* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular System
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial septal defect wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
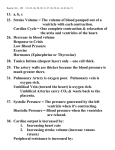
Cardiovascular System The component of the cardiovascular system are blood, the heart, and the blood vessels. The heart pumps blood through the circulatory system (an extensive closed system of blood vessels that carry blood to and from nearly every cell in the body). The heart is a hollow muscular organ located in the mediastinum. Its function is to pump blood to all parts of the body. The layers of the heart wall include the endocardium, the myocardium, and the epicardium. The heart is surround by the pericardial sac, which has a fibrous layer and a serous layer continous with the epicardium. The pericardial cavity (filled with pericardial fluid) and lies between the heart and the pericardial sac. The endocardium consist of a signle layer of endothelial cells on the surface and several underling layers. Beneath the endocardium, there is a specialized tissue (derived from muscle tissue) that responsible for initiating and conducting impulse to cause the heart muscle to contract. The myocardium is the muscular part of the heart that make up about three- fourth of the heart s bulk. It is composed of cardiac muscle. The epicardium (or visceral pericardium) is a serow membrane that covers the muscular part of the heart. Cardic muscle has several distinctive 1- Its fibrous undergo extensive branching. 2-Its cells are connected by intercalated disc through wich action potential easily move. 3-Its fiber are striated. 4-Its control is involuntary. The general anatomical plan of the heart The heart consists of a left and a right pump, each of which has an atrium and ventrical. The left and right sides of the heart are separated by the interatrial and interventricular septa. Valves separate the atria from the ventricles and the ventricles from the arteries leaving the heart: 1-The tricuspid valve separates the right atrium and ventricle. 2-The bicuspid (mitral) valve separates the left atrium and ventricle. 3-Aortic valve separates the left ventricle and aorta. 4-Pulmonary valve separates the right ventricle and pulmonary artery. 1 Blood flow through the heart chambers Blood enters the heart from the arterior and posterior venae cavae and passes through the following structures 1-right atrium 2-tricuspid valve 3-right ventricle 4-Pulmonary valve to the pulmonary artery and lung tissue 5-from lung tissue and pulmonary veins to the left atrium 6-bicuspid(mitral) valve 7-left ventricle 8-aortic valve to the aorta and different body tissues. Impulse-Generation Conducting System of the Heart and Innervation The impulse-generating and conducting system of the heart consist of several structures that make it possible for the atria and ventricles to beat in succession and permit the heart to function as an effective pump. 1-The sinoatrial node(S-A node) The pacemaker of the heart, since it has the most rapid rhythmic activity. It is located close to the entrance of superior vena cave into the right atrium. The nodal cells are modified cardiac muscle cells, smaller than atrial muscle cells and with fewer myofibrils. Nodal cells are concentration arranged around a large nodle artery. 2-Internodle tracts Specialized cells that conduct the electrical depolarization of the S-A node to the A-V node. 3-Mass of specialized cardiac muscle cells lies beneath the endocardium of the septal wall of the right atrium. The nodle cells are similar to those of the S-A node. In addition, there are large arteriol present as well as considerable amounts of adipose tissue. 4-Bundle of Hiss (or called atrio ventricular bundle of His) is formed by purkinje cells that penetrate the fibous skeleton of the heart and then divide to four the right and left bundle branches. The left bundle again divides to form 2 fascicles. These bundle of purkinje cells travel in the subendocardial layer to the apex of the heart where they reverse their direction and begin giving 2 off side branches that make contact with ordinary (working) cardiac muscle cells via gap junction. Owing to this arrangement the stimulus for ventricular contraction is rapidly conducted to the apex of the heart which , must contract first to eject blood from the ventricles. Then, the wave of contraction sweep toward the base of the heart (pulmonary valve and aortic valve). Purkinje cells has a diameter considerably greater than ordinary cardic muscle cells (30µm versus 15µm) but are somewhat shorter (20-50µm versus 80µm). It is the greater diameter of purkinje cells that responsible for the rapid conduction of electrical activity. Purkinje cells have