* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Low potential of dobutamine and dopexamine to block intestinal
Prescription costs wikipedia , lookup
Toxicodynamics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Plateau principle wikipedia , lookup
Gastrointestinal tract wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Drug interaction wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Environmental persistent pharmaceutical pollutant wikipedia , lookup
Neuropharmacology wikipedia , lookup
Epinephrine autoinjector wikipedia , lookup
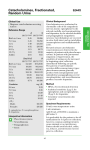
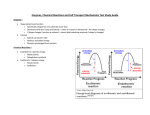
Low potential of dobutamine and dopexamine to block intestinal peristalsis as compared with other catecholamines Sonja Fruhwald, MD; Stefan Scheidl; Wolfgang Toller, MD; Thomas Petnehazy; Peter Holzer, PhD; Helfried Metzler, MD; Heinz F. Hammer, MD Objective: Catecholamines are frequently used in critically ill patients to restore stable hemodynamics and to improve organ perfusion. One effect of short-term or long-term administration of catecholamines may be inhibition of propulsive motility in the intestine. We therefore analyzed the effect of dopexamine, dobutamine, and dopamine on ileal peristalsis and compared their action with that of epinephrine and norepinephrine, which have long been known to suppress intestinal peristalsis. Design: In vitro study on excised guinea pig ileum segments. Setting: Laboratory for experimental studies at the University. Subjects: Isolated guinea pig ileum. Interventions: Segments of ileum excised from guinea pigs were mounted in a tissue bath in Krebs-Henseleit solution and bubbled with 95% oxygen/5% CO2. Luminal perfusion with the same solution was performed at a rate of 0.35 mL/min. The bath temperature was kept at 36.5°C. Peristalsis was recorded via changes in the intraluminal pressure. The drugs under investigation (dopamine, epinephrine, norepinephrine, dobutamine, and dopexamine) were added to the tissue bath. C atecholamines are frequently used in critically ill patients with low cardiac output syndrome to improve global hemodynamics and/or regional perfusion. Their effects on the human splanchnic region may be divided into indirect effects, which result from beneficial or detrimental impact on splanchnic perfusion, and direct effects on intestinal motility. Experimental and clinical research on the effect of catecholamines on the gastrointestinal tract currently focuses primarily on their indirect effects because of changes in cardiac output and splanchnic perfusion (1–7). Despite the beneficial ef- From the Departments of Anesthesiology and Intensive Care (Drs. Fruhwald, Toller, Metzler), Internal Medicine (Dr. Hammer, Mr. Scheidl, Mr. Petnehazy), and the Institute of Pharmacology (Dr. Holzer), University of Graz, Graz, Austria. Address requests for reprints to: Heinz F. Hammer, MD, Associate Professor of Medicine, Medizinische Universitaetsklinik, Auenbruggerplatz 15, A-8036 Graz, Austria. E-mail: [email protected] Copyright © 2000 by Lippincott Williams & Wilkins Crit Care Med 2000 Vol. 28, No. 8 Measurements and Main Results: Low concentrations of each catecholamine, except epinephrine, caused a decrease in the pressure threshold, which reflects a stimulatory effect on peristalsis. Higher catecholamine concentrations caused a concentration-related increase in the threshold, cumulating in a complete block of peristalsis. The rank order of inhibitory potency was epinephrine > norepinephrine > dopamine > dobutamine ⬃ dopexamine. Dobutamine and dopexamine were about 500-fold less active than epinephrine in suppressing peristalsis. Conclusions: This study shows that dobutamine and dopexamine have the least potential to block propulsive motility in the intestine, whereas epinephrine demonstrates the most adverse inhibitory effect. Because at low concentrations dobutamine and dopexamine even stimulate peristalsis, these drugs appear to be superior compared with other catecholamines with regard to their direct effects on intestinal motility. (Crit Care Med 2000; 28: 2893–2897) KEY WORDS: guinea pig; ileum; threshold; peristalsis; dopamine; epinephrine; norepinephrine; dobutamine; dopexamine; motility fects of catecholamines on cardiac output and overall splanchnic circulation, catecholamines do not necessarily improve blood flow to the gastrointestinal mucosa. Dopamine, for instance, increases splanchnic perfusion but causes a redistribution of blood flow from the mucosa to the muscularis, which may lead to mucosal