* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Enzymatic function of nitric oxide synthases
Survey
Document related concepts
NADH:ubiquinone oxidoreductase (H+-translocating) wikipedia , lookup
Protein domain wikipedia , lookup
Metalloprotein wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
P-type ATPase wikipedia , lookup
List of types of proteins wikipedia , lookup
Transcript
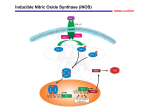
Cardiovascular Research 43 (1999) 521–531 www.elsevier.com / locate / cardiores www.elsevier.nl / locate / cardiores Review Enzymatic function of nitric oxide synthases Penelope J. Andrew, Bernd Mayer* ¨ Pharmakologie und Toxikologie, Karl-Franzens-Universitat ¨ Graz, Universitatsplatz ¨ 2, Graz A-8010, Austria Institut f ur Received 22 December 1998; accepted 25 February 1999 Abstract Nitric oxide (NO) is synthesised from L-arginine by the enzyme NO synthase (NOS). The complex reaction involves the transfer of electrons from NADPH, via the flavins FAD and FMN in the carboxy-terminal reductase domain, to the haem in the amino-terminal oxygenase domain, where the substrate L-arginine is oxidised to L-citrulline and NO. The haem is essential for dimerisation as well as NO production. The pteridine tetrahydrobiopterin (BH 4 ) is a key feature of NOS, affecting dimerisation and electron transfer, although its full role in catalysis remains to be determined. NOS can also catalyse superoxide anion production, depending on substrate and cofactor availability. There are three main isoforms of the enzyme, named neuronal NOS (nNOS), inducible NOS (iNOS), and endothelial NOS (eNOS), which differ in their dependence on Ca 21 , as well as in their expression and activities. These unique features give rise to the distinct subcellular localisations and mechanistic features which are responsible for the physiological and pathophysiological roles of each isoform. 1999 Elsevier Science B.V. All rights reserved. Keywords: Nitric oxide; Free radicals; Endothelial function; Endothelial factors; Vasoconstriction / dilation 1. Introduction Nitric oxide (NO), synthesised by the enzyme NO synthase (NOS), is a major factor in the cardiovascular system. Its multiple roles include regulation of vasomotor tone [1] and cell adhesion to the endothelium [2], and inhibition of platelet aggregation [3] and vascular smooth muscle cell proliferation [4]. At first glance, this list would appear to suggest that NO is a crucial factor in the prevention of cardiovascular damage such as that seen in atherosclerosis. Indeed, the loss of endothelial-derived NO arising from endothelial dysfunction is now thought to be a major cause of such pathological conditions. However, too much of a good thing should usually be avoided, and NO is no exception. Excess or inappropriate production of NO can be equally as deleterious as insufficient NO. Hence, immense research efforts are currently being made to understand the regulation, production, and functions of NO. This review will concentrate on what is currently known about the enzyme which synthesises NO. *Corresponding author. Tel.: 143-316-3805567; fax: 143-3163809890. E-mail address: [email protected] (B. Mayer) The complexity of NOS, with its distinct domains, its multitude of cofactors and prosthetic groups, and its unique reaction mechanism, has in recent years drawn the attention of a large number of biochemists and structural biologists. However, despite intense research efforts, several key features remain to be determined, most notably the structure of the intact enzyme. Other open questions include the complex role of the pterin cofactor tetrahydrobiopterin (BH 4 ), the nature of the NOS products in vivo, and the mechanistic reasons for the subtle differences between the three isoforms. Recent progress that has been made towards these goals will be discussed. 2. Overview of the NO synthase family NOS (EC 1.14.13.39) catalyses NO biosynthesis via a reaction involving the conversion of L-arginine to L-citrulline [5]. The enzyme functions as a dimer consisting of two identical monomers, which can be functionally (and structurally) divided into two major domains: a C-terminal reductase domain, and an N-terminal oxygenase domain Time for primary review 31 days. 0008-6363 / 99 / $ – see front matter 1999 Elsevier Science B.V. All rights reserved. PII: S0008-6363( 99 )00115-7 522 P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 Fig. 1. Scheme of the domain structure of the NOS dimer, showing cofactor and substrate binding sites. Fig. 2. The NOS-catalysed reaction. (Fig. 1) [6]. The former contains binding sites for one molecule each of NADPH, FAD, and FMN, in close homology with cytochrome P-450 reductase, whereas the latter binds haem and BH 4 , as well as the substrate L-arginine. Between these two regions lies the calmodulin (CaM) binding domain, which plays a key role in both the structure and function of the enzyme. There are three distinct isoforms of NOS which differ both in their structure and function [7]. Endothelial NOS (eNOS or NOS III, 23134 kDa) and neuronal NOS (nNOS or NOS I, 23160 kDa) are generally referred to as constitutively expressed, Ca 21 -dependent enzymes, although eNOS can also be activated in a Ca 21 -independent manner (discussed in Section 8.1) [8]. Inducible NOS (iNOS or NOS II, 23130 kDa) is expressed at high levels only after induction by cytokines or other inflammatory agents, and its activity is independent of an increase in Ca 21 . The three NOS isoforms are characterised by regions of high homology, namely the oxygenase and reductase domains, but at the same time each isoform exhibits distinctive features which reflect their specific in vivo functions. Although the molecular biology of these isoforms is discussed at length in another article in this issue, the main structural differences between the three enzymes will be referred to briefly in a later section of this article, since they have a major impact on the enzymatic function of each isoform. 