one or 2 centrally placed nuclei, an abundance of glycogen and few peripherally disposed myofibrils. These cells are united longitudinally by intercalated discs. Innervation of the heart Both the parasympathetic and sympatheticm division of the ANS contribute to innervate the heart and from wide spread plexuses at the base of the heart. In the regions close to the S-A node and A-V node gauglionic nerve cells and nerve fibers are present. It is known that these nerves do not affect generation of the heart beat which is a precess attributed to the S-A node. These nerves do affect heart rhythm, where by stimulate of the parasympathetic division (vagus nerve) promotes a slowing of the heart beat, where as stimulation of the sympathetic nerve accelerates the rhythm of the pacemaker (S-A node). 3 4 5 Excitability of Cardic muscle A-B= resting membrane potential B-C= refractory period 1-depolarization 2-repolarization 3-plateau( permeability to K+ and both Na+Ca++) *The heart is absolutely refractory which means during this period additional action potential can not be produced no matter how strong the stimulus. For this reason the cardiac muscle can not be tetanized because of this long refractory period (20 msec), which the skeletal muscle has very short refractory period (1msec) so it can be tetanized by repetitive stimuli. The Conductive System of the Heart 1-S-A node (normal pacemaker) 2-A-V node 3-Bundle of His a- left branch b-right branch 4-Purkinje fibers. *Other regions of the heart that initiate action potential beat under abnormal conditions are called ectopic pacemaker. These region like A-V node, purkinje fiber, atrial myocardium and ventricular myocardium. The abnormal condition are : 1-very high rhythmicity of these region 2- low rhythmicity ofs-A node 3-This leads to block the conduction system * The frequency of discharge of S-A node is varied by : 1-the rate of depolarization 2-the threshold potential 3-the resting potential *The frequency is controlled by the activity of the autonomic nervous system. a-Increased vagal activity through the release of Ach(parasympathetic) will diminish the heart rate by: 1-reducing the slope of action potential 2-by producing a greater resting potential 6 b- Increased sympathetic activity through the release of nor epinephrine will increase the heart rate (principally by increasing the slope of action potential). *How the autonomic mediators (Ach and NE) change the slope of pacemaker action potential? Ach will decrease the permbility of membrane to K+ while NE will do the opposite. *From the S-A node, the cardiac impulse (wave of excitation) spreads radially throughout the atria (left and right) at a conduction velocity of 1m/sce. *The conduction from atria to ventricles is through the A-V node and the bundle of His. The conduction through the A-V node is delayed for about 100 msec. to allow the atria to contract befor ventricular contraction (conduction velocity= 0.05m/sec). *The excitation then spread through purkinje fibers(conduction velocity= 1-4m/sec. to the left and right ventricles). * The A-V conduction system is frequently the site of blocks due to : 1-nervous factors 2-inflammatory factor like rheumatic fever 3pharmacological factor like digitalis and its derivtives. Cardia Cycle Is one of heart beat or one cycle of contraction and relaxation of the cardiac muscle. *The main function of the heart is to generate the pressures which produce blood flow. The valves serving to direct the flow. At peak of P-wave of ECG(atrial depolarization) contraction of atria will takes place which will be rapidly followed by contraction of the ventricles at the peak of R-wave (ventricular depolarization). *The cardiac cycle is divided into two phases: 1- Systole (pumping of blood): period of ventricular contraction. 2-Diastole(filling of the heart): period of ventricular relaxation. During diastole: 1-the atria and ventricles are relaxed so the pressure inside the atria is higher than in the ventricles because : a- blood entering to left atrium from pulmonaryVeins. b-blood entering to right atrium from the venae cavae. 7 2-Therefor, the A-V valves are opened and blood is passing from atria to ventricles, so the ventricles will be filled to about 70-80% during diastole (before atrial contraction). 3-The aortic and pulm. Valves are closed because the aorta and pulm. Artery pressures are higher than the ventricular pressure. 4-At the end of diastole, the S-A node discharge so the atria will depolarization, then contract to push more blood th the ventricles. *The amount of blood in the ventricles before systole is called end diastolic volume. During systole 1-The wave of depolarization passes through the ventricles which will be followed by ventricular contraction, so the pressure inside the ventricles will exceed the atrial pressure, so that the A-V valves will be closed to prevent back flow of the blood into the atria. 