* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Isolation of Monocyte/Macrophage Populations
Survey
Document related concepts
Transcript
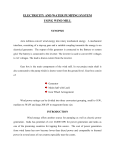
UNIT 7.6 Isolation of Monocyte/Macrophage Populations The following basic and alternate protocols describe the isolation of monocytes from lymphocytes by adherence, gradient sedimentation on colloidal silica particles, and flow cytometry. Because the first two methods can result in cell activation (induction of gene expression or protein secretion), and the third is technically difficult, a fourth protocol is presented which describes counterflow centrifugal elutriation. This latter procedure can be used to isolate large numbers of purified, nonactivated monocytes. Flow cytometry methods for measuring the expression of membrane determinants to characterize the phenotypic profiles of monocytes and macrophages can be found in UNIT 14.3; functional assays using isolated monocytes/macrophages (e.g., assays of oxidative metabolism, phagocytosis, and anti-viral and anti-tumor activities) are also covered in Chapter 14. CAUTION: When working with human blood, cells, or infectious agents, biosafety practices must be followed (see Chapter 7 introduction). NOTE: All solutions and equipment coming into contact with cells must be sterile, and proper sterile technique must be used accordingly. BASIC PROTOCOL ISOLATION OF MONOCYTES BY ADHERENCE In this protocol, monocytes are isolated from mononuclear cells by exploiting their ability to adhere to glass or plastic. This is a quick and easy procedure, but it can induce cell activation (see background information). Materials Peripheral blood mononuclear cells (PBMC; UNIT 7.1) Serum-free DMEM (e.g., GIBCO/BRL #320-1960), supplemented with 2 mM L-glutamine and 50 µg/ml gentamycin 0.02% EDTA in PBS (APPENDIX 2; low pyrogen and without Ca++ or Mg++) 75-cm2 tissue culture flasks (Falcon #3023) Beckman GPR centrifuge with GH-3.7 horizontal rotor (or equivalent) 15-ml conical polypropylene centrifuge tube Additional reagents and equipment for cell counting (APPENDIX 3) 1. Suspend PBMC in supplemented serum-free DMEM at 2 × 106 cells/ml. 2. Add 10 ml of the cell suspension to each 75-cm2 flask and incubate 1 hr in a humidified 37°C, 5% CO2 incubator. Some investigators add 10% autologous human serum (Edelson and Cohn, 1976) or 10% pooled human serum (Gartner et al., 1986) to DMEM during the initial adherence step. Although cells adhere in the presence of serum, they adhere more quickly in its absence. 3. Decant the medium which contains nonadherent cells, wash twice with 10 ml supplemented serum-free DMEM to remove any residual nonadherent cells, and replace with 10 ml fresh DMEM. 4. Remove adherent monocytes by gently scraping with a plastic cell scraper or by incubating the cells in ice-cold 0.02% EDTA/PBS solution for 10 min followed by firmly tapping the flask. Transfer cells to a 15-ml conical tube and centrifuge 10 min in GH-3.7 rotor at 1400 rpm (300 × g) to remove the EDTA/PBS solution. Isolation of Monocyte/ Macrophage Populations 5. Resuspend in supplemented serum-free DMEM and count monocytes. Alternatively, monocytes can be adhered in the appropriate culture plate and used directly. 7.6.1 Supplement 16 CPI Copyright © 1995 by John Wiley & Sons, Inc. ISOLATION OF MONOCYTES BY SIZE SEDIMENTATION In this procedure, monocytes are isolated from cell suspensions by size sedimentation using a continuous gradient of colloidal silica particles (Gmelig-Meyling and Waldmann, 1980). This avoids the adherence step of the previous protocol. Nevertheless, activation of monocytes is still possible (see background information). BASIC PROTOCOL Materials Fetal calf serum (FCS; heat-inactivated 1 hr, 56°C) Peripheral blood mononuclear cells (PBMC; UNIT 7.1) Hanks balanced salt solution (HBSS; APPENDIX 2) containing 10% FCS Percoll (specific gravity 1.130 g/ml, 17 mosM/kg; Pharmacia #17-0891-01) 2× PBS (GIBCO/BRL #310-4200AJ or APPENDIX 2) Sorvall RC2-B centrifuge with SS-34 fixed-angle rotor (or