BACTRIM DS OR DOXYCYCLINE TREATMENT • FOLLOW-UP: • 24-48 HOURS FOR IMPROVEMENT • PATIENT EDUCATION • RETURN IF FEVER, EXTENSION OF REDNESS, RED STREAKS • COMPLETE ANTIBIOTICS • PREVENTION OF SPREAD CELLULITIS • SKIN INFECTION OF DERMIS AND SUBQ TISSUES • MOST COMMONLY R/T GROUP B STREP AND STAPH AUREUS (NORMAL IMMUNE STATUS) • GRAM – OR FUNGAL IN IMMUNE COMPROMISED • FACIAL CELLULITIS: H. FLU AND STREP PNEUMONIAE • OTHERS: CONSIDER IF PUNCTURE WOUND, EXPOSURE TO FRESH WATER OR SALT WATER CELLULITIS CELLULITIS: RISK FACTORS • CRACKS IN SKIN • HX OF PVD • INJURY OR TRAUMA TO SKIN • DIABETES • USE OR CORTICOSTEROIDS OR IMMUNE SUPPRESSANTS • WOUND FROM RECENT SURGERY CELLULITIS: SYMPTOMS • FEVER • SIGNS OF INFECTION • PAIN OR TENDERNESS IN THE AREA OF THE RASH OR LESION • SKIN REDNESS OR INFLAMMATION • SKIN LESION OR RASH • SHARP BORDERS • MAY GROW QUICKLY IN FIRST 24 HRS CELLULITIS SYMPTOMS • SKIN MAY APPEAR STRETCHED OR TIGHT • WARMTH OVER AREA OF REDNESS • N/V • MAY BE JOINT STIFFNESS IF OVER JOINT COMPLICATIONS • LYMPHANGITIS • ABSCESS • GANGRENOUS CELLULITIS • NECROTIZING FASCIITIS • BACTEREMIA • SEPSIS CELLULITIS: DIAGNOSTIC TESTS • CBC • BLOOD CULTURE • CULTURE ANY ABSCESS OR DRAINAGE CELLULITIS TREATMENT: ANTIBIOTICS • BASED ON APPEARANCE • IF NO • EMPIRIC COVERAGE FOR STREP AND STAPH AUREUS SHOULD BE PROVIDED • CONSIDER TETANUS STATUS ANTIBIOTICS IDSA ANTIBIOTIC SUGGESTIONS BY ORGANISM: • GROUP A STREP AND /OR MSSA (METHICILLIN SENS. STAPH AUREUS) CEPHALEXIN 500 MG PO TID X 10 DAYS OR CLINDAMYCIN 300 MG PO TID X 10 DAYS • MRSA: TMP/SMX (BACTRIM DS) 1 PO BID X 10 DAYS OR DOXYCYCLINE 100 MG PO BID X 10 DAYS (PLEASE AVOID CLINDA ALONE AS WE ARE SEEING MRSA RESISTANCE. CAN BE USED AS ADD-ON). • TO COVER BOTH STREP AND MRSA: KEFLEX 500 MG PO TID X 10 DAYS (STREP COVERAGE) PLUS BACTRIM DS OR DOXYCYCLINE CELLULITIS TREATMENT • HOSPITALIZATION IF: • SEPSIS • FAILURE TO RESPOND TO TREATMENT • IMMUNE COMPROMISED STATE • PERIORBITAL CELLULITIS SKIN ABSCESS • LOCAL ACCUMULATION OF PUS/DEBRIS • MOST COMMONLY OCCUR IN AXILLAE, GROIN • CONSIDER IF ANY FOREIGN BODY, IV DRUG ABUSE ABSCESS TREATMENT • I & D ALONE FOR SIMPLE ABSCESS • ANTIBIOTIC IF: • GENERALLY > 5 CM • MULTIPLE SITES • RAPID PROGRESSION OR ASSOC. CELLULITIS • SYSTEMIC ILLNESS • IMMUNOSUPPRESSION • EXTREMES OF AGE • FAILURE TO RESPOND TO I & D ALONE • AREA WHERE I & D DIFFICULT ABSCESS: ANTIBIOTICS • SAME AS BEFORE… ABSCESS ANTIBIOTICS • 5-10 DAYS OF TREATMENT • OTHER SELECTIONS FOR HOSPITALIZED PATIENTS AND PEDIATRIC PATIENTS • CONSIDER TETANUS STATUS RECURRENT MRSA? DECOLONIZE! WASH WITH HIBICLENS SOAP IN SHOWER FOR 7 DAYS MUPIRICIN OINTMENT TO NARES BID X 5 DAYS CLEAN HIGH-CONTACT SURFACES AVOID SHARING PERSONAL ITEMS (TOWELS, RAZORS, ETC) BITES • MAY OR MAY NOT BE EVIDENT • TREATMENT IS FOR CURRENT ABSCESS OR CELLULITIS AND RABIES FOR ANIMAL BITES SPECIAL CONSIDERATIONS • DOG BITE • CONSIDER STAPH, STREP, EIKENELLA, OTHERS • CAT BITE • CONSIDER PASTEURELLA, OTHERS • HUMAN BITE ANTIBIOTICS • COVER STAPH, STREP, ANAEROBES, PASTEURELLA • IF PROPHYLACTIC TREATMENT FOR 3-5 DAYS • IF INFECTION TREATMENT FOR 10 DAYS OR LONGER • FIRST LINE TREATMENT: AMOXICILLIN-CLAVULANATE OTHER CONSIDERATIONS • FOR ANIMAL BITES CONSIDER TETANUS STATUS AND POTENTIAL FOR RABIES TREATMENT FOR BITES BY DOGS AND CATS WHOSE RABIES STATUS CAN NOT BE OBTAINED, OR IN FOXES, BATS, RACCOONS, OR SKUNKS IN THE U.S. HIDRADENITIS SUPPURATIVA • RECURRENT INFLAMMATORY DISORDER OF SKIN CONTAINING APOCRINE (SWEAT) GLANDS • TYPICALLY OCCURS IN AXILLAE, UNDER BREASTS & GROIN/ANAL AREA • CHRONIC INFLAMMATORY CONDITION, MORE COMMON IN PATIENTS WHO ALSO EXPERIENCE ACNE • CAN GET SECONDARILY INFECTED WITH BACTERIA (OFTEN STAPH) HIDRADENITIS SUPPURATIVA PATIENT WITH A RASH • 42 Y.O. MALE CALLS YOUR OFFICE FOR HIVES AND AN ITCHY RASH THAT OCCURRED 10 MINUTES AFTER BEING STUNG BY A BEE. HE HAS HIS SON’S EPI-PEN AT HOME. • WHAT ELSE SHOULD YOU ASK TO DETERMINE TREATMENT? QUESTIONS • CLINICAL MANIFESTATIONS OF ANAPHYLAXIS • SKIN • FLUSHING, PRURITIS, URTICARIA, ANGIOEDEMA (UP TO 90% WITH URTICARIA/ANGIOEDEMA) • UPPER RESPIRATORY • CONGESTION, RHINORRHEA • LOWER RESPIRATORY • BRONCHOSPASM, THROAT OR CHEST TIGHTNESS, HOARSENESS, WHEEZING, SOB, COUGH (UP TO 60% WITH LARYNGEAL EDEMA) QUESTIONS • CLINICAL MANIFESTATIONS OF ANAPHYLAXIS • GI • ORAL PRURITIS, CRAMPS, NAUSEA, VOMITING, DIARRHEA • CV • TACHYCARDIA, BRADYCARDIA, HYPOTENSION/SHOCK, ARRHYTHMIAS, ISCHEMIA, CHEST PAIN MYTHS: ANAPHYLAXIS ALWAYS PRESENTS WITH CUTANEOUS MANIFESTATIONS • REALITY • APPROXIMATELY 10-20% OF ANAPHYLAXIS WILL NOT PRESENT WITH HIVES OR OTHER CUTANEOUS MANIFESTATIONS • 80% OF FOOD INDUCED, FATAL ANAPHYLAXIS CASES WERE NOT ASSOCIATED WITH CUTANEOUS SIGNS OR SYMPTOMS (WEBB, ET AL. 2004) MYTH: THE CAUSE OF ANAPHYLAXIS IS ALWAYS OBVIOUS • REALITY • IDIOPATHIC ANAPHYLAXIS IS COMMON • TRIGGERS MAY BE HIDDEN • FOODS • LATEX • PATIENTS MAY NOT RECALL DETAILS OF EXPOSURE SO WHAT SHOULD THIS PATIENT DO? • GO TO THE ED • USE THE EPI-PEN AND GO TO THE ED • USE BENDARYL AND GO TO THE ED • USE THE BENADRYL AND EPI-PEN AND GO TO THE ED OR CLINIC EMERGENCY TREATMENT • IMMEDIATE TREATMENT WITH EPINEPHRINE • NO CONTRAINDICATIONS IN ANAPHYLAXIS • FAILURE OR DELAY ASSOCIATED WITH FATALITIES • IM MAY PRODUCE MORE RAPID, HIGHER PEAK THAN SC • NEED TO HAVE AVAILABLE AT ALL TIMES; EPI-PEN • ANTIHISTAMINE (ORAL OR PARENTERAL, IF ORAL USE LIQUID OR CHEWABLE) • CALL 911; PROCEED TO ED OTHER CONSIDERATIONS • ALLERGY TESTING AND POSSIBLE IMMUNOTHERAPY • DEVELOP EMERGENCY PLAN • EPI-PEN AT ALL TIMES • USE OF ANTIHISTAMINE AND WHEN TO SEEK CARE CASE: PATIENT WITH A RASH • A 64 YEAR OLD FEMALE PRESENTS WITH CC: PAINFUL RASH X 1 DAY HISTORY • BURNING SENSATION TO LEFT ANTERIOR ABDOMEN AND CHEST X 2 DAYS, THEN ONSET OF RASH. RASH ONLY ON CHEST AND ABDOMEN. • ROS: DENIES FEVER. C/O HEADACHE. NO OTHER SYMPTOMS • MEDICAL HISTORY: HYPERTENSION, TYPE 2 DIABETES • MEDICATIONS: METFORMIN, LISINOPRIL • ALLERGIES: NONE PE: RASH WHAT’S THE DIAGNOSIS? DIAGNOSIS • HERPES ZOSTER (SHINGLES) WHAT’S THE TREATMENT? TREATMENT • ACYCLOVIR (AN DERIVATIVES): 7-10 DAYS FOR UNCOMPLICATED CASES • USUALLY STARTED WITHIN 48-72 HOURS OF RASH; THOUGH PT. BENEFIT IF STARTED LATER IN COURSE • DECREASE SEVERITY AND LENGTH OF ILLNESS; MAY PREVENT PHN • CORTICOSTEROIDS • PAIN CONTROL SYMPTOMATIC TREATMENT WHO’S AT RISK? • VZV-SPECIFIC IMMUNITY AND CELL-MEDIATED IMMUNITY, WHICH GENERALLY DECLINES WITH AGE • IMMUNOSUPPRESSION (EG, BY HIV INFECTION OR AIDS) • IMMUNOSUPPRESSIVE THERAPY[ • PRIMARY VZV INFECTION IN UTERO OR IN EARLY INFANCY, WHEN THE NORMAL IMMUNE RESPONSE IS DECREASED • ANTI−TUMOR NECROSIS FACTOR (TNF)-Α AGENTS (MAY POSE AN INCREASED RISK) • IMMUNE RECONSTITUTION INFLAMMATORY SYNDROME (IRIS) • ACUTE LYMPHOCYTIC LEUKMIA AND OTHER MALIGNANCIES EDUCATION • HOW IS SHINGLES PREVENTED? • IS IT “CONTAGIOUS”? • WHAT OTHER TREATMENTS CAN BE ADDED? ANOTHER RASH • 22 YEAR OLD WITH PRURITIS RASH ON THE HANDS AND SPREADING TO THE WRIST X 3 DAYS • NO RECENT ILLNESS • DENIES OTHER SYMPTOMS • HEALTHY ADULT RASH SCABIES • WHAT’S THE CLASSIC PRESENTATION? • HOW IS IT CONTRACTED? • HOW IS IT TREATED? REFERENCES • LUI, C., BAYER, A., COSGROVE, R. DAUM, S.K., FRIDKIN, R., GORWITZ, S.. ET AL. (2011). CLINICAL PRACTICE GUIDELINES BY THE INFECTIOUS DISEASES SOCIETY OF AMERICA FOR THE TREATMENT OF METHICILLIN-RESISTANT STAPHYLOCOCCUS AUREUS INFECTIONS IN ADULTS AND CHILDREN. • WEBB, L., GREENE, E., & LIEBERMAN, P.L. (2004). ANAPHYLAXIS: A REVIEW OF 593 CASES. THE JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY, 113, S240.