3. The NOS-catalysed reaction Biosynthesis of NO involves a two step oxidation of to L-citrulline, with concomitant production of NO (Fig. 2). The reaction consumes 1.5 mol of NADPH, and 2 mol of oxygen per mol of L-citrulline formed. The proposed mechanisms are discussed at length by Griffith and Stuehr and others [9–11], and involve an initial hydroxylation of L-arginine, leading to the formation of N G -hydroxy-L-arginine, which can also act as a substrate for NOS. This is followed by oxidation of the intermediate, using a single electron from NADPH [12], to form Lcitrulline and NO. Although this scheme represents the reaction assumed to be catalysed by NOS, the enzyme is also capable of catalysing the production of additional products, notably superoxide anion (O ?2 2 ), depending on L-arginine the conditions [13–15]. The nature of the in vivo products of NOS is still under debate and is discussed in Section 7, as well as elsewhere in this issue. 4. The reductase and oxygenase domains The isolated reductase domain is able to transfer electrons from NADPH via the flavins FAD and FMN to cytochrome c, while the oxygenase domain dimer can convert the reaction intermediate N G -hydroxy-L-arginine to NO and L-citrulline [16–18]. Hence, the two domains perform catalytically distinct functions. While the reductase domain itself is highly homologous to enzymes such as the NADPH:cytochrome P450 reductase, its dependence on the CaM-binding domain for efficient electron transfer is unique [19]. The cofactor binding sites have been well-defined as a result of the close homology with related reductases as well as evidence obtained from mutagenesis studies [20–22]. In contrast, the binding sites for L-arginine, haem, and BH 4 in the oxygenase domain are less well characterised, although several residues have been identified which are important for BH 4 binding (C99 in eNOS [23], G450 and A453 in iNOS [24]). A polypeptide of this region (558–721 in rat nNOS) which shows similarity to the pterin-binding domain of dihydrofolate reductase and to a region in aromatic amino acid hydroxylases [24], was however unable to bind BH 4 , but could bind N G -nitro-L-arginine [25]. Two residues important for L-arginine binding have been identified in this region: E371 and D376 in iNOS [26], and the analogous E361 in eNOS [27]. Several other acidic residues which affect L-arginine and BH 4 binding were also identified in this region [26]. The loss of L-arginine binding by the E371 mutant was put to good use in a study of electron transfer in heterodimers consisting of a full length subunit and an oxygenase domain [28]. NO was synthesised when the oxygenase domain containing the mutation was in the same subunit as the reductase but not if it was in the opposite oxygenase domain, indicating that electrons are transferred from the reductase domain flavins on one subunit to the oxygenase domain haem on the second subunit. P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 The recently solved crystal structure of a dimeric iNOS oxygenase truncation mutant (residues 66–498) revealed a structure which is unusual for haem-binding proteins in that it contains a large amount of b-sheet [29]. The authors describe the structure in analogy with a baseball glove, with the haem cradled between the proximal ‘thumb’ and the distal ‘palm’. BH 4 binds on the proximal side, while L-arginine is located on the distal side. Another notable feature of the oxygenase domain dimer, revealed in the recent crystal structure of the eNOS haem domain [30], is the presence of a zinc atom which is tetrahedrally coordinated to two pairs of Cys residues. The metal may be important in determining the stereospecificity of the BH 4 binding site. The reductase and oxygenase domains of NOS are therefore distinct catalytic units, which together provide the complete machinery required for NO production. This raises the question as to why the functional enzyme is a dimer rather than a monomer. The mutation experiments described above, showing that electrons are transferred from one subunit to another rather than within one subunit, provide a hint to this puzzle. The next section describes the factors important in the dimerisation process which leads to the fully functional enzyme. 