equivalent) Beckman GPR centrifuge with GH-3.7 horizontal rotor (or equivalent temperature-controlled centrifuge) 15-ml conical polypropylene centrifuge tube 15-ml polycarbonate centrifuge tube (Sorvall #00770) 1. Place 3 ml FCS in a 15-ml centrifuge tube and carefully overlay with PBMC. Centrifuge 15 min in a GH-3.7 rotor at 800 rpm (200 × g), 18° to 20°C. Discard supernatant, which contains platelets. Resuspend pellet in HBSS/FCS at 2-5 × 107 cells per 1 to 2 ml. 2. In a 15-ml polycarbonate centrifuge tube, add 7 ml Percoll to 6 ml of 2× PBS. Centrifuge 40 min in Sorvall SS-34 rotor at 15,000 rpm (21,000 × g), room temperature, to form the continuous gradient. 3. Gently layer the platelet-free mononuclear cells from step 1 onto preformed gradient. 4. Centrifuge 20 min in GH-3.7 rotor at 2400 rpm (1000 × g), 4°C. 5. Using sterile Pasteur pipets, carefully collect the four opaque bands of cells beginning at the top. Band 1 contains dead cells, debris, and a few platelets. Band 2 contains monocytes, a few lymphocytes, and any remaining platelets. Band 3 contains lymphocytes, and a few monocytes. Band 4 contains granulocytes and RBC. 6. Wash and count the cells in band 2 (APPENDIX 3). Monocytes comprise 70% to 90% of band 2. ISOLATION OF MONOCYTES BY FLOW CYTOMETRY In this protocol, monocytes are separated from mononuclear cell populations by flow cytometry. Although minimal activation is caused by this method, the flow cytometer can be difficult to use. Materials Peripheral blood mononuclear cells (PBMC; UNIT 7.1) PBS (APPENDIX 2), without and with 10% AB serum (heat-inactivated 1 hr, 56°C) Serum/azide solution: 0.1% NaN3 and 2% FCS in PBS Azide solution: 0.1% NaN3 in PBS 10 µg/ml monocyte-specific monoclonal antibody in serum/azide solution (e.g., Leu M3 or Leu M5; Becton Dickinson) Serum-free DMEM (e.g., GIBCO/BRL #320-1960), supplemented with 2 mM L-glutamine and 50 µg/ml gentamycin Beckman GPR centrifuge with GH-3.7 horizontal rotor (or equivalent) BASIC PROTOCOL Immunologic Studies in Humans 7.6.2 Current Protocols in Immunology Additional reagents and equipment for immunofluorescent staining (UNIT 5.3) and flow cytometry (UNIT 5.4 & 7.9) 1. Suspend PBMC in PBS and centrifuge 10 min in a GH-3.7 rotor at 1400 rpm (300 × g), 4°C. Aspirate and discard the supernatant. 2. Resuspend the pellet in PBS containing 10% AB serum and incubate 10 min at 4°C. Centrifuge 10 min at 300 × g, 4°C, to pellet cells. This step blocks nonspecific binding of MAb to surface Fc receptors. 3. Resuspend pellet at 1.0-1.5 × 107 cells/ml in serum/azide solution containing 10 µg/ml monocyte-specific MAb. Incubate 20 min at 4°C. If the MAb reacts with surface determinants on other cells, the purity of the sorted cells will be reduced. Leu M3 and Leu M5 are monocyte-specific and have low cross-reactivity with other cell types. In addition, they do not cause monocyte activation. 4. Centrifuge cells 10 min at 300 × g, 4°C. Wash cells by resuspending in 3 ml azide solution, and centrifuging 3 min at 300 × g, 4°C. 5. Resuspend the cells in supplemented serum-free DMEM at ≥1 × 106 cells/ml. 6. Sort by flow cytometry. 7. Resuspend monocytes in supplemented serum-free DMEM and keep on ice prior to use. BASIC PROTOCOL ISOLATION OF MONOCYTES BY COUNTERFLOW CENTRIFUGAL ELUTRIATION Counterflow centrifugal elutriation (CCE) is a highly effective method for separating large numbers of monocytes from Ficoll-Hypaque purified PBMC (UNIT 7.1). The protocol has four parts: assembly of the CCE system, preparation of mononuclear cells for CCE, loading of mononuclear cells, and isolation of monocytes by CCE. In contrast to the adherence and sedimentation methods of isolation, this procedure does not lead to monocyte activation. Materials 70% ethanol Phosphate-buffered saline (PBS; APPENDIX 2) low pyrogen and without Ca++ and Mg++ Peripheral blood mononuclear cells (PBMC; UNIT 7.1) Isolation of Monocyte/ Macrophage Populations Beckman elutriation system: J-6M elutriation centrifuge with JE-6B rotor, strobe, and standard elutriation chamber(s) Tissue culture