dysfunction, promote bacterial translocation, and eventually give rise to multiple organ failure (8, 9). A well-established action of the older catecholamines epinephrine and norepinephrine on the gut, which may limit their therapeutic usefulness, is the inhibition of propulsive intestinal motility (10 –13). This effect is primarily a result of inhibition of acetylcholine release from enteric neurons (11, 13, 14). New catecholamines, such as dobutamine and dopexamine, have been introduced into clinical routine. They are used alone or in combination with traditional catecholamines with the aim of improving regional hemodynamic effects (1, 6). It is not known whether these catecholamines also inhibit peristalsis and, if so, how the potency of such effects compares with that of epinephrine and norepinephrine. We therefore set out to compare the actions of catecholamines currently in clinical use on peristalsis in the isolated guinea pig ileum. The experimental model, which uses a fluid-perfused segment of ileum, allows a quantitative assessment of direct drug effects on peristalsis independent of circulatory changes (15, 16). To allow comparison of the potency of five catecholamines (epinephrine, norepinephrine, dopamine, dobutamine, and dopexamine), concentration response curves were constructed for each drug. MATERIALS AND METHODS Animals and Assay Arrangement. Guinea pigs were obtained from the Central Research Institute for Laboratory Animal Breeding, University of Vienna, Austria. The guinea pigs were fasted overnight with free access to water. The animals were killed by decapitation and the ileum was excised. Before the guinea 2893 Table 1. Composition of the Krebs-Henseleit solution Substance Concentration (mM) NaCl KCl CaCl2 MgSO4 NaHCO3 KH2PO4 Glucose 119 4.75 2.5 1.5 25 1.2 11 pigs were killed, all procedures for care were executed in accordance with national and international guidelines for the care and use of laboratory animals. After cleaning, the ileum was first equilibrated in Krebs-Henseleit solution (Table 1) and bubbled with 95% oxygen/5% CO2 for ⬃1 hr. In a second step, segments of ileum with a length of 6 cm were taken and mounted in a small volume (22 mL) tissue bath (Mayflower, Hugo Sachs Electronics, Freiburg, Germany) in Krebs-Henseleit solution, which was bubbled with 95% oxygen/5% CO2. The temperature of the tissue bath was kept at 36.5°C, whereas the pH of the Krebs-Henseleit solution was kept between 7.35–7.45. Peristaltic contractions of the mounted ileum segment were elicited by luminal perfusion with Krebs-Henseleit solution at a rate of 0.35 mL/min using a REGLO-Digital MS-4/6 – 100 roller pump (Ismatec, Germany) against an aboral pressure of 5 cm H2O. The peristaltic nature of the contractions was confirmed visually. Peristaltic contractions resulted in complete emptying of the segment. In total, 70% to 80% of the ileum segments developed repetitive peristaltic contractions and could be used for our experiments. Segments that did not show regular contractions were discarded. After a 15-min control period, the test drug was added to the organ bath and a 15-min test period was recorded. For each test drug and test concentration, a new segment was used. Test Drugs. The drugs used in the study were dobutamine (Dobutrex, Eli Lilly, Indianapolis, IN), dopamine (Dopamin, Fresenius, Austria), dopexamine (Dopacard, Fisons plc, Pharmaceutical Division, UK), epinephrine (Suprarenin, Hoechst, Austria), and norepinephrine (Arterenol, Hoechst, Austria). Each test substance was first examined at a concentration of 1 nM. In the following experiments, the concentration was increased to evaluate the effect of different catecholamine concentrations on intestinal motility. The drugs were administered into the bath to the serosal surface of the ileum, in volumes not exceeding 1% of the bath volume. Data Recording. Intraluminal pressure was measured at the oral end of the segment with a very low range differential pressure transducer (Validyne DP 45-XX, Hugo Sachs Electronics) and an amplifier (2-channel bridge 2894 amplifier, type 301, Hugo Sachs Electronics). Contractions were recorded with a Multi-Pen Recorder (R-OX, Hugo Sachs Electronics). The pressure curves of the mounted ileum segments were characterized by a slow initial rise of pressure to a threshold at which a peristaltic contraction was triggered (Fig. 1A). Then the cycle started anew. An increase in the threshold represents an inhibitory effect, whereas a decrease in the threshold reflects a stimulant action on