5. The NO synthase dimer An essential feature of NOS is that, despite the ability of the reductase and oxygenase domains to function independently under certain circumstances, NO synthase activity is carried out by the homodimer. Although the mechanistic reasons have not yet been resolved in detail, a significant amount is already known about the factors which govern dimerisation. 5.1. Role of haem The haem plays an essential role in dimerisation (Fig. 3). In its absence, NOS exists as monomers which are essentially normal with respect to secondary structure. Furthermore, the ability to catalyse the NADPH-dependent reduction of cytochrome c is retained in nNOS monomers, indicating that the transfer of electrons within the reductase domain from NADPH via the two flavins is not dependent on the dimeric structure [31]. Monomers of all the isoforms are, however, unable to bind BH 4 or a substrate analogue and do not catalyse L-citrulline / NO production [31–33]. Haem is the sole cofactor for which there is an absolute requirement for the formation of active nNOS dimers [31], and it is also the key factor in eNOS dimerisation [33]. Although the characteristics differ from those of the two constitutive isoforms, the haem plays a similarly essential role in iNOS dimerisation [32]. Resolution of the crystal structure confirmed that the haem is bound via a proximal cysteine thiolate ligand [29], 523 Fig. 3. Stages of NOS dimer assembly. Haem-free monomers (a) associate in the presence of haem to form a dimer with NADPH oxidase activity (b). Low levels of BH 4 lead to the formation of a stable dimer (indicated by the black bar) which catalyses simultaneous production of NO and O ?2 (c). At high BH 4 levels, the enzyme acts purely as an NO 2 synthase (d). the identity of which is known for all three isoforms [34–36]. The formation of this bond has been suggested to be a key step in the process of dimerisation [37]. Evidence obtained from studying the fluorescence dynamics of nNOS-bound flavins suggests that the haem is also essential in the interaction between the reductase and oxygenase domains [38], which form an interface in the quaternary structure. The coordination state of the haem can be unequivocally identified through examination of the absorption spectrum. This depends upon the energetical ‘spin state’ of the unpaired electrons of the haem iron, which in turn is related to the geometry of the haem ligands. When these electrons are in the low-spin state, reflecting a six-coordinate haem, the maximum is observed at 394–397 nm. This form of NOS is inactive. Upon binding L-arginine and its analogues, as well as BH 4 [39–47], the maximum shifts to 418 nm, indicative of a high-spin five-coordinate haem, which is necessary for NOS activity. 5.2. Role of BH4 The haem requirement for dimerisation is common to all three NOS isoforms. They do however differ with respect to the role of BH 4 in dimerisation. Whereas nNOS and eNOS can form dimers in the absence of BH 4 [48], iNOS dimerisation was reported to require the presence of the 524 P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 pteridine [32], although dimers were formed in E. coli in the absence of BH 4 [49]. Furthermore, BH 4 stabilises the nNOS and eNOS dimers once formed, and also the iNOS dimer, although not to the same extent [33,48,50,51]. These data are supported by the reduced binding of BH 4 by an N-terminal deletion mutant of iNOS, demonstrating the importance of residues 66–114 in iNOS for binding of the cofactor and hence dimerisation [52]. The recent crystallographic data also show the location of BH 4 at the dimer interface [29]. Although these observations have had an impact on in vitro synthesis and reconstitution experiments, the functional implications remain uncertain. The close resemblance of 4-amino-BH 4 , a novel pterin-based inhibitor of NOS [51,53], to BH 4 in terms of conformational changes induced (low-spin to high-spin conversion of the haem, dimer stabilisation, increased affinity for L-arginine) despite the inability to support NO production suggests a more complex role for BH 4 than merely inducing conformational changes [51,54]. The close proximity of BH 4 to the haem, as well as to the flavins at the domain–domain interface [38], hints at a possible role in electron transfer [55], although exogenously added BH 4 does not appear to provide electrons for the reaction [56]. In this respect, the role of BH 4 in NOS differs from that in aromatic amino acid hydroxylation [57]. A thorough analysis of the interaction of numerous pterins with iNOS revealed that the steps up to and including haem reduction are supported by dihydropterins as well as tetrahydropterins [58]. However, only the latter are able to support NO synthesis and NADPH oxidation. The role of BH 4 in electron transfer therefore remains to be settled, although it has been shown that the cofactor accelerates the decay of the ferrous–dioxy complex of nNOS, providing a novel hint to its role in NO synthesis [59]. Despite these clues, the full role of BH 4 in NOS catalysis remains to be elucidated. 