* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Gynecology. Infertility
Survey
Document related concepts
Transcript
INFERTILITY in Gynecology
Including Contraception and
Post Menopausal Anatomy
Harry H. Holdorf
Contents
Contraception
Infertility Defined
Causes of Infertility
Medication and Treatment
Assisted Reproduction Technology
Postmenopausal Anatomy
Hormone Replacement Therapy (HRT)
Contraception
There are countless ways available to prevent pregnancy.
Hormonal Methods
Hormonal methods are very reliable means of birth control.
Hormonal methods use two basic formulas:
– Combination hormonal methods:
contain both estrogen and progestin (synthetic progesterone).
Combination methods include pills ("the Pill"), skin patches, and rings.
– Progestin-only hormonal methods:
include pills, also called "mini-pills," and injections (Depo-Provera).
If a patient cannot take estrogen, a progestin-only method may be an option.
Contraception
Contraception
Intrauterine device (IUD)
An intrauterine device (IUD) is a small device that is placed in
the uterus to prevent pregnancy.
IUDs are wrapped with copper (Copper T 380-A) or contain a
hormone.
Once an IUD is in place, it can provide birth control for 5 to 10
years, depending on the type.
Unlike IUDs that were used in the 1970s, present-day IUDs
are small, safe, and highly effective.
Contraception
Contraception
Barrier methods
Barrier methods (including the diaphragm; cervical cap; Lea's Shield;
male condom; female condom; and spermicidal foam, sponge, gel,
suppository, or film) prevent sperm from entering the uterus and
reaching the egg.
Typically, barrier methods are not highly effective, but they generally
have fewer side effects than hormonal methods or IUDs.
Spermicides and condoms should be used together or along with
another method to increase their effectiveness.
Contraception
A cervical cap is made of rubber
and shaped like a large thimble. It
fits tightly over the cervix and is
used with a spermicide.
A diaphragm is a round, domeshaped device made of rubber with
a firm, flexible rim. It fits inside the
vagina and covers the cervix, the
opening of the uterus. It should
always be used with a sperm-killing
cream or jelly (spermicide).
Contraception
A male condom is a thin,
flexible tube of latex rubber,
polyurethane, or sheep
intestine that has a closed end.
The condom is placed over the
erect penis before intercourse.
A female condom is a tube of soft
plastic (polyurethane) with a closed
end. Each end has a ring or rim. The
ring at the closed end is inserted deep
into the vagina over the cervix, like a
diaphragm, to hold the tube in place.
The ring at the open end remains
outside the opening of the vagina.
Contraception
Lea's Shield is a new diaphragmtype device. Lea's Shield is made
of silicone, so latex allergy is not
a concern. The device comes in
one size only, simplifying the
fitting process.
A contraceptive sponge contains a
spermicide, nonoxynol-9, that is
released over the 24 hours that
the sponge may be left in the
vagina. The sponge also blocks the
cervix so sperm can't pass
Contraception
Permanent birth control (sterilization)
Sterilization
–
a surgical procedure done for men or women who decide that they do
not want to have any (or more) children.
– Sterilization is one of the most effective forms of birth control.
– Sterilization is intended to be permanent, and while you can try to reverse
it with another surgery, reversal is not always successful.
Tubal ligation or implants.
– Tubal ligation is a surgical procedure where the fallopian tubes, are tied,
cut, or blocked.
– A new nonsurgical sterilization technique uses a small metal coil, or tubal
implant , inserted up into each fallopian tube.
– Over time, scar tissue grows around each tubal implant, permanently
blocking the tubes.
Contraception
A tubal implant is a small metal spring that is placed in each of the two fallopian
tubes without using surgery. It is guided through the vagina, cervix, and uterus and
lodged in a fallopian tube. Over time, scar tissue grows around the two implants and
permanently blocks the tubes. This stops eggs from traveling from the ovaries and
down the fallopian tubes, where eggs are normally fertilized by sperm
Infertility
Causes of Infertility - Risk Factors
There are many risk factors as to why a woman may be infertile.
Some of these risk factors include:
– Age.
Age is the strongest predictor of female fertility.
After about age 32, a woman's fertility potential gradually declines.
A woman does not renew her oocytes. Infertility in older women may be due to a higher risk of
chromosomal abnormalities that occur in the eggs as they age.
Older women are also more likely to have health problems that may interfere with fertility.
The risk of miscarriage also increases with a woman's age.
–
Tobacco smoking.
Women who smoke tobacco may reduce their chances of becoming pregnant and the possible benefit of
fertility treatment.
Miscarriages are more frequent in women who smoke.
