* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 1
Survey
Document related concepts
Transcript
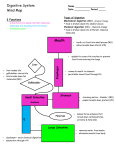
Cadaver dissection videos • http://anatomy.med.umich.edu/courseinfo/vi deo_index.html – Gastrointestinal: http://anatomy.med.umich.edu/gastrointestinal_ system/peritoneum_vid.html 24-1 The Digestive System • Mouth---bite, chew, swallow • Pharynx and esophagus---transport • Stomach----mechanical disruption; absorption of water & alcohol • Small intestine--chemical & mechanical digestion & absorption • Large intestine----absorb electrolytes & vitamins (B and K) • Rectum and anus---defecation 24-2 Layers of the GI Tract 1. Mucosal layer 2. Submucosal layer 3. Muscularis layer 4. Serosa layer 24-3 Mucosa • • • Epithelium – stratified squamous (in mouth, esophagus & anus) = tough – simple columnar in the rest • secretes enzymes and absorbs nutrients • specialized cells (goblet) secrete mucous onto cell surfaces • enteroendocrine cells---secrete hormones controlling organ function Lamina propria – thin layer of loose connective tissue – contains BV and lymphatic tissue Muscularis mucosae---thin layer of smooth muscle – causes folds to form in mucosal layer – increases local movements – movements increase absorption with exposure to “new” nutrients 24-4 Submucosa • Loose connective tissue – containing BV, glands and lymphatic tissue • Meissner’s plexus – parasympathetic – innervation • vasoconstriction • local movement by muscularis mucosa smooth muscle 24-5 Muscularis • Skeletal muscle = voluntary control – in mouth, pharynx, upper esophagus and anus – control over swallowing and defecation • Smooth muscle = involuntary control – inner circular fibers & outer longitudinal fibers – mixes, crushes & propels food along by peristalsis • Auerbach’s plexus (myenteric) – both parasympathetic & sympathetic innervation of circular and longitudinal smooth muscle layers 24-6 Serosa • An example of a serous membrane • Covers all organs and walls of cavities not open to the outside of the body • Secretes a serous fluid • Consists of connective tissue covered with simple squamous epithelium 24-7 Peritoneum • Peritoneal cavity – potential space containing a bit of serous fluid – Contains most of the digestive organs • A sheet of serosa forms the peritoneal cavity • Serosa is known as the Peritoneum – Cavity within the abdomen that contains the viscera – Formed by a parietal layer – visceral layer covers organs 24-8 The 4 Mesenteries • Serosa also forms connections from the parietal peritoneum to several organs in the cavity = Mesenteries • 4 kinds: • Mesentery – parietal peritoneum to small intestines • Mesocolon – parietal peritoneum to large intestine (colon) • Lesser omentum • Greater omentum 24-9 The path of food: oral cavity/teeth/salivary glands oropharynx/epiglottis esophagus stomach small intestine: duodenum small intestine: jejunum small intestine: ileum large intestine: ascending colon large intestine: transverse colon large intestine: descending colon sigmoid colon rectum anus 24-10 Mouth • Oral cavity proper---the roof = hard, soft palate and uvula – floor – geniohyoid, mylohyoid – contains the tongue – lips and cheeks-----contains buccinator muscle that keeps food between upper & lower teeth – Vestibule---area between cheeks and teeth • Lined with an oral mucosa (stratified squamous epithelium & lamina propria) – Lining of the cheeks = buccal mucosa – Lining of the maxilla and mandible = alveolar mucosa (gingiva) • Landmarks: lingual frenulum, labial frenulum, uvula 24-11 – Shortened lingual frenulum can impede movement of the tongue within the mouth Tubal tonsil Nasopharynx Geniohyoid Oropharynx Mylohyoid Laryngopharynx Larynx Lingual tonsil Epiglottis Vocal cords Pharyngeal Arches • Two arches skeletal muscles that elevate the soft palate when we swallow – Closes off the nasopharynx and directs food