2-Then the aortic and pulmonary valves will be opened because the ventricles pressure is higher than that of aortic and pulm. Pressure. So ventricular ejection occurs. *The ventricles dose not empty completely. The amount of blood remain after ventricular ejection is called end systolic volume. 3-After that the ventricles will relaxe so the ventricular pressure will falls below the aortic and pulm. Valves will be closed. Heart Sounds Are the sounds result from vibrations caused by valval closure which can be heard by using a stethoscope placeon the chest wall. 1-First sound (lub): of low intensity and associated with the closure of the A-V valves at the beginning of systole. 2-Second sound (Dup): of high intensity and associated with closure of pulm. And aortic valves at the begening of diastole. *These sounds are normal but heart murmurs are assign of heart disease. Heart murmurs are noise or turbulent sounds happens in valve stenosis or valve regulation. 8 Heart Sound The Electrocardiogram(ECG) Is a record of the electrical activity associated with the contraction of cardiac muscle. Or it is a tool for evaluating the electrical events within the heart. Differences of potential are recorded between two points on the skin. The action potential of the cardic muscle is like battery which cause current flow throughout the body fluids. These currents produce voltage differences at the body surface which can be detected by metal plate electrodes. The uses of ECG is valuable for: 1-detect the anatomical orientation of the heart. 2-detect the size of the chambers. 3-detect the disturbances of rhythm and conduction. 4-detect the extent, location and progress of myocardial ischemia. 5-detect the effect of changed electrolyte concentration. 6-detect the influence of certain drugs (like digitalis). Normal ECG P-wave= atrial depolarization Q-wave=depolarization of ventricular septum R-wave=depolarization of the ventricular free wall from endocardium to pericardium S-wave=depolarization of the base of the ventricles T-wave=repolarization of ventricles 9 P-R interval: is the time from the onest of atrial activation to the onest of ventricular activation. Normally range from 0.12 to 0.20 seconds. QRS interval: is the time of ventricular activation which is followed by compete ventricular contraction. Normally range (0.06-0.10 sec.). Pathological prolongation of this internal indicates a block in the ventricular conduction (block of left and right purkinje fibers). S-T interval: is the time of depolarization of the entire ventricular myocardium. Ay deviation in this period may indicate ischemic damage of the myocardium. Standard limb leads Leads means recording electrodes located on the skin. Lead system was first devised by William Einthoven(1860-1927), he consider the heart lies in the center of a triangle formed by the left and right shoulders and the pubic region (this is called Einthoven triangle). The standard limb leads (electrod are connected to the left arm, right arm and left leg. Lead I: record the potential differences between LA and RA. Lead II: between RA and LL. Lead III: between LA and LL. Arrhythmias 1-Sinus tacchycardia and sinus bradycardia: due to increase or decrease S-A node discharge leading shorten the P-R interval (in tacchycardia) or length the P-R interval (in bradycardia). 2-Atrioventricular block (A-V block) a-first degree:Characterized by prolongation P-R interval (greater than 0.2 sec.) b-Second degree: not all P-wave followed by QRS 10 c-Third degree:is complete heart block(the atrial and ventricular rhythm are independent) usually it is associated with syneape due to insufficient cerebral blood flow . In this case artificial pacemaker are used to insure normal ventricular frequency. 3-Premature systoles: due to ectopic foci. Ectopic foci S-A nodeتعني حصول تحفيز من منطقة غير a-Premature atrial systole:characterized by inverted P-wave and there is normal QRS b-Premature ventricular systole: the QRS and T waves are different from normal waves but the natural rhythm is not different. 4-Fibrillation: it is an irregular type of contraction without adequate blood pushing. a-atrial fibrillation:in ECG there is no P-wave but replaced by irregular fluctuation of potentials called f-waves. The pulse is irregular. It happen in chronic heart diseases. b-ventricular fibrillation(lead to loss of consciousness within a few seconds). There is irregular continous uncoordinated twitching of the ventricular muscle result in no output of blood, death will occur. It happen when the coronary blood supply to the myocardium is stoped (infraction) also occure in response to certain drugs and anesthesia. Cardic Output Is the volume of blood pumped by each ventricle per minute. Cardic output= Heart rate x Stroke volume C.O= HR x SV (beat/minute) (Liter/beat). Stoke volume:is the volume of blood ejected by each ventricle during each beat. E.g.: HR= 72, SV=70ml/beat. C.O.