peristalsis. Data Analysis. Each segment served as its own control. Paired Student’s t-test was used for statistical analysis. A p of ⬍ .05 was considered to be significant. The recordings were analyzed for a shift in the pressure threshold required for triggering a contraction. The effects of different catecholamine concentrations on peristaltic frequency were analyzed by measuring the distance between two consecutive contractions. RESULTS We tested five different catecholamines in at least six different concentrations. Analysis of the concentration response curves for pressure threshold showed significant qualitative and quantitative differences in the action of the different catecholamines on peristalsis. As shown in Figure 2, all catecholamines had a concentration-related increase in pressure thresholds, cumulating in a complete block of peristaltic activity. Epinephrine was the most effective inhibitor of peristalsis; significantly lower concentrations increased the pressure threshold as compared with the other catecholamines. Dopexamine and dobutamine were the least potent inhibitors; higher concentrations were necessary to show an effect on the pressure threshold. The highest concentrations of each catecholamine used in the study resulted in a block of peristalsis. The concentration that led to this block of peristalsis was significantly lower for epinephrine and norepinephrine as compared with the other catecholamines (Fig. 2). Figure 2 also shows that all substances, except epinephrine, caused a small, but significant, reduction in the pressure threshold in their lower concentration ranges. Effects of Different Catecholamines. Table 2 summarizes concentrations of maximum threshold reduction, halfmaximum catecholamine concentrations and maximal inhibitory concentrations (block of peristalsis). Epinephrine. Concentrations ⬍5 nM did not change the peristaltic activity of the ileum segment. Higher concentrations of epinephrine resulted in a concen- tration-dependent rise of the pressure threshold (Fig. 1B). At 100 nM, peristalsis was completely abolished (Fig. 1C). Epinephrine was the only catecholamine that did not decrease the threshold at lower concentrations (Fig. 2). At lower epinephrine concentrations, the frequency of peristaltic contractions increased (Fig. 1A), whereas at higher concentrations peristaltic frequency was reduced (Fig. 1B). Norepinephrine. Concentrations ⬍5 nM did not alter peristaltic motility. Concentrations between 5 and 25 nM led to a significant reduction of the threshold with a maximal effect at 10 nM. Higher concentrations resulted in an increase in the threshold and a complete blockade of peristalsis at 1 M. The frequency of peristaltic contractions was reduced at all concentrations tested. Dopamine. There was no effect on peristalsis with dopamine concentrations ⬍75 nM. A concentration of 100 nM led to a significant reduction of the threshold. Concentrations up to 5 M resulted in a small increase of the threshold, whereas higher concentrations led to a pronounced increase in the threshold, which resulted in a complete block of peristalsis at 50 M. The frequency of peristaltic contractions increased at dopamine concentrations between 10 and 25 nM. Higher concentrations of the drug reduced peristaltic frequency. Dobutamine. Dobutamine added to the tissue bath at concentrations ⬍1 M did not influence peristaltic motility (Fig. 3A). Concentrations between 1 and 10 M caused a significant reduction of the threshold. At bath concentrations of 15 to 25 M, the drug caused a moderate concentration-related increase in the threshold. A concentration of 30 M dobutamine led to a marked rise in the threshold, and at 50 M, a complete block of peristalsis was seen (Fig. 3B, C). The peristaltic frequency was reduced by dobutamine at all concentrations tested. Dopexamine. Dopexamine concentrations up to 1 M did not alter peristaltic motility. Concentrations between 1 M and 20 M lowered the peristaltic pressure threshold. At 30 M, no change in the threshold was found, whereas higher concentrations of the drug caused a marked increase in the threshold, and 50 M dopexamine completely suppressed peristalsis. All concentrations caused an initial increase in the peristaltic frequency, whereas after a few minutes a decrease of frequency was found. Crit Care Med 2000 Vol. 28, No. 8 Figure 2. Concentration response curves of the effect of different catecholamines on the pressure threshold of peristalsis. The effect of catecholamines on threshold is shown as the difference