into the oropharynx • First arch = Palatoglossal muscle – extends from palate down to tongue – uvula dangles from the middle of this arch – forms the boundary between the oral cavity and oropharnyx • Second arch = Palatopharyngeal muscle – extends from palate to pharyngeal wall – part of the oropharynx – found behind the palatine tonsil 24-13 Structure and Function of the Tongue • Muscular structure covered with an oral mucosa • Muscle of tongue is attached to hyoid, mandible, hard palate and styloid process • Two groups of muscles • 1. Intrinsic muscles – Change the shape of the tongue – Organized as transverse muscles, longitudinal and vertical muscles • 2. Extrinsic muscles – move the tongue in the oral cavity – Styloglossus, palatoglossus & hyoglossus – Geniohyoid & genioglossus 24-14 Salivary Glands • Parotid below your ear and over the masseter • Submandibular is under lower edge of mandible • Sublingual is deep to the tongue in floor of mouth • All have ducts that empty into the oral cavity (exocrine glands) • Classified either as: serous or mixed • Wet food for easier swallowing • • Dissolves food for tasting • Bicarbonate ions buffer acidic foods • • Helps build stronger enamel • Chemical digestion begins with enzyme salivary amylase & lingual lipase • Also contains lysozyme ---helps destroy bacteria • Protects mouth from infection with its rinsing action Serous glands - cells secrete a watery fluid – e.g. parotid Mixed glands secrete both mucus and a serous fluid – e.g. submandibular & sublingual 24-15 • Parotid gland secretes the enzyme Salivary amylase • Submucosa layer of the tongue secretes Lingual lipase Parotid Sublingual Submandibular 24-16 Salivation • Parasympathetic nerves - Increase salivation – sight, smell, sounds, memory of food, tongue stimulation---rock in mouth – cerebral cortex signals the salivatory nuclei in brainstem – carried by parasympathetic nerves = CN 7 & 9 • Sympathetic nerves - Stop salivation – dry mouth when you are afraid – sympathetic nerves 24-17 Teeth: -grinding, tearing and shearing of food -two main divisions: crown and root -crown: above gumline/gingiva -covered with a layer of enamel -root: below the gumline, embedded in the alveolar socket of the jaw -entry of nerves and blood vessels via the apical foramen -root is secured in the jaw by two tissues: cementum & periodontal membrane/ligament -neck – where crown and root meet -gingiva should form a tight a seal at this area -inside of the tooth = pulp (nerves/blood vessels) -nerves and BVs enter the root via apical foramen and travel through root canals to enter the pulp cavity -tooth is formed of a calcified connective tissue called dentin -dentin, enamel and cementum – made of calcium phosphate very similar to bone 24-18 Primary and Secondary Dentition -primary: 20 teeth starting at 6 months -secondary/adult: between 6 and 12 years = 32 teeth 8 incisors 4 canines (cuspids) 8 premolars (bicuspids) 12 molars (tricupids) ** third pair of molars (wisdom teeth) may not erupt -impacted 24-19 Pharynx • Funnel-shaped tube extending from internal nares to the esophagus (posteriorly) and larynx (anteriorly) • Skeletal muscle lined by mucous membrane • Deglutition or swallowing is facilitated by saliva and mucus – starts when bolus is pushed into the oropharynx – sensory nerves send signals to deglutition center in brainstem 24-20 Esophagus • • • • • Collapsed muscular tube In front of vertebrae Posterior to trachea Posterior to the heart Pierces the diaphragm at hiatus – hiatal hernia or diaphragmatic hernia • Mucosa = stratified squamous • Submucosa = large mucous glands • Muscularis = upper 1/3 is skeletal, middle is mixed, lower 1/3 is smooth – upper & lower esophageal sphincters are prominent circular muscle 24-21 Thoracic Aorta Esophagus Diaphragm Liver 24-22 Physiology of the Esophagus - Swallowing • • Voluntary phase---tongue pushes food to