–
Body mass.
Extremes in body mass — either too high (body mass index, or BMI, of greater than 25.0) or too low (BMI
of lower than 20.0) — may affect ovulation and increase the risk of infertility.
–
Being overweight.
Among American women, infertility often is due to a sedentary lifestyle and being overweight.
–
Being underweight.
Women at risk include those with eating disorders, such as anorexia nervosa or bulimia, and women
following a very low-calorie or restrictive diet.
Strict vegetarians also may experience infertility problems due to a lack of important nutrients such as
vitamin B-12, zinc, iron and folic acid. Marathon runners, dancers and others who exercise very intensely
are more prone to menstrual irregularities and infertility.
Causes of Infertility
Causes of female infertility
The most common causes of female infertility include fallopian tube damage or blockage,
endometriosis, ovulation disorders, elevated prolactin, polycystic ovary syndrome, early menopause,
benign uterine fibroids and pelvic adhesions:
Fallopian tube damage or blockage.
– This condition usually results from inflammation of the fallopian tube (salpingitis).
Chlamydia is the most frequent cause.
Tubal inflammation may go unnoticed or cause pain and fever.
Tubal damage with scarring is the major risk factor of a pregnancy in which the fertilized egg
is unable to make its way through the fallopian tube to implant in the uterus (ectopic
pregnancy).
One episode of tubal infection may cause fertility difficulties.
The risk of ectopic pregnancy increases with each occurrence of tubal infection.
Endometriosis.
– Endometriosis occurs when the tissue that makes up the lining of the uterus grows outside of the
uterus.
– This tissue most commonly is implanted on the ovaries or the lining of the abdomen near the
uterus, fallopian tubes and ovaries.
– These implants respond to the hormonal cycle and grow, shed and bleed in sync with the lining
of the uterus each month, which can lead to scarring and inflammation.
– Pelvic pain and infertility are common in women with endometriosis.
Endometriosis
Sagittal view shows
endometrioma (e) in the cul-desac with diffuse low-level echoes.
The endometrioma lies directly
posterior to the uterus (u).
Endometriosis
Transverse view of a left
ovarian endometrioma
shows a heterogenous
appearance with diffuse
low-level echoes
interspersed with
echogenic and anechoic
areas.
Causes of Infertility
Infertility in endometriosis also may be due to:
Ovarian cysts
– Ovarian cysts may indicate advanced endometriosis and often are
associated with reduced fertility. Endometriomas can be treated with
surgery.
Scar tissue.
– Endometriosis may cause rigid webs of scar tissue between the uterus,
ovaries and fallopian tubes. This may prevent the transfer of the egg to
the fallopian tube.
Ovulation disorders.
– Some cases of female infertility are caused by ovulation disorders.
– Disruption in the part of the brain that regulates ovulation (hypothalamicpituitary axis) can cause deficiencies in luteinizing hormone (LH) and
follicle-stimulating hormone (FSH).
– Even slight irregularities in the hormone system can affect ovulation.
Specific causes of hypothalamic-pituitary disorders include:
– Direct injury to the hypothalamus or pituitary gland
– Pituitary tumors
– Excessive exercise
– Anorexia nervosa
Elevated prolactin– The hormone prolactin stimulates breast milk production. High levels in
women who aren't pregnant or nursing may affect ovulation.
Endometrial Scarring
Very bright
(hyperechoic)
uterine lining scar tissue in
cavity
Causes of Infertility
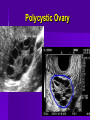
Polycystic ovary syndrome (PCOS).
– An increase in androgen hormone production causes PCOS.
– In women with increased body mass, elevated androgen production may
come from stimulation by higher levels of insulin.
– In lean women, the elevated levels of androgen may be stimulated by a
higher ratio of luteinizing hormone.
– Lack of menstruation or infrequent menses are common symptoms in
women with PCOS.
In PCOS, increased androgen production prevents the follicles of the ovaries from
producing a mature egg.
Small follicles that start to grow but can't mature to ovulation remain within the ovary.
A persistent lack of ovulation may lead to mild enlargement of the ovaries.
Without ovulation, the hormone progesterone isn't produced and estrogen levels remain
constant.
Elevated levels of androgen may cause increased dark or thick hair on the chin, upper lip or
lower abdomen as well as acne and oily skin.
Polycystic Ovary
Causes of Infertility
Early menopause (premature ovarian failure).
– Early menopause is the absence of menstruation and the
early depletion of ovarian follicles before age 35.
– Although the cause is often unknown, certain conditions are
associated with early menopause, including:
Autoimmune disease.