between thresholds before and after administration of the test substance (⌬threshold). Mean ⫾ SEM from six experiments performed at each concentration. Positive ⌬ threshold values represent inhibition of peristalsis and negative values represent stimulation of peristalsis. *significant values as compared with baseline. Table 2. Relevant catecholamine concentrations Figure 1. Effects of epinephrine on peristalsis in guinea pig ileum. The figures show original pressure recordings before and after administration (s) of epinephrine. Note the pressure threshold (T) at which peristaltic contractions were elicited. At 25 nM, the peristaltic frequency was increased. At 50 nM, the threshold increased markedly and the frequency decreased. At 100 nM, peristalsis was completely blocked, an effect that was irreversible during the test period (15 mins). DISCUSSION Our results demonstrate that catecholamines that are currently used in critically ill patients because of their cardiovascular effects differ markedly in their inhibitory and stimulatory actions on the peristaltic motility of guinea pig ileum in vitro. Dobutamine and dopexamine are ⬃500 times less potent in inhibiting peristalsis than epinephrine, which was the most active compound among the catecholamines tested. The rank order of inhibitory potency was as follows: epinephrine ⬎ norepinephrine ⬎ dopamine ⬎ dobutamine ⬃ dopexamine. The relative potency of epinephrine and norepinephrine corresponds with the potency reported by Mc Dougal and West (10). To our knowledge, the effects of the Crit Care Med 2000 Vol. 28, No. 8 Catecholamine Maximum Threshold Reduction Half-Maximum Catecholamine Concentration Block of Peristalsis 0.01 0.1 10 20 0.065 0.250 25 39 40 0.1 1 50 50 50 Epinephrine Norepinephrine Dopamine Dobutamine Dopexamine All concentrations given in M. other catecholamines on peristaltic motility have not been tested. The low inhibitory potency of dobutamine (1-adrenoceptor agonist) and dopexamine (2adrenoceptor agonist and dopamine receptor agonist) is, however, consistent with the finding that ␣-adrenoceptor agonists are more active in inhibiting acetylcholine release from enteric neurons and suppressing peristalsis than -adrenoceptor agonists (13, 17, 18). Other differences among the catecholamines concern the observation that all substances, except epinephrine, decreased the peristaltic pressure threshold at low subinhibitory concentrations, which means that they facilitated peristalsis at this concentration range. The relevance of this finding to propulsive motility in vivo remains to be determined. Another difference relates to the steepness of the concentration-response curves for peristaltic inhibition. The curves for norepinephrine and dopamine were flatter than those for the other tested substances, which is likely to reflect the involvement of different receptors and/or mechanisms. There were also differences in the catecholamine-induced changes of peristaltic frequency. Epinephrine, dopamine, and dopexamine increased the frequency, at least at subinhibitory concentrations. The increase in pressure thresholds at higher catecholamine concentrations was associated with a reduction of frequency. This was not evaluated further because peristaltic frequency in vitro is a complex variable dependent on infusion rate, intestinal compliance, peristaltic pressure threshold, and the efficiency of emptying. 2895 D obutamine and dopexamine have the least potential to block peristalsis; at low concentrations they even stimulate peristalsis. These drugs appear to be superior to other catecholamines with regard to their adverse effects on intestinal motility. Figure 3. Effect of dobutamine on peristalsis in guinea pig isolated ileum. The figures show original pressure recordings before and after administration (s) of dobutamine. Note the pressure threshold (T). At 100 nM, there is no influence on peristaltic contractions. A concentration of 30 M of dobutamine led to a marked increase in pressure thresholds, whereas at 50 M, peristalsis is completely blocked. 