* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiology
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Artificial heart valve wikipedia , lookup
Echocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Rheumatic fever wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Aortic stenosis wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
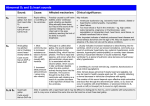
Internal Medicine Board Review – Cardiology III th July 16 , 2015 Topics EKG’s and arrhythmias/conduction abnormalities Myocardial Disease and Cardiomyopathies Pulmonary artery catheters and hemodynamic data interpretation Syncope Valvular heart disease HOLD ON!!! Approach to EKG’s Always read the question stem first to know what you are looking for Think about the clinical context; may not even need the tracing Look for patterns that fit the clinical situation Dissect the EKG in your usual systematic way EKG interpretation Use your system, whatever it is ie. Mechanism, Structure, Function If the question includes multiple tracings, it is usually looking for a pattern; beware that two are likely very similar. ie. Mitral stenosis Don’t forget you can use paper/pencil as “poor man’s calipers” EKG interpretation May include 12 lead, 6 lead, 3 lead or rhythm strips Pay attention to which leads you are given (and the order/arrangement) Look for standardization if voltage is relevant (ie. LVH, tamponade) Count big blocks for heart rate (300, 150, 100, 75, 60…) Remember, each small block is 0.04 seconds Frequently Seen Tracings On Boards Conduction Abnormalities AV block, LBBB, RBBB Bradyarrhythmias Sinus brady, A-fib with junctional escape Atrial Tachyarrhythmias Sinus tach, A-fib, A-flutter, AVNRT, MAT Ventricular Arrhythmias VT, AIVR, torsades Acute Infarction (Identify the vascular distribution) Pericarditis Tamponade WPW (ventricular pre-excitation) Long QT syndrome Electrolyte Disturbances Hyperkalemia, hypo/hypercalcemia Normal 1st degree AV block 2nd degree - Mobitz I (Wenckebach) 2nd degree (Mobitz II) AV Block 2:1 AV Block 3rd degree AV block Left Bundle Branch Block Right Bundle Branch Block Sinus Bradycardia Sick Sinus Syndrome Atrial Fibrillation with Heart Block and Junctional Escape Premature Atrial Contractions Premature Ventricular Contractions Sinus Tachycardia Atrial Fibrillation Atrial Flutter (2:1 conduction) Atrial Flutter (4:1 conduction) Multifocal Atrial Tachycardia AV Node Reentrant Tachycardia Ventricular Tachycardia Frequent PVC’s and Nonsustained Ventricular Tachycardia Ventricular Tachycardia Torsades de Pointes Torsades de Pointes AIVR (Accelerated Idioventricular Rhythm) AIVR (Accelerated Idioventricular Rhythm) LVH with Repolarization Abnormalities or Hypertrophic Cardiomyopathy Tamponade (low voltage with electrical alternans) Low voltage (amyloid) Anterior Acute Infarction (LAD) Inferior Acute Infarction (RCA) Posterolateral Acute Infarction (Circumflex) Pericarditis Ventricular Pre-excitation (WPW) Atrial Fibrillation with WPW Long QT syndrome Brugada Syndrome S1Q3T3 (Pulm embolus) Ventricular Pacemaker Pacemaker Failure to Capture Hyperkalemia Hyperkalemia Hypo/hypercalcemia ANY QUESTIONS on EKG’s???? QUESTION #1 A 56 y/o man with ischemic cardiomyopathy is being maintained on a medical regimen of furosemide 40mg twice daily, spironolactone 25mg daily, enalapril 10mg twice daily, digoxin 0.125mg daily, and carvedilol 6.25mg twice daily. In an attempt to titrate up to the target dose of 25mg BID (the dose shown to have the greatest mortality benefit), the carvedilol is increased to 12.5mg BID. Five days later, the patient returns due to worsening dypsnea on exertion and orthopnea. Physical exam is consistent with mild volume overload. Which of the following steps in this patient’s management is most appropriate at this time? A. B. C. D. E. Decrease the dose of enalapril Discontinue the digoxin Discontinue the spironolactone Increase the dose of furosemide to reestablish euvolemia Discontinue the carvedilol QUESTION #2 You are working in an emergency department when a 72 year old woman presents with increasing shortness of breath over the past 12-24 hours. She has a diagnosis of heart failure after a myocardial infarction several years ago. She has been prescribed an excellent medical regimen, but she has been intermittently compliant recently. On presentation her vital signs reveal a heart rate of 94, blood pressure of 196/110, respiratory rate of 24, and oxygen saturations of 85% on room air. Physical exam reveals no significant peripheral edema, normal