5.3. Role of L-arginine Binding of L-arginine to iNOS facilitates dimerisation [32]. Various arginine analogues as well as compounds containing the guanidinium moiety are also able to facilitate iNOS dimerisation [44]. Despite the inability to support NO synthesis, these compounds also alter the heme spin state, indicating a change in the haem geometry to the five-coordinate conformation, and increase the rate of NADPH oxidation, showing that occupation of the guanidinium-binding site in the enzyme alters electron flow. The extensive interactions of L-arginine, as revealed by the crystal structure [29], with hydrophilic side chains of the alpha helix involved in dimer formation, as well as with the haem propionate which hydrogen bonds to BH 4 , provide the structural reasons for the stabilising effect on the dimer. In summary, the key to dimerisation of NOS lies in the haem prosthetic group, although BH 4 and L-arginine are also important factors, with their relative contribution differing depending on the isoform in question. As a result of their stabilising interactions, these molecules endow the NOS dimer with an exceptionally stable quaternary structure. 6. Calcium dependence and the role of calmodulin Dependence on Ca 21 is a key distinguishing feature between the constitutive and inducible isoforms. eNOS and nNOS are both activated by an elevation in intracellular Ca 21 , followed by the subsequent binding of Ca 21 / CaM. In contrast, iNOS contains irreversibly bound CaM, and is hence largely independent of Ca 21 , although a 2-fold greater activity is observed in the presence of 2.5 mM Ca 21 compared to that in 10 mM EGTA [60]. The molecular reasons for this fundamental difference have been investigated by swapping the respective CaM-binding regions [60]. The iNOS CaM-binding peptide enabled eNOS to bind CaM but did not confer Ca 21 -independence. Hence, only the Ca 21 -bound conformation of CaM can activate the enzyme. This dependence on Ca 21 may be ultimately due to the presence of an autoinhibitory sequence which is present in the FMN-binding region of the two Ca 21 -dependent isoforms but is not found in iNOS [61]. The CaM-binding region in eNOS is directly involved in membrane association, specifically to anionic phospholipids such as phosphoserine, and this association prevents the binding of CaM to eNOS and hence catalytic activity [62]. CaM binds to both the isolated reductase domain of nNOS as well as to the full-length enzyme, and stimulates the rate of electron transfer within the reductase domain [19]. CaM is furthermore essential for the transdomain transfer of electrons to the haem [63]. Despite this knowledge, the exact mechanism by which CaM induces these changes is not understood. 7. Products of the reactions catalysed by NO synthase nNOS is capable of producing not only NO, but also O ?2 2 , and peroxynitrite (Fig. 3). This unusual property is a consequence of the dimeric nature of the enzyme, in which the two subunits are able to function independently [64]. In fact, the purified nNOS dimer normally consists of one BH 4 -containing subunit and one BH 4 -free subunit, due to the large difference in binding affinity between the first and second BH 4 -binding sites [47]. This negative cooperativity of BH 4 binding means that only one subunit will have BH 4 bound over a wide range of BH 4 concentrations (up to 1 mM). This has important implications for the outcome of the catalytic reaction, since only at very high BH 4 concentrations will NOS function purely as an P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 NO synthase (Fig. 3d). Although the following discussion concerning NOS products largely refers to nNOS, recent observations (see below) suggest that both eNOS and iNOS are also capable of catalysing the production of O 2?2 , suggesting that this mechanism may be more widespread than originally thought. 7.1. The uncoupled reaction In the presence of low concentrations or the absence of nNOS catalyses the uncoupled reduction of oxygen, leading to the production of O ?2 2 and H 2 O 2 (Fig. 3b) [13,14]. Although O 2?2 itself, as well as its metabolic products, can trigger a variety of signal transduction processes leading to pathogenic conditions [65], the detrimental effects of O ?2 on endothelial function, vascular 2 smooth muscle cell proliferation, and leukocyte adhesion, which are evident in vascular pathologies are likely to be mediated by the scavenging of NO. Evidence for the damaging role played by O ?2 2 is provided by the protective effect of superoxide dismutase (SOD) delivery in a rat model of angiotensin II-induced hypertension [66] as well as in cholesterol-fed rabbits [67,68]. The only major difference between the NOS isoforms in terms of the reactions performed lies in the rate of this NADPH oxidation, termed the uncoupled reaction. Under these conditions, nNOS continues to transfer electrons to the haem and hence oxidise NADPH at a high rate, whereas in eNOS and iNOS, this reaction occurs at a much slower rate [33,40,63]. A mechanistic explanation for this difference is provided by a study examining the reduction potential of the haem [69]. The haem iron in nNOS has a significantly higher reduction potential than that in iNOS, which must first bind substrate and BH 4 in order to achieve a similar value. Hence, the haem iron of nNOS but not of iNOS is readily reduced in the absence of L-arginine and BH 4 . The protective effect of manganese SOD in NO-mediated NMDA toxicity in cortical