2896 Interpretation of frequency changes is therefore controversial (19). Furthermore, in contrast to changes in thresholds, which were constant during the whole observation period for each of the catecholamine concentrations tested, influences on peristaltic frequency were not constant. The opposite effects of low and high concentrations of four of the five tested catecholamines on motility are most likely attributable to stimulation of different receptors. Stimulation of different receptors at different catecholamine dosages has been demonstrated for the effect of dopamine on blood vessels. Low-dose dopamine (ⱕ3 g/kg/min) has a vasodilatory effect because of a stimulation of dopaminergic receptors. Doses ⬎5 g/ kg/min cause a stimulation of ␣-receptors and a vasoconstriction. In the present study, we have also observed dose-dependent switches of direct catecholamine effects. Except in the case of epinephrine, lower concentrations caused a reduction of the pressure threshold, and therefore a stimulation of intestinal contractility. The present observations concerning the peristaltic pressure threshold indicate that dobutamine and dopexamine have the least potential to block propulsive motility in the gut. This low potency in suppressing intestinal propulsion favors the use of dobutamine and dopexamine in critically ill patients, although this recommendation is only based on their effects on intestinal motility and does not take their effects on gut perfusion into account. Milder disturbances of intestinal motility are frequently seen in the intensive care setting. Serious abdominal complications are known to occur in 1.4% of patients after cardiac surgery and have a total mortality of 14.5% (20). Risk factors for severe abdominal complications in cardiac surgery include advanced age, prolonged aortic cross-clamping time, low cardiac output, and multiple organ failure. In experimental studies of pharmacologic effects on intestinal motility, addition of a pharmacologic substance to the organ bath rather than through the mesenteric vessels is commonly performed. Our data suggest that neither the timing nor quantitative aspects of the actions of catecholamines on the ileum are influenced by a possible diffusion barrier. As shown in Figures 1 and 3, the catecholamines had an immediate effect on peristaltic activity, which suggests that the time that is needed for diffusion of the catecholamine to their receptors was not a limiting factor of our preparation. In addition, as shown in the Figures 1 and 3, the catecholamine effect did not increase during the observation time, which suggests that there was no diffusion barrier which would have been overcome with time and which might possibly have influenced the quantitative aspect of the catecholamines. Although caution must be observed when our data from the guinea pig are applied to intensive care patients, some comparisons may shed light on potential clinical implications. Arterial plasma concentrations reach 23.9 nM in healthy volunteers after infusion of epinephrine at a rate of 0.2 g䡠kg⫺1䡠min⫺1 (21). In guinea pig ileum, comparable concentrations of epinephrine resulted in a stimulation of peristaltic frequency (Fig. 1A). There was no marked effect on the threshold of peristalsis at this concentration, but because the concentrationresponse curve of epinephrine is very steep, only slightly higher concentrations already cause a considerable inhibition of peristaltic contractility of the guinea pig ileum (Fig. 2). Infusion of norepinephrine in humans at a rate of 0.2 g䡠kg⫺1䡠 min⫺1 resulted in arterial plasma concentrations up to 44.1 nM (21). In the guinea pig ileum, comparable concentrations caused a marginal increase of the threshold. Because the concentration response curve of the effects of norepinephrine on motility is flatter, the margin of safety for the therapeutic use of norepinephrine may be bigger as compared with epinephrine. Plasma concentrations of dobutamine at an infusion rate of 10 g䡠kg⫺1䡠min⫺1 reach about 0.6 M, and plasma concentrations of dopexamine at an infusion rate of 4 g䡠kg⫺1䡠min⫺1 reach 0.4 M (22, 23). As can be seen in Figure 2 these concentrations have no effect on intestinal motility. Higher concentrations would stimulate motility, before at even higher concentrations inhibition of motility would occur. From the point of ileal motility, our data therefore support the suggestion of Meier-Hellmann et al. (4) and Levy et al. (1) that a combination of norepinephrine and dobutamine may be preferable over an epinephrine monotherapy. This combination of drugs has also recently been suggested to be used in septic patients, by the Task Force of the American College of Critical Care Medicine (24). Crit Care Med 2000 Vol. 28, No. 8 In conclusion, our in vitro study compared the different effects of clinically used catecholamines on intestinal motility. We demonstrated that these catecholamines differed profoundly in their action on intestinal motility. Of the tested substances, dobutamine and dopexamine have the least potential to block peristalsis; at low concentrations they even stimulate peristalsis. These drugs appear to be superior to other catecholamines with regard to their adverse effects on intestinal motility. 