– The body produces antibodies to attack its own tissue, in this case
the ovary.
– This may be associated with hypothyroidism (too little thyroid
hormone).
– Radiation or chemotherapy for the treatment of cancer.
– Tobacco smoking.
Causes of Infertility
Benign uterine fibroids.
– Fibroids are benign tumors in the wall of the uterus and are common in
women in their 30s.
– Occasionally they may cause infertility by interfering with the contour of
the uterine cavity, blocking the fallopian tubes.
Pelvic adhesions.
– Pelvic adhesions are bands of scar tissue that bind organs after pelvic
infection, appendicitis, or abdominal or pelvic surgery.
– They may limit the functioning of the ovaries and fallopian tubes and
impair fertility.
– Scar tissue formation inside the uterine cavity after a surgical procedure
may result in a closed uterus and ceased menstruation.
– This is most common following surgery to control uterine bleeding after
giving birth.
Fibroids
Hysterosalpingogram showing a uterus with a submucosal myoma that is pushing in to the
cavity. Another myoma on the outside of the uterus is circumscribed by dye along the red line.
The myoma inside the cavity might cause reproductive problems.
Fibroids
Ultrasound view of a uterus with an intramural (within the uterine wall)
myoma. Image on right shows uterus outlined in blue, uterine lining in red,
myoma in green. A fibroid in this location should not affect chances for
pregnancy or miscarriage.
Scar Tissue/ Adhesions
Ultrasound of uterus with ovary
stuck on top in scar tissue
Uterus outlined in pink, uterine
lining yellow, ovary green
Causes of Infertility
A number of other causes can lead to infertility in women:
Medications.
– Temporary infertility may occur with the use of certain medications.
– n most cases, fertility is restored when the medication is stopped.
Thyroid problems.
– Disorders of the thyroid gland, either too much thyroid hormone
(hyperthyroidism) or too little (hypothyroidism), can interrupt the menstrual
cycle and cause infertility.
Cancer and its treatment.
– Certain cancers — particularly female reproductive cancers — often severely
impair female fertility.
– Both radiation and chemotherapy may affect a woman's ability to reproduce.
– Chemotherapy may impair reproductive function and fertility more severely in
men than in women.
Other medical conditions.
– Medical conditions associated with delayed puberty or amenorrhea, such as
Cushing's disease, sickle cell disease, HIV/AIDS, kidney disease and
diabetes, can affect a woman's fertility.
Ovarian Cancer
This is a ovary with multiple
irregular cysts and turned out
to a cystic cancer of the ovary
Transvaginal ultrasound examination
of an ovarian cyst showing
suspicious solid areas (arrows) and
abnormal blood flow (shown in red).
Medication and Treatment
of Infertility
Treatment of infertility depends on the cause, the
duration of the problem, the age of the partners and
their specific wishes.
– Some causes of infertility can't be corrected.
– However, various means of insemination or embryo
transfer may be possible so that a woman can still become
pregnant.
Non-surgical fertility treatment falls into two main
categories:
– Restoring or bringing about fertility
– Assisted reproductive technology (ART)
Medication and Treatment
of Infertility
Restoring or bringing about fertility
These approaches can involve steps related to the male or to the
female, or both.
Sperm survive in the female reproductive tract for up to 72 hours, and
an egg can be fertilized for up to 24 hours after ovulation. Increasing
the frequency of intercourse increases the chances for conception.
Fertility drugs (ovulation induction)
– Fertility drugs are the primary treatment for women who are infertile due to
ovulation disorders.
– These medications regulate or induce ovulation.
– In general, they exert actions designed to work like natural folliclestimulating hormone (FSH) and luteinizing hormone (LH).
Ovulation Induction
Ultrasound photo of a polycystic ovary
after Clomid treatment
Some mature size follicles are now
present, as well as some small ones
Ultrasound scan of stimulated
ovary.
Medication and Treatment
of Infertility
– Commonly used fertility drugs include:
Clomiphene citrate (Clomid, Serophene). This drug is
taken orally and stimulates ovulation in women who
have PCOS or other ovulatory disorders. It causes the
pituitary gland to release more FSH and LH, which
stimulate the growth of an ovarian follicle containing an
egg.
Human menopausal gonadotropin, or hMG (Repronex,
Pergonal). This injected prescription medication is for
women who don't menstruate on their own due to the
failure of the pituitary gland to stimulate ovulation.
Unlike clomiphene, which stimulates the pituitary
gland, hMG and other gonadotropins directly stimulate
the ovaries. This drug contains both FSH and LH.