neurons [70] indicates that the uncoupled reaction catalysed by nNOS is pathologically relevant. The much lower rate at which this reaction is catalysed by iNOS, which is often present in situations where L-arginine is limited, for example in wounds [71], has been suggested to constitute a substratecontrolled safety mechanism to minimise O ?2 production 2 under such conditions [63]. However, recent data has shown that iNOS is in fact capable of catalysing substantial O ?2 production [72]. This occurs via a different 2 mechanism to that in nNOS, in that production is catalysed by the reductase domain and is only inhibitable by very high concentrations of L-arginine. A similar control mechanism for eNOS has been proposed, since the production of O ?2 would be highly detrimental in the vasculature [40]. 2 However, increased O ?2 production by eNOS has been 2 described in the context of the endothelial dysfunction seen in spontaneously hypertensive rats [73] and native LDL- 525 treated endothelial cells [74]. The reason for this alteration in eNOS activity leading to an increase in O ?2 2 production may be related to a decrease in BH 4 levels since two recent studies show that O 2?2 production by eNOS is inhibited by BH 4 but not L-arginine [75,76]. However, whereas L-arginine inhibits O 2?2 production by preventing uncoupled NADPH oxidation, BH 4 appears to act by directly scavenging superoxide [76]. The reasons for these isoform-specific differences in the regulation of O ?2 2 production are not clear. L-arginine, 7.2. A peroxynitrite synthase? Saturating L-arginine concentrations and the presence of sub-saturating levels of BH 4 lead to the simultaneous production of NO and O ?2 2 , by the BH 4 -containing and the BH 4 -free subunits respectively (Fig. 3c). Although these two products can react together extremely rapidly to form the potent oxidant peroxynitrite [77], the physiological outcome probably depends on the levels of GSH and SOD [78]. In the absence of these two molecules, peroxynitrite is formed. Free NO, which appears to feedback inhibit nNOS [79] by forming a ferrous–nitrosyl complex [80], is not detectable unless high concentrations of SOD are present [81]. However, very low levels of SOD are sufficient to allow enough NO to be formed to activate soluble guanylate cyclase, although the NO levels are below the limits of detection. In the presence of GSH and SOD, NO / O ?2 2 reacts preferentially with the thiol to form the thionitrite GSNO, which is likely to act as a storage or transport form of NO [82,83]. Subsequent release of NO can be mediated by both enzymatic and non-enzymatic mechanisms, although the actual physiological route has not yet been clarified. The formation of peroxynitrite from NO and O ?2 has 2 been implicated in the pathology of a large number of conditions involving oxidative stress such as atherosclerosis [84], using the presence of the marker nitrotyrosine as evidence. However, the true identity of the molecule responsible for the tyrosine nitration has recently been put into question, with the demonstration that peroxynitrite formed from the simultaneous production of NO and O ?2 2 at physiological pH is unable to efficiently nitrate tyrosine [85]. NO 22 has been proposed as a possible alternative, with the demonstration that, in human polymorphonuclear neutrophils, NO 2 2 is converted by myeloperoxidase into the nitrating and chlorinating species NO 2 Cl and NO 2 [86]. Therefore NOS can, in vitro, act as a peroxynitrite synthase. However, the name is unlikely to be applicable in vivo, given the ubiquitous presence of GSH and / or SOD, which will react with the NOS products, thereby preventing the formation of peroxynitrite. The ability to catalyse the production of O ?2 is not, as was previously 2 thought, limited to nNOS, and may in fact be pathologically highly relevant. 526 P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 8. Unique features of the NO synthase isoforms 8.1. eNOS The main source of endothelial NO, a crucial factor for the normal functioning of the cardiovascular system, is eNOS expressed by endothelial cells [87,88]. Other cellular sources relevant to the cardiovascular system include cardiac myocytes [89] and cardiac conduction tissue [90]. The particular properties of eNOS which enable it to perform its specialised functions include Ca 21 sensitivity, and the posttranslational modifications which mediate subcellular localisation. These enable the enzyme to respond not only to a variety of neurohormonal agents, but also to haemodynamic forces. In these respects, eNOS differs significantly from the other isoforms, and this section describes the molecular properties of the enzyme which account for these specialised features. Although eNOS was often referred to earlier as constitutive NOS, a number of factors as diverse as hypoxia [91], estrogen [92] and exercise [93] are now known to alter its expression. Since endothelial control of vascular tone is a sensitive and highly tuned process, these changes are likely to be immensely important to cardiovascular function, particularly in pathophysiological situations. eNOS is active, albeit sub-maximally, at the concentration of Ca 21 found in resting