* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The hypothalamo-pituitary-thyroid axis
Survey
Document related concepts
Hormone replacement therapy (male-to-female) wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Hypothalamus wikipedia , lookup
Pituitary apoplexy wikipedia , lookup
Hypopituitarism wikipedia , lookup
Transcript
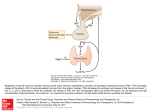
The hypothalamopituitary-thyroid axis Thyrotropin releasing hormone (TRH):- TRH is manufactured in the hypothalamus and transported via the portal circulation to the pituitary where it ultimately leads to exocytosis of TSH. TRH is a modified tripeptide synthesized as a 26kDa prohormone by peptidergic hypothalamic nuclei and transported, after activation, to the anterior pituitary by the portal circulation. Stimulates TSH synthesis and secretion by binding to receptors on the pituitary thyrotroph cell membranes that are linked to phospholipase C. More chronic actions of TRH include stimulation of TSH subunit biosynthesis and TSH glycosylation. Thyroid stimulating hormone:TSH (also known as Thyrotropin) is a 28kDa glycoprotein synthesized by the pituitary thyrotroph. It consists of two noncovalently linked subunits and contains about 15% carbohydrate. The α-chain is identical to that found in other pituitary glycoprotein hormones and so the specificity is determined by the βchain and the three dimensional configuration. The synthesis each subunit is directed by separate messenger R ribonucleic acids (mRNAs) encoded by separate genes on different chromosomes. The plasma half life of TSH is about 65 minutes. TSH acts on the thyroid gland and influences virtually every aspect of thyroid hormone biosynthesis and secretion:TSH acts via a specific membrane receptor on the target cell of the thyroid gland. The receptor is a 85kDa glycoprotein with an extracellular domain of approximately 400 amino acids, seven transmembrane domains of about 250 amino acids. The binding of TSH to the receptor activates adenylate cyclase. How the TSH control of thyroid metabolism:1- stimulation of iodide pump to increase ion trapping. 2- stimulate oxidation of iodide. 3- stimulate glucose metabolism by pentose shunt so increase production of NADPH which is a factor of production H2O2 & also deiodinase. 4- stimulate endocytosis to engulf & storage of thyroglobulin. Biosynthesis of T4 and T3 • The first step is transport of Iodide from blood to thyroid follicle. This process against gradient because the concentration of Iodide in thyroid gland 20 times more than blood, this process needs energy thus it is ATP driven, under control of TSH. It is linked to ATPasedependent Na/K pump. • Follicle of thyroid gland composed of single epi. Cell contain colloid inside lumen. The colloid contains thyroglobulin which is a glycoprotein M.w 660 kd, CHO account 8-10 of wt and iodide 0.2-1, it contain 115 tyrosine residues each of which is potential site of iodination. About 70 percentage of the iodide is thyroglobulin exist in the inactive precursors MonoIodotyrosine(MIT) and DiIodotyrosine(DIT) while 30 percentage as T3andT4 • The second step is the oxidation of iodide to iodine(active) by peroxidase in the presence of H2O2 this is called free radical reaction and occur in epi. Cell of follicle. This process inhibited by thiourea drugs. • The third step is iodination of tyrosine(tyrosyl residues in thyroglobulin) , probably involves thyroperoxidase. • In 3 position------------- MIT • I 3, 5 position------------ DIT . Both occur in luminal thyroglobulin • The 4th step • DIT+ DIT--------- T4 • DIT+ MIT--------- T3 both occur within thyroglobulin molecule. • T4 is quantitatively the most important thyroid hormone and it is produced exclusively by the thyroid gland . T3 is the biologically active form of thyroid hormone produced by 5- deiodination of T4. This process may occur in thyroid gland, in target tissues or in other peripheral tissues Removal of an iodine from the 5 rather than the 5- position result in reverse T3, which biologically inactive • The daily production rate of T4 is approximately 110 nmol (90μg) and transported in the plasma bound to a variety of specific and non specific binding proteins . • Approximately 80‰ of T4is converted into equal amounts of T3 and reverse T3(rT3), the remaining T4 is conjugated with sulfate or glucuronide and deactivated by deamination or decarboxylation . • The daily production rate of T3 is approximately 45 nmol (35μg) by extra thyroidal deiodination . The turnover of T3 is much greater than that of T4 , and the free form – is able to exert the biological activity while the bound form – is not able to exert the biological activity. • Transport of T3 and T4 1/2 – 2/3 OF T3 and T4 in the body is extrathyriodal and bound to 2 specific protein Thyroxin binding globulin (TBG) and Thyroxin binding pre albumin(TBPA). The TBG is glycoprotein , bind to T3,T4 with 100 times the affinity of TBPA. TBG is produced in the liver and it is synthesis increases by estrogen while it decreases by androgen and glucocorticoid and some liver diseases. • Biochemical action of thyroid hormone • • • • • By acting on a wide range of tissues : 1- They increase the basal metabolic rate 2- Increase ATP consumption 3- Increase O2 consumption Most, if not all, of these actions result from altered transcription brought about by the binding of T3 to its nuclear receptor. • Clinical disorders • Thyroid disease can occur at any time from birth to old age. Greater than 95 percentage of thyroid disease originates in the thyroid gland and much of this is autoimmune in origin