Medication and Treatment
of Infertility
Follicle-stimulating hormone, or FSH (Gonal-F, Follistim, Bravelle).
FSH is essentially hMG without the LH. Like hMG, it works by
stimulating the ovaries to mature egg follicles.
Human chorionic gonadotropin, or hCG (Ovidrel, Pregnyl). Used in
combination with clomiphene, hMG and FSH, this drug stimulates the
follicle to release its egg (ovulate).
Gonadotropin-releasing hormone (Gn-RH) analogs. This treatment is
for women with irregular ovulatory cycles or who ovulate prematurely
— before the lead follicle is mature enough — during hMG treatment.
Gn-RH analogs deliver constant Gn-RH to the pituitary gland, which
alters hormone production, so that a physician can induce follicle
growth with FSH.
Metformin (Glucophage). This oral drug is taken to boost ovulation. It's
used when insulin resistance is known or suspected.
Medication and Treatment
of Infertility
Letrozole (Femara). This drug is in a class of medications
called aromatase inhibitors, which are approved for treatment
of advanced breast cancer. Doctors sometimes prescribe
letrozole for women who don't ovulate on their own and who
haven't responded to treatment with clomiphene citrate.
Letrozole is not approved by the U.S. Food and Drug
Administration for inducing ovulation. The drug's
manufacturer has warned doctors not to use the drug for
fertility purposes because of possible adverse health effects.
These adverse effects may include birth defects and
miscarriage.
Bromocriptine. This medication is for women whose ovulation
cycles are irregular due to elevated levels of prolactin, the
hormone that stimulates milk production in new mothers.
Bromocriptine inhibits prolactin production.
Medication and Treatment
of Infertility
Injectable fertility drugs significantly increase the chance of multiple births. The use of
these drugs requires careful monitoring with a combination of blood tests of hormones
and ultrasound measurement of ovarian follicle size. Generally, the greater the number of
fetuses, the higher the risk of premature labor. Babies born prematurely are at increased
risk of health and developmental problems. The risk is greater for triplets than it is for
twins or single pregnancies.
The risk of multiple pregnancies can be reduced. If a woman requires an hCG injection to
trigger ovulation, and ultrasound exams show that too many follicles have developed, she
and her doctor can decide to withhold the hCG injection. For many couples, however, the
desire to become pregnant overrides concerns about conceiving multiple babies.
When too many babies are conceived, removal of one or more fetuses (multifetal
pregnancy reduction) can offer improved survival odds for the surviving fetuses. This
presents serious emotional and ethical challenges for many people. If you and your
partner are considering fertility drug treatment, discuss this possibility with your doctor
before starting treatment.
There may be a link between fertility drugs and an increased, long-term risk of ovarian
cancer. However, the association between fertility drugs and ovarian cancer hasn't been
confirmed.
Assisted
Reproductive
Technology
Assisted Reproductive
Technology
ART has revolutionized the treatment of
infertility. Each year thousands of babies are
born in the United States as a result of ART.
Medical advances have enabled many
couples to have their own biological child.
An ART health team includes physicians,
psychologists, embryologists, laboratory
technicians, nurses and allied health
professionals who work together to help
infertile couples achieve pregnancy
Assisted Reproductive Technology
The most common forms of ART include:
In vitro fertilization (IVF).
Electroejaculation.
– Electric stimulus brings about ejaculation to obtain semen.
– This procedure can be used in men with a spinal cord injury who can't
otherwise achieve ejaculation.
Surgical sperm aspiration.
– This technique involves removing sperm from part of the male
reproductive tract such as the epididymis, vas deferens or testicle.
– This allows retrieval of sperm if blockage is present.
Intracytoplasmic sperm injection (ICSI).
–
–
Assisted hatching.
–
This technique consists of a microscopic technique in which a single sperm is
injected directly into an egg to achieve fertilization in conjunction with the standard
IVF procedure.
ICSI has been especially helpful in couples who have previously failed to achieve
conception with standard techniques.
This technique attempts to assist the implantation of the embryo into the lining of the
uterus.
ART works best when the woman has a healthy uterus, responds well to
fertility drugs, and ovulates naturally or uses donor eggs. The man should
have healthy sperm, or donor sperm should be available. The success rate of
ART gradually diminishes after age 32.
Gamete Intra-fallopian
Transfer
GIFT was developed primarily for couples with "unexplained infertility" to facilitate a
formal "meeting" of the sperm and egg.
Fertility drugs are used to stimulate the ovaries to produce multiple follicles.
The follicles are retrieved.
There is no fertilization process that is done in a laboratory.