7. 8. 9. REFERENCES 10. 1. Levy B, Bollaert PE, Charpentier C, et al: Comparison of norepinephrine and dobutamine to epinephrine for hemodynamics, lactate metabolism, and gastric tonometric variables in septic shock: A prospective randomized study. Intensive Care Med 1997; 23: 282–287 2. Leier CV: Regional blood flow responses to vasodilators and inotropes in congestive heart failure. Am J Cardiol 1988; 62:86E–93E 3. Bersten AD, Hersch M, Cheung H, et al: The effect of various sympathomimetics on regional circulations in hyperdynamic sepsis. Surgery 1992; 112:549 –561 4. Meier-Hellmann A, Reinhart K, Bredle DL, et al: Epinephrine impairs splanchnic perfusion in septic shock. Crit Care Med 1997; 25: 399 – 404 5. Meier-Hellmann A, Reinhart K: Effects of catecholamines on regional perfusion and oxygenation in critically ill patients. Acta Anaesthesiol Scand 1995; 107:239 –248 6. Martin C, Viviand X, Potie F: Use and misuse of catecholamines: Combination in septic Crit Care Med 2000 Vol. 28, No. 8 11. 12. 13. 14. 15. 16. shock patients. In: Yearbook of Intensive Care and Emergency Medicine. Vincent JL (Ed). Berlin, Springer-Verlag, 1997, pp 289 –301 Meier-Hellmann A, Sakka S, Reinhart K: Aspects in monitoring and treatment of gastrointestinal underperfusion in sepsis. Diagnosis and therapy of gastrointestinal underperfusion in sepsis. Anesthesiol Intensivmed Notfallmed Schmerzther 1998; 33 (Suppl 2): 60 – 69 Giraud GD, Mac Cannell KL: Decreased nutrient blood flow during dopamine- and epinephrine-induced intestinal vasodilatation. J Pharmacol Exp Ther 1984; 230:214 –220 Carricio CJ, Meakins JL, Marshall JC, et al: Multiple-organ-failure syndrome. The gastrointestinal tract: The “motor” of MOF. Arch Surg 1986; 121:196 –208 Mc Dougal MD, West GB: The inhibition of the peristaltic reflex by sympathomimetic amines. Br J Pharmacol 1954; 9:131–137 Doherty NS, Hancock AA: Role of alpha-2 adrenergic receptors in the control of diarrhea and intestinal motility. J Pharmacol Exp Ther 1983; 225:269 –274 Kazic T: Effect of adrenergic factors on peristalsis and acetylcholine release. Eur J Pharmacol 1971; 16:367–373 Frigo GM, Lecchini S, Marcoli M, et al: Changes in sensitivity to the inhibitory effects of adrenergic agonists on intestinal motor activity after chronic sympathomimetic denervation. Naunyn Schmiedebergs Arch Pharmacol 1984; 325:145–152 Paton WDM, Vizi ES: The inhibitory action of noradrenaline and adrenaline on acetylcholine output by guinea-pig ileum longitudinal muscle strip. Br J Pharmacol 1969; 35:10 –28 Bülbring E, Crema A, Saxby OB: A method for recording peristalsis in isolated intestine. Br J Pharmacol 1958; 13:440 – 443 Holzer P, Scluet W, Maggi CA: Substance P 17. 18. 19. 20. 21. 22. 23. 24. stimulates and inhibits intestinal peristalsis via distinct receptors. J Pharmacol Exp Ther 1995; 274:322–328 Holzer P, Lembeck F: Effect of neuropeptides on the efficiency of the peristaltic reflex. Naunyn Schmiedebergs Arch Pharmacol 1979; 307:257–264 Marcoli M, Lecchini S, De Ponti F, et al: Subsensitivity of enteric cholinergic neurones to ␣2-adrenoceptor agonists after chronic sympathetic denervation. Naunyn Schmiedebergs Arch Pharmacol 1985; 329: 271–277 Waterman SA, Tonini M, Costa M: The role of ascending excitatory and descending inhibitory pathways in peristalsis in the isolated guinea-pig small intestine. J Pharmacol 1994; 481:223–232 Simic O, Strathausen S, Geidel S, et al: Abdominal complications after heart surgery interventions. Zentralbl Chir 1997; 122: 893– 897 Ensinger H, Weichel T, Lindner KH, et al: Relationship between arterial and peripheral venous catecholamine plasma concentrations during infusion of noradrenaline and adrenaline in healthy volunteers. Eur J Clin Pharmacol 1992; 43:245–249 Leier CV, Unverferth DV, Kates RE: The relationship between plasma dobutamine concentrations and cardiovascular responses in cardiac failure. Am J Med 1979; 66: 238 –242 Baker PR, Gardner JJ, Lockley WJS, et al: Determination of dopexamine hydrochloride in human blood by high-performance liquid chromatography with electrochemical detection. J Chromatogr B Biomed Appl 1995; 667:283–290 Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine: Practice parameters for hemodynamic support of sepsis in adult patients in sepsis. Crit Care Med 1999; 27:639 – 660 2897