hood (biosafety cabinet) 2-ml pipet Silastic tubing, 1⁄4 × 118–in. Masterflex pump (1 to 100 rpm, 10-turn potentiometer, 115 VAC with 7014 pump head, Cole-Parmer #N-07520-35 and silicone tubing, #F6411-14, respectively) Ring stand and holder Beckman GPR centrifuge with GH-3.7 horizontal rotor (or equivalent) Coulter counter with channelyzer 10-ml pipet or 10-ml syringe 50-ml polypropylene centrifuge tubes Additional reagents and equipment for Ficoll-Hypaque cell separation (UNIT 7.4), flow cytometry (UNIT 5.4), and nonspecific esterase staining (APPENDIX 3) 7.6.3 Current Protocols in Immunology Assemble the elutriation system 1. Assemble the elutriation rotor and the strobe setup according to the manufacturer’s instructions. Before attaching the seal housing, be sure that the spring forces the rotating seal against the seal housing by pressing the rotating seal down on the shaft. The spring should force the rotating seal back up when the pressure is released. 2. Assemble the inlet line from a tissue culture hood to the rotor in the centrifuge as shown in Figure 7.6.1. Connect a 2-ml pipet to silastic tubing and attach this tubing to the silicone tubing on the inlet side of the Masterflex pump. Assemble the sample reservoir using silastic tubing as shown in Figure 7.6.2A. Connect the silicone tubing on the outlet side of the pump to the silastic tubing on the sample reservoir setup as shown in Figure 7.6.1. The setup for the sample reservoir (Fig. 7.6.2) differs from that suggested by the manufacturer. An additional three-way valve has been added, and the position of the needles is reversed. This allows the sample chamber to be used as a bubble trap and a pulse dampener during elutriation and, as discussed below, as a mechanism to slowly introduce the cells into the elutriation chamber(s) at a controlled flow rate. A 70-ml sample chamber is shown in this setup; however, a 30-ml chamber can be used in the same manner. Also note that the pressure indicator supplied with this equipment (to detect pressure buildup as a result of air bubbles) has been eliminated due to contamination that can occur in its housing. Problems with back pressure can be eliminated by ensuring that there are no bubbles in the system (see below) and by using the sample reservoir as a bubble trap during the run. 3. Connect the silastic outlet line from the rotor to the silicone tubing as described by the manufacturer. Route this tubing back to the tissue culture hood, connect it to a 2-ml pipet with a short piece of silastic tubing, and attach the pipet to a holder on a ring stand (Fig. 7.6.1). 4. To sterilize the elutriation system, place the pipet on the inlet line into a beaker containing 300 ml of 70% ethanol and turn the pump on at flow rate of 5 to 8 ml/min. (Use the settings on the 10-turn potentiometer of the pump corresponding to flow rates between 5 and 19 ml/min.) Turn the three-way valves to positions that will initially bypass the sample reservoir. Once the ethanol has gone through the system and is being collected in a beaker under the pipet connected to the outlet line, manually spin the rotor clockwise until all of the air in the chambers in the rotor has been removed. Remove the sample reservoir, leave the needles connected to the tubing, Culture hood J-6M elutriation centrifuge silicone silastic tubing tubing sample reservoir setup silicone tubing pump silastic tubing 10turn potentiometer 1 liter of PBS ice elutriation JE-6B chamber elutriator rotor Figure 7.6.1 Design of counterflow centrifugal elutriation system. Immunologic Studies in Humans 7.6.4 Current Protocols in Immunology and run 70% ethanol through each side of the setup by opening and closing the appropriate three-way valves. Then turn the three-way valves so that the sample setup is by-passed again, and continue to pump the remaining ethanol through the system. 5. After the ethanol wash, place the inlet pipet in PBS, and pump 400 ml through the elutriation system following the protocol outlined for ethanol in step 4. Rinse the sample chamber with 70% ethanol and then with PBS, and reattach it to the sample chamber setup. Prepare mononuclear cells for elutriation 6. Isolate PBMC by density-gradient sedimentation on Ficoll-Hypaque. 