=72 x 0.07 = 5L/min (in resting adult). During exersice the C.O. may reach 30-35L/min. Factors control the C.O. 1-Control of HR A- Autonomic control 1-Carotid sinus reflex. Pressure in carotid sinus glossopharyngeal nerve(IX) cardio inhibitory center (medulla) vagus nerve(X) S-A discharge AV discharge HR C.O 11 2-Aortic reflex. Pressure in aortic (baroreceptors) medulla (cardiol inhibitory center) (parasympathetic) vagus S.A and AV HR C.O 3-Atrial reflex (Bainbridge reflex) Atrial pressure stimulate baroreceptors HR and force of contraction C.O B-Chemical 1-Epinephrin from adrnal medulla Sympathetic activity epinephrine S-A node and myocardium contraction HR and contraction C.O + + + + 2-K and Na K and Na HR and contractility C.O. ++ ++ 3- Ca Ca HR and contractility C.O. C-Temperature, emosions, sex, and age. 1-Temperature . Tempreture (fever, exercise) HR. and contractility C.O 2-Emosions Fear, angry, and anxiety sympathetic discharge HR C.O Depression stimulate cardioinhibitory center HR C.O 3- Sex and age In female HR is faster the male. At birt the HRis faster and will be decreased as the age is progressed. 2-Control of SV A-End-diastolic volume (DDV) 1-length of ventricular diastole Ventricular diastole ventricular filling vent.volum SV C.O 2-venous pressure Venous pressure venous return vent.filling SV CO B-End-systolic volume(ESV) 1-Arterial pressure Art.press. ESV SV C.O Art.press. ESV SV C.O SV=EDV-ESV ( ESV SV and vice versa). 2-Force of ventricular contraction a- sympathetic stimulation SA node and AV node ventricular muscle contraction SV C.O 12 b-changes in the degree of stretching of ventricular muscle secondary to changes in ventricular volume. This is the intrinsic factor relaxationship between end-diastolic pressure volume and stoke volume which called starling law of the heart which mean that the more distended ventricle responds with more forceful contraction. The mechanism for this is that cardic muscle like skeletal muscle increases its strength of contraction when it is stretched. C-circulating EP. And NE. also produce increase of myocardial force of contractiuon . D- chemoreceptors: is a receptors in the hypothalamus sensitive to decrease of O2 level and increase of CO2 level in the blood. This receptors will stimulate the cardioacceletory center in the medulla in response to O2 and CO2 to stimulate SA-node, A-V node and ventricular myocardium which will increase HR and force of contraction to increase SV which will increase cardiac output. CO2 and O2 St.cardioacceletory center HR and SV C.O Cardiovascular Physiology Function of cardiovascular system: 1-Transport and distribute essential substance to the tissues. 2-Remove by-product of metabolism. 3-Regulate body temperature. 4-Humoral communication throughout the body. 5-Adjustment of O2 and nutrient supply in different physiology states. The CVS consists of: 1-Pump(heart) pulmonary circulation , systemic circulation 2-Distributing and collecting tubes (arteries and veins). 3-Extensive system of thin vessels which permit rapid exchange between tissues and vasculas channels (capillaries). Hemodynamics The arterial blood flow is pulsatile in character (due to cardiac ejection) and become steady in the capillaries because of large surface area so the exchaenge of diffusible substance occure between blood and tissue. *The heart is an extremely complication pump. *The blood vessels are multibranched elastic tubes of varying diameters. 13 *The blood is not a simple fluid, it is a suspension of cells (RBCs,WBCs, platelets), lipid globules, proteins. Velocity of Blood Stream Vlocity The rate of displaceme with respect to time (cm/sec.) or (distance per unit time ) . Flow: volume per unit time (cm3/sec.) V=velocity Q= flow A=cross-sectional area Steady flow: is the absence of variation of flow in time (non pulsation flow). Laminar flow: is a gradient of flow rate between the stationary peripheral layer of fluid and the rapidly flowing central layers of fluide. Viscosity: is the friction exerted by the movement of laminae of blood relative to each other. Resistance: hydraulic resistance is the ratio of pressure drop to flow. The Vascular System 1-Blood flow: the amount of blood that passes through a blood vessel in a given time. Factors which control blood flow are: a- differences in pressure between the two ends of the tube. b- resistance of flow which means friction between tube wall and fluid and between the