Instead, roughly two hours prior to egg retrieval, a semen sample is delivered and put
inside a centrifuge where it's washed and then placed in a test tube.
The active sperm swim to the top of the test tube and are then placed inside a catheter.
The mature egg is placed inside a separate catheter. Each catheter is then inserted into
the fallopian tube via a laparoscopy procedure under a general anesthetic.
A woman undergoing GIFT will need to rest quietly after the procedure and report for a
pregnancy test roughly two weeks later.
If pregnancy doesn't occur, a maximum of four GIFT cycles is recommended.
Gamete Intrafallopian
Transfer
After the eggs have been collected and examined, they are mixed with the
prepared sperm and transferred to the fallopian tube.
In Vitro Fertilization
Ovaries are hyper-stimulated through medication to produce ova.
Ultrasound is used to monitor the development of the eggs inside the
ovary.
Once eggs have matured they are collected from the ovary.
A sampling of sperm is then collected.
IVF involves combining eggs and sperm outside the body in a
laboratory.
About 2 to 5 days after fertilization, the best fertilized eggs are
selected.
Two to four are placed in the uterus using a thin flexible tube
(catheter) that is inserted through the cervix. .
IVF
Zygote Intra Fallopian
Transfer
Zygote intrafallopian transfer (ZIFT) is
technique in which a woman's egg is
fertilized outside the body, then implanted in
one of her fallopian tubes.
This procedure involves the placement of
the zygote directly into the fallopian tube
utilizing a laparoscope.
Zygote Intra Fallopian
Transfer
ZIFT involves ovarian stimulation, monitoring and
egg retrieval, to ensure the greatest possibility of
success, several ova are collected and fertilized at
a time.
The ovaries are stimulated with hormones to
release several mature eggs at once.
Once mature, the eggs are collected using
ultrasound or laparoscopy.
Zygote Intra Fallopian Transfer
The ultrasound retrieval method is performed in the doctor's office or ultrasound laboratory.
–
–
–
The doctor places a needle inside a guide which is attached to an vaginal probe.
After the patient receives a local anaesthetic, the doctor uses the Transvaginal probe to locate the
follicles containing the eggs.
Then the doctor guides the needle through the vaginal wall and aspirates the fluid containing the
eggs into a small tube.
The sperm are collected, specially prepared, and combined with the eggs in a special
medium that contains the nutrients similar to those found in the uterus.
After a day, during which fertilization takes place, the fertilized eggs are evaluated,
transferred to another dish containing a suitable solution, and allowed to grow.
With ZIFT, the embryos are just grown in the lab for a day and are transferred back the day
after retrieval.
ZIFT requires that the woman have at least one functioning fallopian tube. Therefore, ZIFT
is not an option in women with infertility caused by tubal problems.
Postmenopausal Anatomy
and Physiology
Normal Anatomy
– The normal adult uterus measures approximately 7.0 - 9.0 cm long, 4.5 - 6.0 cm wide and 2.5 3.5 cm deep (anteroposterior dimension).
Menopausal Anatomy– During the POST-MENOPAUSAL years of a normal female, the uterus decreases in size and
the endometrium atrophies.
Menopause:
– is defined as the time that ovulation and menstruation cease.
–
usually occurs between the ages 45-55.
–
accompanied by a decline in circulating concentrations of estrogen & progesterone and a sharp
sustained rise in the production of Gonadotropin-releasing hormone (GnRH), Follicle
Stimulating Hormone (FSH) and Lutenizing Hormone (LH).
–
The decline in estrogen levels leads to reductions in the size of the uterus & breasts,
accompanied by a thinning of the urethral & vaginal epithelia.
–
Hot flashes typically begin while estrogen levels are declining & cease when estrogen levels
reach minimal values.
–
These intervals of elevated body temperature are associated with surges in LH production.
–
Atherosclerosis & other forms of cardiovascular disease increases after menopause.
Hormonal Replacement
Therapies
Some individuals experience acutely unpleasant symptoms before,
during or after menopause.
For most of those individuals relief may be found through hormonal
replacement therapies involving a combination of estrogen and
progestins.
This type of treatment may prevent osteoporosis, as well as the
neural and vascular changes associated with menopause.
The hormones are administered as pills, by injections, or by
transdermal “ estrogen patches.”
Recent studies suggest that estrogen-replacement therapy should be
prescribed with caution & only after full assessment & discussion of
the potential risk & benefits.
Hormonal Replacement
Therapy
Women can experience side effects
during hormone therapy;
Some of the minor side effects are
more common than, and are generally
described by women as “annoying.”
– These side effects include:
Headaches
Nausea
Breast pain