back of oral cavity Involuntary phase----pharyngeal stage – breathing stops & airways are closed – soft palate & uvula are lifted to close off nasopharynx – vocal cords close – epiglottis is bent over airway as larynx is lifted – controlled by autonomic nervous system • Peristalsis pushes food down – circular fibers behind bolus – longitudinal fibers in front of bolus shorten the distance of travel • • Travel time is 4-8 seconds for solids and 1 sec for liquids Lower sphincter relaxes as food approaches 24-23 Gastroesophageal Reflex Disease • If lower esophageal sphincter fails to open – distension of esophagus feels like chest pain or heart attack • If lower esophageal sphincter fails to close – stomach acids enter esophagus & cause heartburn (GERD) – for a weak sphincter---don't eat a large meal and lay down in front of TV – smoking and alcohol make the sphincter relax worsening the situation • Control the symptoms by avoiding – coffee, chocolate, tomatoes, fatty foods, onions & mint – take Tagamet HB or Pepcid AC 60 minutes before eating – neutralize existing stomach acids with Tums 24-24 Anatomy of Stomach • Size when empty – large sausage – stretches due to rugae (folds in the mucosa caused by contraction of the m. mucosae) • Muscularis – three layers of smooth muscle – longitudinal – circular – oblique • Parts of stomach – – – – Cardiac region Fundus Dody Pyloric region---starts to narrow as approaches pyloric sphincter - Greater curvature - Lesser curvature • Bolus of food enters and mixes with gastric juice Chyme • Stomach empties as small squirts of chyme leave the stomach through the pyloric valve/sphincter 24-25 FUNDUS BODY PYLORIC REGION PANCREAS DUODENUM Mucosa of the Stomach • • • • • • • simple columnar epithelium with embedded mucus cells Mucosa forms columns of secretory cells = gastric glands that open into the stomach lumen through gastric pits Chief cells secrete pepsinogen (inactive) into the stomach which will become pepsin (active) – for protein digestion Parietal cells secrete H+ and Cl- ions into the stomach – become Hydrochloric acid HCl converts pepsinogen into pepsin = protein digestion Intrinsic factor (parietal cells) – absorption of vitamin B12 for RBC production Gastrin hormone (G cells) • Increases gastric juice production, gastric motility and increase gastric emptying 24-27 Anatomy of the Small Intestine • 20 feet long----1 inch in diameter • Large surface area for majority of absorption • 3 parts – duodenum---10 inches – jejunum---8 feet – ileum---12 feet • ends at ileocecal valve 24-28 Lesser Omentum Liver Stomach Gallbladder Transverse Colon Ascending Colon Descending Colon Mesentery of Small Intestine Small Intestine 24-29 Small Intestine • Structures that increase surface area – plica circularis • permanent ½ inch tall folds in the mucosa • not found in lower ileum • cannot stretch out like rugae in stomach – villi • 1 Millimeter tall • Core is lamina propria of mucosal layer • Contains vascular capillaries and lacteals (lymphatic capillaries) – microvilli • Found on the apical surface of absorptive cells • Gives the villus the appearance of a brush border 24-30 Small intestine - Mucosa • Absorptive cells -project their microvilli into the lumen of the SI -absorb amino acids and saccharides from food • Epithelial cells at the bottom of the villus form a gland = Intestinal gland – production of intestinal juice or brush-border enzymes • Submucosal layer has duodenal glands secretes alkaline mucus • Goblet cells – mucus production • Enteroendocrine cells – Found within the intestinal glands – Secrete three hormones – secretin – cholecystokinin – gastric inhibitory peptide • Paneth cells – secretes lysozyme – kills bacteria Anatomy of Large Intestine • • • • • 5 feet long by 2½ inches in diameter Ascending & descending colon are retroperitoneal (not in the peritoneal cavity) Cecum & appendix Rectum = last 8 inches of GI tract anterior to the sacrum & coccyx Anal canal = last 1 inch of GI tract – internal sphincter----smooth muscle & involuntary – external sphincter----skeletal muscle & voluntary control 24-32 Histology of Large Intestine • Muscular layer – internal circular layer is normal – outer longitudinal muscle can be seen from the outside • taeniae coli = shorter bands • Permanent contractions of these bands puckers the LI into pouches called haustra (also called diverticula) • epiploic appendages • Serosa = visceral peritoneum 24-33 Histology of Large Intestine • Mucosa – smooth tube -----no villi – intestinal glands found in the mucosa – simple columnar cells absorb water & goblet cells secrete mucus • Submucosal & mucosa contain lymphatic nodules 24-34 Defecation • Reflex moves feces into rectum • Stretch receptors signal to the sacral spinal cord • Parasympathetic nerves contract muscles of rectum & relax internal anal sphincter • External sphincter is voluntarily controlled 24-35 Anatomy of the Pancreas • 5" long by 1" thick • Head close to curve in C-shaped duodenum • pancreatic duct joins common bile duct from liver • Opens 4" below pyloric sphincter 24-36 Pancreatic Juice • 1 + 1/2 Quarts/day at pH of 7.1 to 8.2 • Contains water, enzymes & sodium bicarbonate • Digestive enzymes: – pancreatic amylase, pancreatic lipase, proteases (protein degradation) – Ribonuclease & deoxyribonuclease - digest nucleic acids 24-37 The 4 Proteases Enterokinase (intestines) – trypsinogen--Trypsinogen Trypsin activated by enterokinase (a brush border enzyme) Trypsin – chymotrypsinogen---- Chymotrypsinogen Chymotrypsin activated by trypsin – procarboxypeptidaseactivated by trypsin – proelastase--Trypsin Proelastase Elastase activated by trypsin Procarboxypeptidase Trypsin Carboxypeptidase 24-38 Anatomy of the Liver and Gallbladder • Liver – – – – weighs 3 lbs. below diaphragm right lobe larger gallbladder on right lobe – size causes right kidney to be lower than left • Gallbladder – fundus, body & neck 24-39 Right & Left Hepatic Ducts Common Hepatic Duct Pancreatic Duct Gallbladder Cystic Duct Ampulla of Vater Common Bile Duct 24-40 Blood Supply to the Liver • Hepatic portal vein – nutrient rich blood from stomach, spleen & intestines – splenic vein + superior mesenteric vein + inferior mesenteric vein • Hepatic artery branches off the Common hepatic artery (from the celiac trunk) Hepatic Portal Vein Common Bile Duct Splenic Vein Superior Mesenteric Vein Inferior Mesenteric Vein 24-41 Histology of the Liver • Hepatocytes arranged in lobules • Sinusoids in between hepatocytes are blood-filled spaces • Kupffer cells phagocytize microbes & foreign matter 24-42 • • • • Lined with simple columnar epithelium No submucosa Three layers of smooth muscle For the production of Bile • Gallbladder role in the absorption of fats • Stimulated by the presence of fat in the duodenum • Fat stimulates CCK production by SI which stimulates contraction of the gallbladder and the release of bile Flow of Bile • Bile capillaries • Hepatic ducts connect to form common hepatic duct • Cystic duct from gallbladder & common hepatic duct join to form common bile duct • Common bile duct & pancreatic duct empty into duodenum 24-43 Types of Digestion • Mechanical – mouth, stomach, SI, LI • Chemical – mouth, stomach, SI 24-44 Chemical Digestion in GI tract Digestion of Carbohydrates • Mouth---salivary amylase • Esophagus & stomach---nothing happens • Duodenum----pancreatic amylase • Brush border enzymes (maltase, sucrase & lactase) act on disaccharides – these enzymes produce the monosaccharides fructose, glucose & galactose – lactose intolerance (no enzyme; bacteria ferment sugar)--gas & diarrhea Digestion of Proteins • Stomach – HCl denatures or unfolds proteins – pepsin turns proteins into peptides • Pancreas – Proteases --split peptides into smaller peptides and