7. Resuspend the PBMC in PBS and centrifuge 10 min in a GH-3.7 rotor at 800 rpm (200 × g), room temperature. This should leave most remaining platelets in suspension while pelleting the mononuclear cells. Decant the supernatant and resuspend mononuclear cells in 30 ml PBS. 8. Determine the approximate number of monocytes by selectively counting the cells on the Coulter counter channelyzer, which provides a profile of the cell size that allows for discrimination between lymphocytes (first peak) and monocytes (second peak). A maximum of 1.5 × 109 mononuclear cells are retained in the standard separation chamber for the JE-6B rotor. When mononuclear cells are obtained from leukapheresis, the number of monocytes may be 2-3 × 109. To purify this many monocytes, put a second standard separation chamber in the rotor in place of the by-pass chamber. Mount this chamber with the indicator pin on the top of the shelf in the rotor rather than in the hole designated for the pin. This is necessary because the lines on the bypass side of the JE-6B rotor are reversed. Also, be sure to use a flow rate in the elutriation described below that will elute most of the lymphocytes while retaining the monocytes. Load the mononuclear cells 9. Turn the knobs up on the three-way valves located on the inlet and outlet needle lines of the sample reservoir setup (Fig. 7.6.2A). Empty the sample reservoir with either a pipet or syringe attached to the injection port. Using a 10-ml pipet or syringe, load A T connector to rotor injection port pipet flow Luer lock connector from pump B to rotor flow from pump 3-way valves Luer lock connectors 70 ml sample reservoir Isolation of Monocyte/ Macrophage Populations Figure 7.6.2 Configuration of sample reservoir during loading of cells (A) and during elutriation (B). 7.6.5 Current Protocols in Immunology the cells into the sample reservoir through the three-way valve attached to the line with the long needle (Fig. 7.6.2). Confirm that there is no air in the injection line by filling the line with PBS. Before removing the pipet or syringe, turn the knob on the three-way value 90° to close the injection port. Also turn the knob on the opposite three-way valve 90° (the air in this line will be trapped in the sample chamber when the elutriation procedure starts). 10. Set the J-6M centrifuge to 1960 rpm (500 × g), 18°C, and the top three-way valve on the sample reservoir setup so that the flow will be directed through the short needle into the chamber (Fig. 7.6.2B). 11. Set the pump flow rate to 10 ml/min; this will result in the lymphocytes being eluted or forced out of the separation chamber(s) in the rotor while the monocytes are retained. Pump 300 ml PBS through the system in order to load all the cells in the sample reservoir as well as elute most of the lymphocytes from the separation chamber(s). Swirl the sample reservoir occasionally to prevent cells from accumulating on the bottom of the tube. Also, monitor the size of the cells exiting from the elutriator on the Coulter counter channelyzer to ensure that only lymphocytes are being eluted. Isolate the monocytes 12. Gradually increase the flow rate at increments of 0.5 ml/min, and pump 100 to 150 ml PBS through the system for each increment. Closely monitor the exiting cells on the Coulter counter. 13. When the ratio of monocytes to lymphocytes exiting the elutriator exceeds 50% (usually ∼11.5 to 12 ml/min), increase the flow rate to 19 ml/min and collect the exiting monocytes in six 50-ml tubes. 