* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download (Hsp90) inhibitors
Cytokinesis wikipedia , lookup
Tissue engineering wikipedia , lookup
Cell culture wikipedia , lookup
Extracellular matrix wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Cell encapsulation wikipedia , lookup
Cellular differentiation wikipedia , lookup
Signal transduction wikipedia , lookup
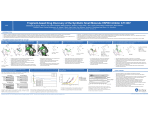
COMMUNICATION Redefining the phenotype of Heat shock protein 90 (Hsp90) inhibitors Yao Wang,b Yen Chin Koaya, and Shelli R. McAlpine*a The phenotypes produced when cells are treated with the Hsp90 inhibitors AUY922 or 17-AAG (classical inhibitors) are different to those produced when cells are knocked down with Hsp90. Pulldown assays using classical inhibitors suggest that these molecules bind to multiple targets other than Hsp90. Classical inhibitors also induce similar protein markers as other anti-cancer therapies Cisplatin and bortezomib that do not target Hsp90. Together these data suggest that AUY922 and 17-AAG acts on multiple targets and likely kills cells through multiple mechanisms. Comparing these classical inhibitors to the effects seen when treating cells with Cterminal Hsp90 modulators reveals that C-terminal modulators effectively bind to Hsp90, and induce phenotypic markers consistent with the Hsp90 CRISPR knockdown data. Our findings challenge the current interpretation of Hsp90 inhibitors and suggest that a large body of literature that describes the Hsp90 phenotype and inhibitors is re-examined in this context. Heat shock protein 90 (Hsp90) is a well-investigated chemotherapeutic target, with 15 unique clinical structures reported to act by controlling this protein [1]. Hsp90 plays a major role in controlling proteins that regulate many oncogenic pathways[2], and it was anticipated that Hsp90 inhibitors would be highly successful at blocking drug resistance and metastasis [3]. However, these clinically tested drugs have produced disappointing results. Mechanistically, all 15 clinical trial drugs (termed “classical Hsp90 inhibitors”) are similar: they are all reported to bind inside the ATPbinding pocket on Hsp90’s N-terminus, blocking ATP-Hsp90 interactions, thereby suppressing Hsp90’s functions. All classical inhibitors produce a similar cellular phenotype that includes the up-regulation of heat shock factor 1 (HSF-1), heat shock protein 70 (Hsp70) and heat shock protein 27 (Hsp27). Indeed, the most common approach for identifying Hsp90 inhibitors is to screen for molecules that induce an increase in Hsp70 protein, with the assumption that they will be Hsp90 inhibitors. It is also well established that these three heat shock proteins initiate anti-apoptotic cascades and promote drug resistance,[4] which is a highly problematic property in a cancer drug. Another explanation for these classical inhibitors’ clinical failure is that act via multiple mechanisms in a cellular environment. Binding to multiple proteins perhaps in addition to Hsp90 and producing off-target effects would explain the perplexing data reported for these classical inhibitors. Specifically, several N-terminal inhibitors, including Geldanamycin (GM) and 17-(Allylamino)-17- [a] [b] Y.C.Koay, Assoc. Prof. S.R.McAlpine School of Chemistry, University of New South Wales, Sydney, NSW 2052, Australia. E-mail: [email protected] Dr. Y..Wang Department of Medicine University of New South Wales E-mail: [email protected] demethoxygeldanamycin (17-AAG), have a binding affinity for isolated or purified Hsp90 protein in the low micromolar range[5], which is at odds with these inhibitors’ nanomolar GI50 values for inhibiting cancer cell growth. Surprisingly, studies using siRNA or CRISPR technology to knockdown or knockout Hsp90 