molecules of the fluid. So resistance depend on the nature (property) of the fluid (viscosity) and the geometry of the tube (length and radius). *The flow is directly proportional to the pressure difference and inversely proportional to the resistance. Fraction viscosity resistance flow Length flow (but it is constant in blood vessels). *radius is markedly determine the resistance while the length of blood vessels and viscosity of blood is constant. II=constant , r=radius , n= viscocity, L= length of tube 14 This formula is called poiseuiilles formula *The radius of blood vessel can be change significantly and constitute the most impotant factor in the control of resistance to blood flow. 2-Arterial Blood pressure. The contration of the ventricles ejects blood into the systemic and pulmonary arteries during systole. This will distends the arteries by raising arterial blood pressure. The systolic pressure: is the maximum pressure reachen during peak ventricular ejection. The diastolic pressure: is the minimal pressure occure just befor ventricular contraction. The blood pressure :is generally recorded as Systolic Diastolic Plus pressure: can be felt in an artery is due to the difference between systolic and diastolic pressure. Plus pressure= systolic pressure-diastolic pressure = 120-80=40mmHg. Factors which change pulse pressure are: 1- an increased stroke volume will systolic pressure. 2-decreased arterial distensibility (as in arteriosclerosis) will systolic pressure. The bood pressure is regulated by: 1-Cardic output (SV and HR) C.O BP. 2-Peripheral resistance R BP. 3-Blood viscosity B.vis. BP Polycythemia and plasma proteins viscosity. 1-Cardic output 2-Viscosity 3-Peripheral resistance which determined primarily by the caliber of the arterioles. The caliber of the arterioles under autonomic control by the control of the vasomotor center in the medulla. 15 Mean arterial pressure: Is the most important pressure because it is the average pressure driving blood into the tissues throughout the cardiac cycle. Mean arterial pressure is not the value half way between systolic and diastolic pressure because diastolic usually lasts longer than systole. Mean arterial pressure Hypertension : increased arterial blood pressure than normal. Hypotension: decreased arterial blood pressure than normal. Baroreceptors: are pressure or stretch receptors located in the carotid sinus and aortic arch. They respond to the changes in the arteries induced by changes in arterial blood pressure through either inhibition or stimulation of the vasomotor center in the medulla oblongata. Mareys Law: is the relationship between increased blood pressure and decreasd heart rate during regulation of blood pressure. Chemoreceptors : are receptors found in the vasomotor center that sensetive to CO2 and in the aortic are carotid bodies that sensitive to O2. Cerebral Circulation 16 R. external carotid artery supplies right side of thyroid gland , tongue, throat, face , ear , scalp and dura matar. R. internal carotid artery supplies brain , right eye, and right sides of forehead and nose. L. external and internal carotid arteries are similar to that of right . * Inside the cranium , anastomoses of left and right internal carotids along with basilar artery from a hexagonal arrangement of blood vessels at base of brain near sella turcica called cerebral arterial circle (circle of Willis). From this circle arise arteries supplying most of the brain . The function of the cerebral arterial circle are: 1-to equalize blood pressure to brain 2-provide alternate routes for blood to brain in case of arterial damage. Exchange of gases and material occur in the sinuses of the brain. Right and left internal jugular veins receive blood from face and neck. They arise as continuation of sigmoid sinuses at base of skull. Intracranial vascular sinuses are located between layers of duramater and receive blood from brain, Other sinuses that drain into internal jugular include superior sagital sinus, inferior sagital sinus, straight sinus and transverse (lateral) sinuses. Internal jugulars descend on either side of neck and join with subclavian veins in the same side to form right and left brachiocephalic veins. From here blood flows into superior vena cava. Right and left external jugulars. They drian blood from parotide (salivary) glands, facial muscle, scalp and other superficial structures into subclavian veins, then into brachiocephalic veins and then into superior vena cava. Fetal circulation : It is not necessary for the fetal heart to pump much blood through either the lungs or the liver because : 1-the lungs are nonfunctioning during fetal life. 2-the liver is only partially functional. There is a specific anatomic structure of fetal circulation: 1-Blood returning from the placenta through the umbilical vein passes through the ducts venosus by-passing the liver into inferior vena cava. 17 2-Then most of the blood (oxygenated) entering the right atrium from the inferior vena cava is directed in a straight pathway through the foramen ovale directly into the left atrium and then into the left ventricle. 