14. Turn off the centrifuge and wash out remaining cells or clumps of cells with PBS. 15. Centrifuge cells 10 min at 800 rpm (150 × g), room temperature, and resuspend the cells in DMEM. Determine the number of monocytes on the Coulter counter. The purity can be further assessed by flow cytometry or nonspecific esterase staining. After completing elutriation, pump distilled water and then air through the system. Occasionally, pump 50% chlorine bleach solution through the system to remove accumulated protein. Disassemble the rotor after each elutriation to minimize corrosion and rust. COMMENTARY Background Information Monocytes and tissue macrophages (collectively referred to as mononuclear phagocytes) play a critical role in host immune responses through their ability to act as phagocytes, to serve as accessory cells for mitogen-and antigen-specific lymphocyte responses, and to secrete soluble products (monokines). Thus, the isolation and study of this cell population is important to the understanding of host defense and the pathogenesis of inflammation. Monocytes are released from the bone marrow into the blood where they have a half-life of ∼8 to 9 hr. Isolation of these cells has the potential of allowing study of mononuclear phagocytic cells prior to their activation. The circulating monocytes migrate to inflammatory sites and tissues where they differentiate into long-lived resident macrophages. Isolation of these cells requires initial dispersal of the tissue under investigation, sometimes using collagenase and other agents. The cells isolated are more mature cells of the mononuclear phagocyte family that have frequently undergone activation in vivo. Following the initial separation of mononuclear cells (monocytes and lymphocytes) from the starting cell population (UNIT 7.1), monocytes are separated from lymphocytes. In the first three procedures described in this unit—adher- Immunologic Studies in Humans 7.6.6 Current Protocols in Immunology ence, size sedimentation, and flow cytometry— this is accomplished on the basis of the following properties of monocytes: their ability to adhere to glass or plastic, their unique size and density compared with other lymphoid cells, and their ability to express specific surface antigens. The advantage of separating monocytes by adherence is that the procedure is quick, easy, and does not require complicated equipment. However, adherence is an activation event that can induce both gene expression and protein secretion (Fuhlbrigge et al., 1987; Haskill et al., 1988). Separation by sedimentation with colloidal silica particles could potentially activate monocytes since silica has been shown to activate monocytes (Heppelston and Styles, 1967). Cell sorting by flow cytometry induces minimal cell activation using appropriate antibodies that do not induce signal transduction; however, this procedure results in relatively low cell yields. To circumvent the problems of activation and low yields, isolation of monocytes by counterflow centrifugal elutriation (CCE) is recommended. This procedure is particularly appropriate for isolating monocytes for gene expression studies. CCE separates cells on the basis of size and density. The cells are loaded in a separation chamber within a centrifuge rotor in a flow pattern which runs against, or counter to, the centrifugal force of the spinning rotor. Thus, the flow rate counters the force of gravity (g) causing the cells to stratify in the chamber in a zone where the sedimentation rate of the cell is balanced by the flow rate. Accordingly, the smaller (less heavy) cells are closer to the top of the chamber or the center of the centrifuge. These cells are the first to exit the separation chamber(s) and rotor as the flow rate is increased. By taking advantage of the differing sizes of the mononuclear subsets, the B cells, T cells, and monocytes, in that order, can be separated by CCE (Wahl et al., 1984). Critical Parameters and Troubleshooting Isolation of Monocyte/ Macrophage Populations Two problems occur using the first three methods for isolating monocytes. The isolated monocyte population may be contaminated by 2% to 10% non-monocytic cells. This contamination may be higher when isolating monocytes by sedimentation from patients with leukemia, because abnormal lymphoblasts may sediment with the monocytes. Also, the number of monocytes isolated is limited by the amount of sur- face available