have not been reported and compared to the impact of treating cells with these extensively utilized molecules. Although pull-down assays using tagged molecules of classical Hsp90 inhibitors have been published, close analysis of these data suggest that the molecules do not target Hsp90 alone but rather have non-specific binding affinities for multiple proteins[5c, 6]. In the past 10 years over 10,000 papers have been published reporting studies on Hsp90 (Scopus), of which over 5,000 use classical inhibitors to investigate Hsp90 pathways. Thus, it is important to understand how these classical inhibitors behave in a cellular environment. Herein we show that the phenotype of Hsp90 knockdown cells using CRISPR technology is significantly different to that generated when cells are treated with classical inhibitors. We reveal that drugs acting via mechanisms unrelated to Hsp90 induce a similar phenotype to that produced by classical Hsp90 inhibitors. We also show that in contrast to an earlier report, [5c] classical molecules are not highly effective at binding to Hsp90 in cancer cells despite their toxicity. We compare the growth inhibitory effect of these classical versus C-terminal inhibitors (SM inhibitors) to their binding affinity for Hsp90. Despite the C-terminal modulators lower cellular potency than the classical inhibitors, we show that the C-terminal modulators outperform classical inhibitors when pulling down Hsp90 from cancer cell lysates. The SM inhibitors also produce a phenotype that is identical to that of Hsp90 knockdown cells, whereas the classical inhibitors produce a very different phenotype. Taken together our data indicate that SM molecules likely function primarily via inhibition of Hsp90. In contrast, classical inhibitors likely act via multiple mechanisms (perhaps including Hsp90), and produce a stress response that is unrelated to Hsp90 inhibiton within the cell. Early work has shown that the behavior of classical[7] and C-terminal inhibitors[8] is cell line independent. It has been well documented that both classical inhibitors and Cterminal inhibitors behave similarly in all cancer cells and this is logical given that Hsp90 is an important chaperone in all cancer cells. Our Hsp90 knockdown studies were conducted in HeLa cells using the CRISPR/Cas9 knockout system, however, the data is translatable to other cell lines. When the protein level of Hsp90α, which is the inducible form of Hsp90 and encoded by HSP90AA1, was decreased by ~ 45% of the control level in HeLa cells, there was no observable increase in the protein expression of HSF-1, Hsp70 and Hsp27 (Fig 1a). Thus a decrease of Hsp90 protein levels does not produce cellular stress, at least as measured by increases in Hsp70 or Hsp27. In contrast, cells treated with AUY922 COMMUNICATION IS PR R C Sc ra m C on t ro l a) HeLa bl ed (which according to the literature targets Hsp90) showed a strong up-regulation of these heat shock proteins (HSPs) (Fig 1a). The protein expression level of Hsp90α isoform was significantly increased by AUY922 treatment (Fig 1a ~ 3 fold). These data indicate that the increase in HSPs is likely unrelated to Hsp90 inhibition in cells. These data also suggest that the cellular stress caused by AUY922 even at low levels of AUY922 treatment, is induced via a mechanism that does not involve Hsp90. Comparing cells treated with Cterminal modulators SM258 (or supplemental data SM253) to the knockdown showed that both modulators produced a similar impact on HSP production to that seen in Hsp90α knockdown cells (Fig. 1b). Thus, in contrast to the classical inhibitors, SM compounds produce a similar phenotype to that produced when knocking down Hsp90 α. AUY922 Hsp90 inhibition, we investigated the impact of Bortezomib (PS-341 or PS) and Cisplatin (Cis), two well-established chemotherapeutic drugs, on the protein expression of HSF-1 and Hsp70 in HCT116 human colorectal carcinoma cells. PS acts as a proteasome inhibitor that blocks protein degradation. Cis crosslinks DNA and leads to DNA damage in cells. At concentrations that were 5 and 10 fold over the GI 50 of each drug, PS, Cis and AUY922 all increased the protein levels of HSF-1 and Hsp70 in HCT116 cells after 24 h-treatments (Fig. 2). Treatments with PS resulted in much higher levels of Hsp70 protein than caused by AUY922 treatments. Specifically, the Hsp70 expression level in PS-treated HCT116 cells was ~ 9 fold the control level, whereas Hsp70 increased by ~ 5 fold over the control in AUY922-treated cells (Fig. 2). HCT116 AUY-922 (nM) a) DMSO 25 nM 50 nM 100 nM Hsp90a HSF-1 HCT116 AUY-922 (nM) Hsp70 Hsp27 Actin R IS PR C am 50 HCT116 PS-341 (nM) 100 HSF-1 HSF-1 Hsp70 Hsp70 Actin Actin 0 30 60 HCT116 Cisplatin (µM) HSF-1 HSF-1 HSF-1 Hsp70 Hsp70 Hsp70 Actin Actin Actin IV V VI VII b) AUY922 SM253 SM258 50 nM 100 nM 30 mM 25 mM Hsp90a Hsp70 Hsp27 Actin 12 0 30 0 30 60 HSP Expression in HCT116 Cells (24 h-treatments) HSF-1 Hsp70 10 8 6 4 2 0 I II III IV V VI VII Figure 1. Hsp90α knockdown study in HeLa cells. a) The impact of Hsp90α knockdown and AUY922 treatments on the protein expression of Hsp90α, HSF-1, Hsp70 and Hsp27. b) Comparison of the impact of Hsp90α knockdown, AUY922 (50 nM and 100 nM), SM253 (30 µM) and SM258 (25 µM) on the production of Hsp90α, total Hsp90, HSF-1, Hsp70 and Hsp27. Actin was used as the protein loading control. All experiments were performed at least three times, and representative images are shown. The knockdown data provides evidence that the upregulation of HSPs caused by AUY922 treatment is unlikely to be the result of suppressing Hsp90’s function. However, it may be the outcome of a cellular stress response caused by off-target toxicity. In order to assess whether similar stress responses can be triggered by mechanisms unrelated to A U A Y9 D U 2 M Y9 2 S 22 (50 O ( 1 nM 0 PS 0 ) ( nM P S 30 ) n C ( 60 M ) is n ( C 30 M) is µ (6 M 0 ) µM A ) U Y A 9 D U 2 M Y9 2 S 22 (50 O ( 1 nM 0 PS 0 ) ( nM P S 30 ) n C ( 60 M ) is n ( C 30 M) is µ (6 M 0 ) µM ) Lane: HCT116 PS-341 (nM) 100 Fold Change Relative to Control Treatment III bl ed II Sc r HeLa or m al b) I N Lane: 0 50 0 Figure 2. The protein expression of HSF-1 and Hsp70 in HCT116 cells treated with PS and Cis at indicated concentrations for 24 hrs. a) The representative Immunoblot images are shown. Actin was used as the protein loading control. b) Immunoblot results are plotted as fold change relative to the untreated control, which is set as 1. All values are average ± s.e.m. from three independent experiments. Although not as effective as PS or AUY922, Cis also induced up-regulation of Hsp70 by 2 fold over of the control (Fig. 2). These data indicate that toxic molecules can produce high levels of HSPs regardless of mechanism, and show that inducing high levels of Hsp70 and HSF-1 are a phenotype of general toxicity. Taken together the knockdown data and the induction of Hsp70 and HSF-1 when treated with three 60 COMMUNICATION different types of drugs are evidence that classical inhibitors produce stress effects that are unrelated to Hsp90. Verification of a molecule’s affinity for a protein in cell lysate is typically accomplished using pull-down assays. Pulldowns have been performed using biotin-tagged Geldanamycin (GM-tag)[5c], where competitive binding assays were used to demonstrate that 17-AAG bound effectively to Hsp90. Through competitive binding assays using GM-Tag, we tested two classes of inhibitors: classical inhibitors 17-AAG, and AUY922 (structures in Supplementary Fig. 1a and b), and Cterminal modulators SM253 and SM258 (structures in Supplementary Fig. 1c and d). Pulling down Hsp90 from cell lysates required tagged versions of these inhibitors, thus PEG-Biotin-tagged SM253 and SM258 (SM253-Tag and SM258-Tag, Supplementary Fig. 1e and f) were synthesized, and PEG-Biotin-tagged GM (GM-Tag, Supplementary Fig. 1g) was purchased. 