3-Other blood (deoxygenated) entering the right atrium from superior vena cava is directed into the right ventricle then into pulmonary artery then into the descending aorta through the ducts arteriosus. 4-Blood is returned through the two umbilical arteries into the placenta thus the deoxygenated blood becomes oxygenated again. *At birth, when lungs, renal, digestive and liver functions are established, the followings changes occure: 1-The umbilical arteries vasoconstrict shut and atrophy to become the medial umbilical ligaments. 2-The umbilical vein vasoconstricts shut and become the round ligament of the liver. 3-The placenta is delivered by the mother as the after birth. 4-The ducts venosus vasoconstricts shut and becomes the ligamentum venosum (a fibrous cord in the liver). 5-the foramen ovale normally closes shortly after birth to become the fossa ovalis (a depression in the internal septum). 6-The ductus arterious closes by vasoconstriction and atrophies and become the ligamentum arteriosus. Pulmonary Circulation : Pulmonary circulation defined as the flow of deoxygenated blood from the ventricle to the air sacs of the lungs and the return of oxygenated blood from the air sacs of the lungs to the left atrium. Pulmonary trunk emerge from the right ventricle and passes upward, then divide into right and left pulmonary arteries to the right and left lungs respectively. On entering the lungs, these arteries divide and subdivide until they from capillaries around the alveoli (air sacs) in the lungs. CO2 is passed from the blood into the alveoli and O2 is passed from the alveoli into the blood. The capillaries unite, venules and veins are formed and eventually two pulmonary veins exit from each lung and transport the oxygenated blood to the left atrium. Blood flow through the lungs differs from systemic circulation in several ways: 18 1-The pulmonary arteries have lager diameter, thinner wall and less elastic tissue than their counterpart systemic arteries. As a result there is little resistance to blood flow. This means that less pressure is required to move blood through the lungs. 2-There is an autoregulation mechanism in response to levels of oxygen. In systemic circulation, blood vessels dilate in response to low oxygen concentration. In pulmonary circulation, blood vessels constricts in response to low oxygen concentration. This mechanism is very important in the distribution of blood in the lungs who it is needed most. 3-There is a different between pulmonary and systemic circulation relates to capillary hydrostatic pressure. In systemic, the capillary hydrostatic pressure=25 mmHg but in pulmonary, the capillary hydrostatic pressure= 15mmHg because the colloid osmotic pressure in the interstitial fluid of the lungs is high. This difference is to prevent pulmonary oedema. *Pulmonary oedema may develop from: a-increased capillary blood pressure due to increased left atrial pressure (e.g. in case of mitral valve stenosis). b-increased capillary permeability due to some bacterial toxin. *Pulmonary oedema lead to decrease diffusion rate of O2 and CO2 which lead to inhibits the exchange of gases in the lungs. Hepato-Portal Circulation: Define as the flow of venous blood from the gastrointestinal organs and spleen to the liver before returning to the heart. (which can be summarized as following: 19 Coronary Circulation: The left and right coronary arteries and their branches supply blood to the heart muscle. These arteries branch from the base of the ascending aorta as it leaves the heart. They traverse the anterior surface of the heart in the grooves and pass to the posterior surface, where their branches anastomose or join together. (This anastomoses is for maintaining a blood supply to the cells of the heart when a vessel becomes blocked). Numerous branches from the main arteries carry blood to the capillary networks among the muscle cells. After passing through the capillaries, blood enters the cardiac veins. Many of these veins unit to form a large vessel called the coronary sinus which carries blood into the right atrium. Other veins(from the wall of the right ventricle) return blood directly to the right ventricle. Sinusoids جيبانياااreturn blood from the myocardium directly into the cavities of the ventricles. Blood flow in heart muscle vessels only when the heart is relaxed (contraction compresses the vessels and prevents the flow). 20