for adherence, the number of cells that can be layered onto the gradient, and the sorting capacity of the flow cytometer. Thus, only 60% to 90% of the starting monocytes may be recovered, depending on the procedure used. In the CCE procedure, air in the system can be a major problem. Air bubbles in the lines and the rotor must be eliminated before elutriation begins. While pumping ethanol or PBS through the system, air bubbles can be forced out of the rotor by manually spinning the rotor, and/or by intermittently pinching the inlet or outlet lines from the rotor. Another potential problem with CCE is cells exiting from the rotor before being separated. They will have the appearance of the unfractionated population. This is usually caused by mixing of the inlet and outlet flow at the surface of the rotating seal. Therefore, it is crucial that the rotating seal makes contact with the seal housing, as described in the procedure, and that the O-ring on the top of the shaft be inspected. This O-ring is very prone to damage and should be inspected each time the rotor is assembled. If there is leakage around the rotor, the chambers should also be inspected to be sure that they are assembled correctly and that the Orings are in place. Anticipated Results The purity of the monocyte population usually exceeds 90%, with 60% to 90% of the starting cells recovered in the first three protocols. In CCE, monocyte recovery depends on mononuclear cell density in the chamber. With up to 1.5 × 109 total mononuclear cells, yields of 75% to 95% are obtained. In contrast, with 5-9 × 109 mononuclear cells (containing 1-1.5 × 109 monocytes), recoveries are likely to be lower (50% to 80%), because the large number of lymphocytes that are exiting the rotor carry some of the monocytes with them. At all concentrations, however, purity of the isolated monocytes is 96%. Time Considerations The quickest method for isolating monocytes is adherence, which takes 1 hr. Isolation by colloidal silica particle gradient sedimentation takes ∼2 hr. Isolation by flow cytometry takes 3 to 5 hr, depending on the purity and size of the starting population and the desired purity and number of cells in the sorted population. Routine assembly of the elutriation system, once the initial tubing is in place, takes 15 to 20 min. Approximately 60 to 80 min are need- 7.6.7 Current Protocols in Immunology ed for preparation of the cells. The elutriation procedure requires ∼90 min. Thus, the entire procedure can be completed in ∼3 hr. Haskill, S., Johnson, C., Eierman, D., Becker, S. and Warren, K. 1988. Adherence induces selective mRNA expression of monocyte mediators and proto-oncogenes. J. Immunol. 140:1690-1694. Literature Cited Heppelston, A.G. and Styles, J.A. 1967. Activity of a macrophage factor in collagen formation by silica. Nature 214:521-522. Edelson, P.J. and Cohn, Z.A. 1976. Purification and cultivation of monocytes and macrophages. In In Vitro Methods in Cell-Mediated and Tumor Immunity (B.A. Bloom and J.R. David, eds.) pp. 333-340. Academic Press, San Diego. Fuhlbrigge, R.C., Chaplin, D.D., Kiely, J.M., and Unanue, E.R. 1987. Regulation of interleukin 1 gene expression by adherence and lipopolysaccharide. J. Immunol. 138:3799-3802. Gartner, S., Markovitz, P., Markovitz, D.M., Kaplan, M.H., Gallo, R.C. and Popovic, M. 1986. The role of mononuclear phagocytes in HTLVIII/LAV infection. Science 233:215-219. Gmelig-Meyling, F. and Waldmann, T.A. 1980. Separation of human blood monocytes and lymphocytes on a continuous percoll gradient. J. Immunol. Methods 33:1-9. Wahl, L.M., Katona, I.M., Wilder, R.L., Winter, C.C., Haraoui, B., Scher, I. and Wahl, S.M. 1984. Isolation of human mononuclear cell subsets by counterflow centrifugal elutriation (CCE). I. Characterization of B-lymphocyte-, T-lymphocyte-, and monocyte-enriched fractions. Cell. Immunol. 85: 373-383. Contributed by Larry M. Wahl and Phillip D. Smith National Institute of Dental Research/NIH Bethesda, Maryland Immunologic Studies in Humans 7.6.8 Current Protocols in Immunology Supplement 17