17-AAG binds to Hsp90 with an IC50 of 700 nM despite killing cells at concentrations mid to low nM (GI50 =10-50 nM). Thus, it is likely acting via multiple mechanisms given its low affinity for Hsp90. Similarly, AUY922, which kills cells at low nM (GI50 ~10 nM), only has an affinity for Hsp90 of 230 nM. (Fig. 3a). These two data are inconsistent for a compound that acts primarily via Hsp90. AUY922 should be more effective at binding to Hsp90 than killing cells because there is no cellular membrane involved in the pulldown studies. Calculating the amount of Hsp90 present in the cell lysate confirms the hypothesis that AUY922 and 17-AAG are likely not acting via as Hsp90 their primary mechanism. Hsp90 is ~ 3% of all protein in HCT116 cancer cells. Using 50 µg of HCT116 cell lysate and GM-Tag, there is ~110 nM of Hsp90, which is 55 nM of the active Hsp90 dimer. Yet 700 nM of 17-AAG or 230 nM AUY922 are required in order to bind effectively to the Hsp90 dimer, while the concentrations of 17-AAG and AUY922 required to inhibit 50% of HCT116 cell growth is 50 nM and 10 nM respectively. These data show that it is unlikely classical inhibitors kill cells via an Hsp90 mechanism because the concentration required to bind to Hsp90 is up to 23 fold greater than the amount required to kill cells. The significantly higher concentrations required to bind to Hsp90 in the presence of cell lysate versus the much lower doses for suppressing cell growth indicate that these classical inhibitors must be killing cells via alternative mechanisms. In contrast, the SM molecules are relatively effective at binding to Hsp90 with comparable binding affinities to their GI 50 values for killing cells. Specifically, they have IC50 binding affinities for Hsp90 of ~20 µM,[9] which is similar to the GI50 (~5 µM).[8] Thus the SM compounds likely reach the necessary concentration to bind effectively to Hsp90, and kill cells via this mechanism. Comparison of tagged SM compounds to GM-Tag showed that GM-Tag pulled down similar levels of Hsp90 as the negative controls. In contrast, SM253-Tag and SM258-Tag pulled down Hsp90 by ~ 6 and 14 fold more than the GM-Tag, respectively (Fig. 3b). b) Figure 3. Binding affinity of Hsp90 inhibitors for Hsp90 in HCT116 cells. a) Competitive pull-down assays using GM-Tag as the probe were performed to evaluate the binding affinity of 17-AAG and AUY922 for Hsp90 in HCT116 cell lysate. Treatment with DMSO in the absence of GM-Tag was used as the negative control. b) A protein pull-down assay comparing the binding affinity of SM253-Tag (i.e. SM253-T), SM258-Tag (i.e. SM253-T) and GM-Tag (i.e. GMT) for Hsp90 in HCT116 cell lysate. DMSO and PEG-Biotin tag (i.e. Tag) were tested as negative controls. All experiments were performed in triplicate, and representative immunoblot images are shown (the images of full length Coomasie stained gels are in the Supplementary Fig. 3). In summary, classic inhibitors, GM, 17-AAG, and AUY922, all exhibit poor binding affinity for Hsp90 in cell lysate, and they induce a stress response in cells, which includes the overproduction of multiple HSPs at protein expression levels. This cellular phenotype is different from that seen in the Hsp90 slightly decreased. The large increase in Hsp70 produced when cells are treated with classical inhibitors is consistent with other drugs that induce cellular stress. Our combined CRISPR phenotype and pulldown