dipeptides • Intestines – brush border enzymes----aminopeptidase or dipeptidase-----split off amino acid at amino end of a peptide (aminopeptidase) or split dipeptides into individual amino acids (dipeptidase) Digestion of Lipids • Mouth----lingual lipase • Small intestine – emulsification by bile – pancreatic lipase--splits into fatty acids & monoglyceride – no enzymes in brush border Digestion of Nucleic Acids • Pancreatic juice contains 2 nucleases – ribonuclease which digests RNA – deoxyribonuclease which digests DNA • Nucleotides produced are further digested by brush border enzymes (nucleosidease and phosphatase) – pentose, phosphate & nitrogenous bases 24-46 Digestion in the Mouth • Mechanical digestion (mastication or chewing) • breaks into pieces • mixes with saliva so it forms a bolus • Chemical digestion – salivary amylase • begins starch digestion at pH of 6.5 or 7.0 found in mouth • when bolus & enzyme hit the pH 2.5 gastric juices hydrolysis ceases – lingual lipase • secreted by glands in tongue – Ebner’s glands • begins breakdown of triglycerides into fatty acids and glycerol 24-47 Stomach--Mechanical Digestion • Gentle mixing waves – every 15 to 25 seconds – mixes bolus with 2 quarts/day of gastric juice to turn it into chyme (a thin liquid) • More vigorous waves – travel from body of stomach to pyloric region • Intense waves near the pylorus – open it and squirt out 1-2 teaspoons full with each wave 24-48 Stomach--Chemical Digestion • Protein digestion begins – HCl denatures (unfolds) protein molecules – HCl transforms pepsinogen into pepsin that breaks peptides bonds between certain amino acids • Fat digestion continues – gastric lipase splits the triglycerides in milk fat • most effective at pH 5 to 6 (infant stomach) • HCl kills microbes in food • Mucous cells protect stomach walls from being digested with 1-3mm thick layer of mucous 24-49 Absorption of Nutrients by the Stomach • • • • Water especially if it is cold Electrolytes Some drugs (especially aspirin) & alcohol Fat content in the stomach slows the passage of alcohol to the intestine where absorption is more rapid • Gastric mucosal cells contain alcohol dehydrogenase that converts some alcohol to acetaldehyde-----more of this enzyme found in males than females • Females have less total body fluid that same size male so end up with higher blood alcohol levels with same intake of alcohol 24-50 Mechanical Digestion in the Small Intestine • 1. Weak peristalsis in comparison to the stomach---chyme remains in SI for 3 to 5 hours – starts at the lower portion of the stomach and pushes the chyme forward – reaches the end of the ileum after 90 – 120 minutes – then another wave starts in the stomach • 2. Segmentation---local mixing of chyme over the surface of the absorptive cells in the SI – does NOT push the food through the SI – moves chyme back and forth within a segment of the SI – done in specific segments – most rapid in the duodenum and slows at it reaches the ileum Small Intestine-Chemical Digestion - Mucosal layer forms Intestinal glands = Crypts of Lieberkuhn - Glands secretes intestinal juice or brush border enzymes -sucrase, maltase, lactase, dextrinase – dissacharides -aminopeptidase or dipeptidase – peptides -phosphatase - nucleic acids -enterokinase – trypsin activation Small Intestine-Chemical Digestion -duodenum is also the site for secretion of the Pancreatic juice: -trypsin, chymotrypsin, elastase, carboxypeptidase -1-2 qt./day------ at pH 7.6 -enzymes are made in the pancreas as inactive forms eg. trypsinogen, chymotrypsinogen, proelastase, procarboxypeptidase -trypsin synthesized as trypsinogen - converted to trypsin by the enzyme enterokinase (brush border enzyme) -activated trypsin then converts others into their active forms Mechanical Digestion in Large Intestine • Done by the smooth muscle • Peristaltic waves (3 to 12 contractions/minute) – haustral