endothelial cells (around 100 nM) [40], explaining the vasoconstricting effect of a NOS inhibitor on basal blood flow [94]. The enzyme is generally fully activated by an increase in intracellular Ca 21 , resulting either from an influx of extracellular Ca 21 , or from release from intracellular stores. However, in a study using stretched segments of artery [8], shear stress-induced NO production, which was dependent on tyrosine phosphorylation, was independent of extracellular Ca 21 . The mechanism behind this observation was suggested to be a change in the microenvironment of the protein, perhaps involving pH changes. The activation of eNOS can be induced by hormones such as catecholamines and vasopressin, autacoids such as bradykinin and histamine, and platelet-derived mediators such as serotonin and ADP, via receptor-mediated activation of G proteins [95]. The activation of eNOS by mechanical forces including shear stress [96] and cyclic strain [97] is also mediated through G protein activation [98]. The subcellular targeting of eNOS plays a crucial role in this receptor-mediated mechanism of activation, by localising the enzyme in the proximity of the signaling molecules which mediate its activation [99]. This localisation to the plasmalemmal caveolae is regulated by the postranslational modifications at the N-terminal myristoylation and palmitoylation sites which are unique to the endothelial isoform of NOS (see accompanying article by Papapetropoulos et al., pp. 509–520, this issue). The distinctive lipid content of the caveolae is important to their function, and, in light of the observation that NOS activity is negatively modified by anionic phospholipids [62], it is conceivable that in conditions such as hypercholesterolemia, the disruption in eNOS activity may be caused by alterations in the lipid surroundings. The association of eNOS with the resident coat protein of caveolae (caveolin-1 and caveolin-3 in endothelial cells and myocytes respectively) is mediated by the scaffolding domain in caveolin, and leads to inhibition of eNOS activity [100], apparently via functional interference with CaM binding and electron transfer [101]. A similar inhibitory association has recently been observed between eNOS and the bradykinin B2 receptor [102]. Interestingly, a putative consensus sequence for mediating the interaction with caveolin is present not only in eNOS (350–358 in bovine eNOS) but also in the other two NOS isoforms [103]. This sequence lies in the putative oxygenase / reductase interaction surface suggested by the crystal structure [29], supporting the proposed role of interference with electron transfer. It is the disruption of this acylationindependent eNOS-caveolin complex and not as earlier studies suggested depalmitoylation [104] which leads to the agonist-induced activation of eNOS [105]. 8.2. nNOS In addition to the well-studied role of NO in the process of penile erection [106], non-adrenergic non-cholinergic relaxation occurs in all vascular smooth cells, as a result of the widespread expression of nNOS in peripheral neurons [107]. The regulation of nNOS activity is unique, with the subcellular localisation of the enzyme being mediated by a completely different mechanism to the fatty acylationmediated membrane association of eNOS. nNOS is the largest of the three isoforms due to the addition of a 300 amino acid stretch at the N-terminus. This region contains a PDZ domain (named after three of the proteins in which it was first described [108], also called a discs-large homologous region (DHR) or GLGF amino acid repeat), which is an approximately 90-residue long protein-recognition module responsible for the association of nNOS with other proteins containing this motif, including dystrophin at the sarcolemmal membrane [109] and PSD-95, a channel-associated protein in the brain [110]. The Tyr77 residue in the nNOS PDZ domain mediates selective binding to an Asp-X-Val consensus, which differs from the (Thr / Ser)-X-Val consensus favoured by PSD-95, and is present in glutamate and melatonin receptors [111]. Like eNOS, nNOS is also inhibited by the association with caveolin [100]. This inhibitory interaction with caveolin-3 in skeletal muscle can be mediated by two separate caveolin domains [112]. In terms of the enzymatic function of nNOS, it appears to differ from the other NOS isoforms by its readiness to catalyse the uncoupled oxidation of NADPH. Progress is being made in understanding the mechanism of this reaction (see Section 7). Although this reaction may help P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 to explain the damaging role of nNOS in ischaemia in the brain [113], the significance for nNOS-expressing cells outside the brain is not yet clear. 