data show that classical Hsp90 inhibitors likely suppress cell growth via multiple mechanisms, which may or may not include the inhibition of Hsp90. Treatment with SM compounds against cancer cells suppresses HSP production, which is similar to the phenotype observed in Hsp90 knockdown cells. C-terminal modulators of Hsp90, SM253 and SM258, selectively pull down Hsp90 in cell lysate, indicating their capability for targeting Hsp90 in the cell system. Indeed, their binding affinity for Hsp90 in a cellular environment correlates to drug concentrations needed to kill cells. These data indicate that the SM molecules likely act on Hsp90 as the primary target. Taken together, these data reinforce the fact that phenotypes identified using small molecules should be compared to knockdown phenotypes of their proposed targets before a target is validated for these small molecules. Acknowledgements This work was supported by the US National Institute of Health grant NCI R01CA137873 and the Australian National Health and Medical Research Council (NHMRC) grant GNT1043561. We thank UNSW for support of Y.W. and S.R.M., and the NHMRC COMMUNICATION for support of Y.W. We also thank the Endeavour program for supporting Y.C.K. [6] Keywords: Heat shock protein 90 • phenotype • CRISPR • knockdown • AUY922 [1] [2] [3] [4] [5] See <http://www.clinicaltrials.gov> D. Hanahan, R. A. Weinberg, Cell 2011, 144, 646-674. a) U. Banerji, Proc. Am. Assoc. Cancer Res. 2003, 44, 677; b) E. A. Sausville, Curr. Cancer Drug Targets 2003, 3, 377-383; c) L. H. Pearl, C. Prodromou, Curr. Opin. Struct. Bio. 2000, 10, 46-51; d) A. Dehner, J. Furrer, K. Richter, I. Schuster, J. Buchner, H. Kessler, ChemBioChem 2003, 4, 870-877; e) F. X. Hagn, K. Richter, J. Buchner, H. Kessler, Proc. experimental nuclear magnetic resonance conference 2005; f) J. M. Jez, J. C. Chen, G. Rastelli, R. M. Stroud, D. V. Santi, Chem. Biol. 2003, 10, 361-368. J. R. Mcconnell, S. R. Mcalpine, Bioorg. Med. Chem. Lett. 2013, 23, 1923-1928. a) B. Panaretou, C. Prodromou, S. M. Roe, R. O'brien, J. E. Ladbury, P. W. Piper, L. H. Pearl, EMBO J 1998, 17, 4829-4836; b) S. M. Roe, C. Prodromou, O. B. R., J. E. Ladbury, P. W. Piper, L. H. Pearl, J. Med. [7] [8] [9] Chem. 1999, 42, 260-266; c) A. Kamal, L. Thao, J. Sensintaffar, L. Zhang, M. F. Boehm, L. C. Fritz, F. J. Burrows, Nature. 2003, 425, 407. a) G. Chiosis, H. Jhuezo, N. Rosen, E. Mimgaugh, L. Whitesell, L. Neckers, Mol. Cancer Ther. 2003, 2, 123-129; b) K. Moulick, J. Ahn, H. Zong, A. Rodina, L. Cerchietti, D. E. Gomes, E. Caldas-Lopes, K. Beebe, F. Perna, K. Hatzi, L. Vu, X. Zhao, D. Zatorska, T. Taldone, P. Smith-Jones, M. Alpaugh, S. S. Gross, N. Pillarsetty, T. Ku, J. S. Lewis, S. M. Larson, R. Levine, H. Erdjument-Bromage, M. L. Guzman, S. D. Nimer, A. Melnick, L. Neckers, G. Chiosis, Nat. Chem. Biol. 2011, 25, 818-826. a) U. Banerji, M. Walton, F. Raynaud, R. Grimshaw, L. Kelland, M. Valenti, I. Judson, P. Workman, Clin. Cancer Res. 2005, 11, 70237032; b) L. E. Xu, J. L.; Egorin, M. J.; D’argenio, D. Z. , J. Pharmacokinet Pharmacodyn. 2003, 30, 185-219. Y. C. Koay, J. R. Mcconnell, Y. Wang, S. R. Mcalpine, RSC Advances 2015, 5, 59003-59013. R. P. Sellers, L. D. Alexander, V. A. Johnson, C.-C. Lin, J. Savage, R. Corral, J. Moss, T. S. Slugocki, E. K. Singh, M. R. Davis, S. Ravula, J. E. Spicer, J. L. Oelrich, A. Thornquist, C.-M. Pan, S. R. Mcalpine, Bioorg. Med. Chem. 2010, 18, 6822-6856. COMMUNICATION Entry for the Table of Contents (Please choose one layout) Layout 1: COMMUNICATION Text for Table of Contents Yao Wang, Yen Chin Koay, Shelli R McAlpine* Hsp90 Hsp90 Page No. – Page No. KnockDown C-terminal Hsp90 modulator Redefining the phenotype of Hsp90 inhibitors Phenotype A Classical Inhibitor AUY922 Phenotype B hihere))