* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Gonapure ® Insert
Survey
Document related concepts
Transcript
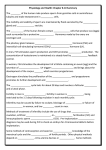
Gonapure® Insert COMPOSITION: Active ingredient: r-hFSH 75 I.U. or 150 I.U. Inactive ingredients: Sucrose, Disodium phosphate dihydrate, Monosodium phosphate monohydrate, O-phosphoric acid, Sodium hydroxide, Nitrogen to fill container. DESCRIPTION Gonapure® is a human follicle stimulating hormone (FSH) preparation of recombinant DNA origin. Gonapure ® contains no luteinizing hormone (LH) activity. Therapeutic Class: Infertility. CLINICAL PHARMACOLOGY FSH stimulates ovarian follicular growth in women who do not have primary ovarian failure. FSH, the active component of Gonapure® is the primary hormone responsible for follicular recruitment and development. In order to affect final maturation of the follicle and ovulation in the absence of an endogenous LH surge, human chorionic gonadotropin (hCG) must be given following the administration of FSH, when monitoring of the patient indicates that sufficient follicular development has occurred. There is interpatient variability in response to FSH administration. FSH, when administered with hCG, stimulates spermatogenesis in men with hypogonadotropic hypogonadism. FSH is the primary hormone responsible for spermatogenesis. PHARMACOKINETICS FSH is slowly absorbed after subcutaneous or intramuscular injection, with an absolute bioavailability of about 70 to 80%. Accumulation occurs with repeated doses, reaching a steady state within 3 to 5 days. Follitropins are slowly eliminated from the body, with a terminal half-life ranging from 12 to 70 hours. About one-eighth of a dose of follitropin alfa is reported to be excreted in the urine. SPECIAL POPULATIONS Safety, efficacy, and pharmacokinetics of FSH in patients with renal or hepatic insufficiency have not been established. DRUG-DRUG INTERACTION No drug-drug interaction studies have been conducted. INDICATIONS AND USAGE Follicle-stimulating hormone is secreted by the anterior lobe of the pituitary gland, with another gonadotropin; luteinising hormone. These gonadotropins stimulate the normal functioning of the gonads and the secretion of sex hormones in both men and women. In women, follicle-stimulating hormone stimulates the development and maturation of the follicles and ova; in men it has a role in spermatogenesis. Recombinant human follicle-stimulating hormones are used in the treatment of female infertility due to anovulation, in women who have not responded to clomiphene therapy. FSH is also used for the stimulation of spermatogenesis in the management of male infertility caused by hypogonadotrophic hypogonadism DOSAGE AND ADMINISTRATION The dosage and schedule of treatment for female infertility must be determined according to the needs of each patient; it is usual to monitor response by studying the patient's urinary oestrogen excretion or by ultrasonic visualization of follicles or both. In menstruating patients treatment should be started within the first 7 days of the menstrual cycle. Treatment is usually begun with 75 to 150 units daily by subcutaneous or intramuscular injection for 7 or 14 days; if there is no response, dosage is increased at 7- or 14-day intervals until an adequate but not excessive response is achieved. Treatment is then stopped and followed after 1 or 2 days by a single dose of chorionic gonadotrophin 5000 to 10000 units to induce ovulation. A daily dose of 225 units is the usual maximum, and that if a patient fails to respond adequately after 4 weeks of treatment that cycle should be abandoned and the patient should subsequently begin the next cycle at a higher starting dose. FSH are also used as part of IVF or other assisted reproductive technologies. For this purpose doses of 150 to 225 units daily are generally given, for at least 4 days, commencing on the second or third day of the menstrual cycle. Thereafter the dose may be adjusted individually based on ovarian response to a usual maximum of about 450 units; adequate follicular development generally occurs within about 5 to 10 days of treatment. Pituitary downregulation with a gonadorelin analogue may be used with FSH therapy, in which case the gonadorelin analogue is generally begun about 2 weeks before FSH, and the 2 are then continued together until follicular development is adequate. A single dose of up to 10 000 units of chorionic gonadotrophin is then given to induce final follicular maturation and oocyte retrieval performed about 35 hours later. FSH is used for the stimulation of spermatogenesis in the management of male infertility caused by hypogonadotrophic hypogonadism. Before starting FSH therapy, chorionic gonadotrophin is given to raise serum testosterone concentrations to the normal range, which may take 3 to 6 months. A dose of 150 units subcutaneously three times weekly is then used, with continued chorionic gonadotrophin; doses of follitropin alfa up to 300 units three times weekly may be required. Treatment is continued for at least 4 months, and more than 18 months of treatment may be needed. CONTRAINDICATIONS FSH is contraindicated in women and men who exhibit: 1. Prior hypersensitivity to recombinant FSH preparations or one of their excipients. 2. High levels of FSH indicating primary gonadal failure. 3. Uncontrolled thyroid or adrenal dysfunction. 4. Sex hormone dependent tumors of the reproductive tract and accessory organs. 5. An organic intracranial lesion such as a pituitary tumor. And in women who exhibit: 6. Abnormal uterine bleeding of undetermined origin. 7. Ovarian cyst or enlargement of undetermined origin. 8. Pregnancy. PRECAUTIONS General: Careful attention should be given to the diagnosis of infertility in candidates for FSH therapy. Information for Patients: Prior to therapy with FSH therapy, patients should be informed of the duration of treatment and monitoring of their condition that will be required. The risks of ovarian hyperstimulation syndrome and multiple births in women and other possible adverse reactions should also be discussed. Laboratory Tests: In most instances, treatment of women with FSH results only in follicular recruitment and development. In the absence of an endogenous LH surge, hCG is given when monitoring of the patient indicates that sufficient follicular development has occurred. This may be estimated by ultrasound alone or in combination with measurement of serum estradiol levels. The combination of both ultrasound and serum estradiol measurement are useful for monitoring the development of follicles, for timing of the ovulatory trigger, as well as for detecting ovarian enlargement and minimizing the risk of the Ovarian Hyperstimulation Syndrome and multiple gestation. It is recommended that the number of growing follicles be confirmed using ultrasonography because plasma estrogens do not give an indication of the size or number of follicles. The clinical confirmation of ovulation, with the exception of pregnancy, is obtained by direct and indirect indices of progesterone production. The indices most generally used are as follows: 1. A rise in basal body temperature; 2. Increase in serum progesterone; and 3. Menstruation following a shift in basal body temperature. When used in conjunction with the indices of progesterone production, sonographic visualization of the ovaries will assist in determining if ovulation has occurred. Sonographic evidence of ovulation may include the following: 1. Fluid in the cul-de-sac; 2. Ovarian stigmata; 3. Collapsed follicle; and 4. Secretory endometrium. Accurate interpretation of the indices of follicle development and maturation require a physician who is experienced in the interpretation of these tests. Pregnancy: Pregnancy Category X. Nursing Mothers: It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in the nursing infant from FSH, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Pediatric Use: Safety and effectiveness in pediatric patients have not been established. PACK AND STORAGE: Gonapure® (r-hFSH) single dose vials: Gonapure® (r-hFSH) is supplied in a sterile, lyophilized form in single dose vials containing 75 or 150 IU FSH activity with diluent (Sterile Water for Injection). Lyophilized vials may be stored refrigerated at temperature 2-8°C. Protect from light.