churning----relaxed pouches are filled from below by muscular contractions (elevator) – gastroilial reflex = when stomach is full, gastrin hormone relaxes ileocecal sphincter so small intestine will empty and make room – gastrocolic reflex = when stomach fills, a strong peristaltic wave moves contents of transverse colon into rectum 24-54 Chemical Digestion in Large Intestine • No human digestive enzymes are secreted by the LI • only mucous – by the Goblet cells in the intestinal glands • Chyme that leaves the SI is acted upon by the action of bacteria (E.coli) • Bacteria actions: – ferment undigested carbohydrates carbon dioxide & methane gas – breakdown undigested proteins - simpler substances (indoles, skatoles, hydrogen sulfide)----odor – turn bilirubin into simpler substances that produce color • Bacteria produce vitamin K and B in colon 24-55 Absorption & Feces Formation in the Large Intestine • food has now been in the GI tract for 3 to 10 hours • solid or semisolid due to water reaborption = feces • feces – water, salts, sloughed-off epithelial cells, bacteria, products of bacterial decomposition, unabsorbed and undigested materials • 90% of all water absorption takes place in the SI – 10% in the LI • but the LI is very important in maintaining water balance • also absorbs some electrolytes---Na+ and Cl- and vitamins • dietary fiber = indigestible plant carbohydrates (cellulose, lignin and pectin) • soluble fiber – dissolves in water (beans, barley, broccoli, prunes, apples and citrus) – forms a gel that slows the passage of materials through the colon – also helps to lower blood cholesterol – binds to bile salts to prevent their reabsorption – liver must make more cholesterol to make more bile salts – takes this cholesterol from the blood • insoluble fiber – woody or structural parts of the plant (skins of fruits and vegetables, coatings around bran and corn) – passes though the colon relatively unchanged 24-56 Where will the absorbed nutrients go? 24-57 Absorption of Water • 9 liters of fluid dumped into GI tract each day • Small intestine reabsorbs 8 liters • Large intestine reabsorbs 90% of that last liter • Absorption is by osmosis through cell walls into vascular capillaries inside villi 24-58 Liver Functions--Carbohydrate Metabolism • Turn proteins into glucose • Turn triglycerides into glucose • Turn excess glucose into glycogen & store in the liver • Turn glycogen back into glucose as needed Liver Functions --Lipid Metabolism • Synthesize cholesterol • Synthesize lipoproteins----HDL and LDL (used to transport fatty acids in bloodstream) • Stores some fat • Breaks down some fatty acids Liver Functions--Protein Metabolism • Deamination = removes NH2 (amine group) from amino acids • Converts resulting toxic ammonia (NH3) into urea for excretion by the kidney • Synthesizes plasma proteins utilized in the clotting mechanism and immune system • Convert one amino acid into another 24-59 Other Liver Functions • Detoxifies the blood by removing or altering drugs & hormones (thyroid & estrogen) • Releases bile salts help digestion by emulsification • Stores fat soluble vitamins-----A, B12, D, E, K • Stores iron and copper • Phagocytizes worn out blood cells & bacteria • Activates vitamin D (the skin can also do this with 1 hr of sunlight a week) 24-60 Gallbladder • • • • Simple columnar epithelium No submucosa Three layers of smooth muscle Serosa or visceral peritoneum Bile Production • One quart of bile/day is secreted by the liver – yellow-green in color & pH 7.6 to 8.6 • Components – water & cholesterol – bile salts = Na & K salts of bile acids – bile pigments (bilirubin) from hemoglobin molecule Flow of Bile • Bile capillaries • Hepatic ducts connect to form common hepatic duct • Cystic duct from gallbladder & common hepatic duct join to form common bile duct • Common bile duct & pancreatic duct empty into duodenum 24-61