8.3. iNOS The effects of iNOS in vivo are a result of its unique features of Ca 21 -independence and inducible, high level expression. Under normal physiological conditions, iNOS is unlikely to have much impact on the cardiovascular system because of its low or absent expression, a conclusion which is supported by the lack of phenotype of uninfected iNOS knockout mice [114]. However, iNOS expression can be induced by inflammatory mediators in most types of vascular cells, including endothelial cells [115], cardiac myocytes [116], and smooth muscle cells [117], as well as macrophages [118], which, as a result of the high NO output, can have potentially damaging consequences. The expression of iNOS by macrophages and smooth muscle cells in atherosclerotic lesions has been taken as evidence for its detrimental role in atherosclerosis [118]. Furthermore, iNOS expression is responsible for the impairment in eNOS-derived NO production in vessels treated with inflammatory mediators [119]. However, iNOS expression may in some cases be protective, as shown by the iNOS-mediated suppression of allograft arteriosclerosis, via the prevention of intimal hyperplasia [120]. In contrast to the two constitutive isoforms, iNOS contains neither of the specific membrane-targeting sequences. Despite this, it has been found to be membraneassociated in human neutrophils [121] and mouse macrophages [122,123]. However, the proportion of membranebound enzyme varies between cell type and species, with less than half of mouse macrophage iNOS being membrane-associated. The functional relevance of this association is not known. The three distinct isoforms of NOS therefore show contrasting functions as a result of their sequence differences. Some of these lead to obvious structural changes, such as the fatty acylation of eNOS, whereas others are more subtle, for example the tendency to uncouple NADPH oxidation. Understanding these differences will enable us to exploit the unique features of each isoform, permitting selective stimulation or inhibition as required. 9. Control of NO synthase activity via substrate / cofactor regulation Although an in depth discussion on the topic is outside the scope of this article, the regulation of cofactor availability in determining NOS activity deserves a mention here. Apparent paradoxes of decreased protein expression in the face of increased NO production, as seen in LDLtreated endothelial cells [124], illustrate the necessity of understanding the global regulation of NOS activity. The 527 availability of substrate, particularly in the case of iNOS, can be regulated by changes in L-arginine uptake [125], or in the activities of argininosuccinate synthetase [126] or arginase [127]. BH 4 availability is controlled largely by GTP cyclohydrolase [128]. Regarding substrate levels, the fact that both the concentration of L-arginine in blood and the intracellular L-arginine concentration [129,130] are far greater than the Km of NOS for L-arginine [131] would seem to suggest that substrate availability should never be a limiting factor under normal conditions. However, several studies have shown that supplementation with Larginine can have beneficial effects, e.g. it reversed the increased adhesiveness of monocytes in hypercholesterolemic humans [132]. One possible mechanism by which L-arginine mediates these effects may be to outcompete the effects of the endogenous inhibitor, asymmetrical dimethylarginine, which is increased in hypercholesterolemia [133]. Since high doses of arginine can have additional effects which are unrelated to NO synthesis such as increasing the release of insulin [134,135], it is important to show that the effects of arginine are stereospecific in order to claim that increased NOS activity is mediating the observed changes. Alterations in the pathways governing substrate and cofactor availability can have a significant impact on the outcome of NOS activity. Understanding these regulatory mechanisms will provide insights into both the physiological regulation of NOS activity as well as the reasons behind the many pathophysiological states in which alterations in NO production are postulated to play a role. 10. Conclusion The complexity of NO biosynthesis is largely attributable to the multi-featured nature of the enzyme itself. Although much progress has recently been made into elucidating the biochemistry of this dimeric, multidomain molecule, it will be clear from this review that the mystery is far from solved. Outstanding questions which have been discussed here include the role of BH 4 and the nature of the NOS products in vivo. Despite the hints provided by the crystal structure and substances like 4-amino-BH 4 , the precise function of the cofactor is still a matter of debate. The continuing development of various BH 4 analogues should in the near future enable us to at last understand the full role of this cofactor in NOS function. In contrast, with recent publications demonstrating the ability of eNOS and iNOS, as well as nNOS, to produce O ?2 [72,75,76], it 2 appears that the struggle to clarify the nature of the actual products of NOS is far from over. Similarly, despite growing evidence concerning the structural differences which give the NOS isoforms their distinct functions, the aim of exploiting these differences in order to selectively modify NOS activity in an isoform-specific manner remains a target for the future. 