jugular venous pressure, an S4 gallop, and rales in the bilateral lung bases. EKG shows sinus mechanism, evidence of an old anterior infarct, and nonspecific st-t wave changes which is unchanged from her EKG 6 months ago. CXR shows moderate pulmonary congestion. Complete blood count and basic metabolic panel are unremarkable. Which of the following would the most appropriate NEXT step in the management of this patient? A. B. C. D. E. Emergent endotracheal intubation with mechanical ventilation Place an intra-aortic balloon pump Take measures to lower the systemic blood pressure, such as administering an ACE-I or intravenous nitrates High dose intravenous diuretics Obtain serum cardiac biomarkers to rule out myocardial infarction QUESTION #3 All of the following statements regarding heart failure are true EXCEPT: A. B. C. D. E. Heart failure is defined as the inability of the heart to pump blood to the vital organs at normal filling pressures. Heart failure now is the most common hospital discharge diagnosis in Medicare patients. The diagnosis of heart failure is excluded by demonstrating normal left ventricular systolic function on echocardiogram. Heart failure is increasing in prevalence due to the aging population and better treatment and salvage of patients with acute myocardial infarction Heart failure is now responsible for greater than 1 million hospitalizations in the United States each year. Myocardial disease Cardiomyopathies Etiology Reversibility Heart failure treatment Cardiomyopathies - Etiology Ischemic Hypertensive Toxin induced ie. EtOH, anthracyclines Metabolic/Infiltrative ie. thyroid, amyloid Associated with general systemic disease ie. MD’s, CTD’s Peripartum Hypertrophic Valvular ie. AS, AI, MR Inflammatory/Infectious ie. post-viral myocarditis, HIV, Chaga’s Idiopathic Familial Question on Myocardial Dz???? QUESTION #4 A 22 year old woman is admitted to the ICU with profound hypotension. She developed a cardiomyopathy 4 months ago after delivery of her first child and was found to have an ejection fraction of 25%. She has done well since that time until today, when she was found unresponsive by family members. Heart rate is 145 bpm with a blood pressure of 86/45 on dopamine. A pulmonary artery catheter is placed to help guide management with the following hemodynamic measurements: QUESTION #4 (con’t) Right Atrial Pressure Wedge Pressure Cardiac Output Systemic Mixed Vascular Venous O2 Resistance Saturation 6 mm Hg (normal) 11 mm Hg (normal) 14 L/min (elevated) 450 87% dynes/sec/cm5 (elevated) (low) QUESTION #4 (con’t) Which of the following is the most appropriate next step in the management of this patient? A. Place an intra-aortic balloon pump and begin workup for heart transplant B. Begin high dose dobutamine C. CT chest to evaluate for pulmonary embolus D. Large boluses of isotonic intravenous fluids E. Draw blood/urine cultures, broad spectrum IV antibiotics, and support with vasopressors PA Catheters (Swan-Ganz) Hemodynamics in hypotension Cardiac Output PCWP RA SVR MISC. Pressure Hypovolemia Low Low Low High Tachycardia, Dry MM Sepsis High Low or normal Low or normal Low Low O2 extr. (High MV O2) Cardiogenic Low High High or normal High High O2 extr. (Low MV O2) Neurogenic Normal or Low or high normal Low or normal Low May be bradycardic Pulmonary Embolus Low Normal or High high Low Very high PVR Questions on PA catheters or hemodynamics???? QUESTION #5 You are consulted by a psychiatrist to see a 17 year old woman admitted 4 days ago with newly diagnosed psychosis. The patient has had several episodes of witnessed syncope in the past 2 days. The patient is very stoic and unable to provide any history. The H&P on the chart states that 2 first degree relatives have died at early ages in their sleep, thought to be due to “heart attacks.” Complete blood count and chemistries are within normal limits. An EKG is obtained and is shown. QUESTION #5 EKG QUESTION #5 (con’t) Which of the following is the most appropriate initial recommendation at this time? A. Obtain an echocardiogram to evaluate for hypertrophic cardiomyopathy B. Perform cardiac MRI to evaluate for arrhythmogenic right ventricular dyplasia C. Transfer patient to a telemetry unit to evaluate for supraventricular arrythmias D. Perform tilt table testing to evaluate for vasovagal syncope E. Discontinue medications that are known to prolong the Qtc interval Syncope Sudden transient loss of consciousness and postural tone with spontaneous recovery without neurologic deficit Differentiate from seizure, SCD Diagnosis on boards (and in practice) should be made by history, history, history, physical exam, or EKG ECHO only when structural heart disease is likely Additional studies guided by history and the clinical suspicion of specific disorders Syncope (hints to specific causes) Young athlete with systolic murmur – Hypertrophic Cardiomyopathy Older patient with systolic murmur – Aortic Stenosis Young patient with prodrome, prolonged standing, or at church – Vasovagal Older patient on multiple HTN meds – Orthostasis Head rotation or shaving – Carotid Sinus Sensitivity Arm exercise – Subclavian Steal Syndrome With exertion – AS, HCM, MS, Pulm HTN Older patient with paroxysmal A-fib – Sick Sinus Swimmer – look for long QT Valvular Heart Disease 69 Breaking It Down Valvular heart disease (2-5 questions) Aortic stenosis – elderly vs younger Aortic regurgitation – Marfan’s or endocarditis MVP – maneuvers, SBE prophylaxis HCM – sudden death in an athlete, maneuvers Mitral stenosis – rheumatic heart disease Tricuspid stenosis with carcinoid patient Tricuspid regurgitation in a patient with right heart failure 70 Question What’s the diagnosis? 71 Aortic Stenosis Scenarios – middle aged adult with bicuspid valve, older adult (> 70) with tricuspid valve Diagnosis Symptoms are chest pain, syncope, CHF PE shows 3-4 SEM at RUSB radiating to carotids, pulsus parvus et tardus (weak and delayed upstrokes) Tests – echo, cath only as pre-op for CAD Mgt – surgery when symptoms develop or if EF <50%, balloon valvuloplasty is only palliative and short-lived 72 Aortic Regurgitation Scenario – Marfan’s syndrome, endocarditis Diagnosis – shortness of breath, early highpitched decrescendo diastolic murmur at left or right upper sternal border, wide pulse pressure, brisk pulses Test – echo +/- CXR if dissection Mgt – afterload reduction with ACE inhibitor or nifedipine, valve replacement for EF < 50% or LVESD > 55mm (or LVEDD > 75mm) 73 Aortic Regurgitation 74 MVP Favorite board question Scenario – young woman with palpitations, chest pain Diagnosis – mid-systolic click with late systolic murmur, increases with Valsalva Test – echo Mgt – beta blocker for symptoms, valve repair only for severe regurgitation SBE prophylaxis no longer recommended** 75 MVP What’s the diagnosis? 77 Hypertrophic Cardiomyopathy 78 Hypertrophic Cardiomyopathy Favorite board question Scenario – young athlete with syncope or aborted sudden death, SOB, diastolic heart failure Diagnosis – SEM at RUSB which increases with Valsalva, brisk carotid upstrokes, S4, pulsus bisferiens Test – EKG with LVH and T wave inversion, echo Mgt – beta blockers and calcium channel blockers, surgical or percutaneous myectomy, ICD placement if high risk for sudden death, no competitive athletics except golf and bowling, screening of first- and second-degree relatives 79 80 HCM EKG 81 Differentiating Aortic Stenosis from Hypertrophic Cardiomyopathy Same Both may present with syncope Both have a harsh SEM radiating to the carotids Different HCM usually younger than AS Carotid upstrokes are brisk with HCM, diminished with AS Murmur gets louder with Valsalva with HCM, softer with Valsalva with AS 82 What’s the diagnosis? 83 Mitral Stenosis Yet another favorite board question Scenario – woman with history of rheumatic heart disease Diagnosis – DOE, palpitations, PND, diastolic rumble with loud S1 and opening snap just after S2, small PMI, palpable P2, rales Tests – echo, TEE to grade valve Mgt – slow heart rate to improve diastolic filling time – beta blockers, balloon valvuloplasty is the first line procedure for these pts (as opposed to AS) SBE prophylaxis no longer recommended** 84 85 Question A 51 year old man… verbose description… with a diastolic murmer…. more and more words… echo confirms tricuspid stenosis (MAN!!??) What is the most likely etiology? 1. 2. 3. 4. Senile calcification Carcinoid Ebstein’s anomaly Rheumatic fever 86 Tricuspid Regurgitation Not a likely test question, but may see a case of pulm HTN with TR and also PR Scenario – young woman with severe SOB, hypoxia, and right heart failure – edema, ascites, elevated JVP, large v wave, pulsatile liver Diagnosis – echo, right heart cath, CTA – must rule out other etiologies – CTD, congenital heart disease, recurrent PE Mgt – poor prognosis if no reversible cause, O2, calcium blockers, Coumadin, prostacyclin analogs (epoprostenol), endothelin receptor antagonists (bosentan), phosphodiesterase-5 inhibitors (sildenafil), lung transplantation 87 QUESTIONS ON ANYTHING????