528 P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 Acknowledgements Work in the authors’ laboratory was supported by grants ¨ from the Osterreichischen Nationalbank (Project No. 6655) ¨ and from the Fonds zur Forderung der Wissenschaftlichen ¨ Forschung in Osterreich (Projects No. P11478, P13013 and P11449). [19] [20] [21] [22] References [1] Palmer RMJ, Ferige AG, Moncada S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 1987;327:524–526. [2] Kubes P, Suzuki M, Granger DN. Nitric oxide: an endogenous modulator of leukocyte adhesion. Proc Natl Acad Sci USA 1991;88:4651–4655. [3] Radomski MW, Palmer RMJ, Moncada S. Modulation of platelet aggregation by an L-arginine-nitric oxide pathway. Trends Pharmacol Sci 1991;12:87–88. [4] Scott-Burden T, Vanhoutte PM. The endothelium as a regulator of vascular smooth muscle proliferation. Circulation 1993;87(Suppl V):V51–V55. [5] Mayer B, Hemmens B. Biosynthesis and action of nitric oxide in mammalian cells. Trends Biochem Sci 1997;22:477–481. [6] Hemmens B, Mayer B. Enzymology of nitric oxide synthases. In: Titheradge M, editor, Methods in molecular biology. Nitric oxide protocols, 1st ed, Totowa, NJ: Humana Press, 1998, pp. 1–32. [7] Stuehr DJ. Structure-function aspects in the nitric oxide synthases. Annu Rev Pharmacol Toxicol 1997;37:339–359. [8] Ayajiki K, Kindermann M, Hecker M, Fleming I, Busse R. Intracellular pH and tyrosine phosphorylation but not calcium determine shear stress-induced nitric oxide production in native endothelial cells. Circ Res 1996;78:750–758. [9] Griffith OW, Stuehr DJ. Nitric oxide synthases: Properties and catalytic mechanism. Annu Rev Physiol 1995;57:707–736. [10] Korth H-G, Sustmann R, Thater C, Butler AR, Ingold KU. On the mechanism of the nitric oxide synthase-catalyzed conversion of Nv-hydroxy-L-arginine to citrulline and nitric oxide. J Biol Chem 1994;269:17776–17779. [11] Marletta MA. Nitric oxide synthase structure and mechanism. J Biol Chem 1993;268:12231–12234. [12] Abu-Soud HM, Presta A, Mayer B, Stuehr DJ. Analysis of neuronal NO synthase under single-turnover conditions: conversion of Nvhydroxyarginine to nitric oxide and citrulline. Biochemistry 1997;36:10811–10816. [13] Mayer B, John M, Heinzel B et al. Brain nitric oxide synthase is a biopterin- and flavin-containing multi-functional oxido-reductase. FEBS Lett 1991;288:187–191. ¨ [14] Heinzel B, John M, Klatt P, Bohme E, Mayer B. Ca 21 / calmodulindependent formation of hydrogen peroxide by brain nitric oxide synthase. Biochem J 1992;281:627–630. [15] Huk I, Nanobashvili J, Neumayer C et al. L-arginine treatment alters the kinetics of nitric oxide and superoxide release and reduces ischemia / reperfusion injury in skeletal muscle. Circulation 1997;96:667–675. [16] Stuehr DJ, Kwon NS, Nathan CF et al. Nv-Hydroxy-L-arginine is an intermediate in the biosynthesis of nitric oxide from L-Arginine. J Biol Chem 1991;266:6259–6263. [17] Ghosh DK, Stuehr DJ. Macrophage NO synthase: Characterization of isolated oxygenase and reductase domains reveals a head-to-head subunit interaction. Biochemistry 1995;34:801–807. [18] Klatt P, Schmidt K, Uray G, Mayer B. Multiple catalytic functions of brain nitric oxide synthase. Biochemical characterization, cofact- [23] [24] [25] [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36] or-requirement and role of N G -hydroxy-L-arginine as an intermediate. J Biol Chem 1993;268:14781–14787. Abu-Soud HM, Yoho LL, Stuehr DJ. Calmodulin controls neuronal nitric-oxide synthase by a dual mechanism: Activation of intra- and interdomain electron transfer. J Biol Chem 1994;269:32047–32050. Bredt DS, Hwang PM, Glatt CE et al. Cloned and expressed nitric oxide synthase structurally resembles cytochrome P450 reductase. Nature 1991;351:714–718. Xie Q, Cho H, Kashiwabara Y et al. Carboxyl terminus of inducible nitric oxide synthase: Contribution to NADPH binding and enzymatic activity. J Biol Chem 1994;269:28500–28505. Zhang JL, Patel JM, Li YD, Block ER. Reductase domain cysteines 1048 and 1114 are critical for catalytic activity of human endothelial cell nitric oxide synthase as probed by site-directed mutagenesis. Biochem Biophys Res Commun 1996;226:293–300. Chen P-F, Tsai A-L, Wu KK. Cysteine 99 of endothelial nitric oxide synthase (NOS-III) is critical for tetrahydrobiopterin-dependent NOS-III stability and activity. Biochem Biophys Res Commun 1995;215:1119–1129. Cho HJ, Martin E, Xie QW, Sassa S, Nathan C. Inducible nitric oxide synthase: Identification of amino acid residues essential for dimerization and binding of tetrahydrobiopterin. Proc Natl Acad Sci USA 1995;92:11514–11518. Nishimura J, Martasek P, McMillan K et al. Modular structure of neuronal nitric oxide synthase: Localization of the arginine binding site and modulation by pterin. Biochem Biophys Res Commun 1995;210:288–294. Gachhui R, Ghosh DK, Wu C et al. Mutagenesis of acidic residues in the oxygenase domain of inducible nitric-oxide synthase identifies a glutamate involved in arginine binding. Biochemistry 1997;36:5097–5103. Chen P-F, Tsai AL, Berka V, Wu KK. Mutation of Glu-361 in human endothelial nitric-oxide synthase selectively abolishes L-arginine binding without perturbing the behavior of heme and other redox centers. J Biol Chem 1997;272:6114–6118. Siddhanta U, Presta A, Fan B et al. Domain swapping in inducible nitric-oxide synthase. Electron transfer occurs between flavin and heme groups located on adjacent subunits in the dimer. J Biol Chem 1998;273:18950–18958. Crane BR, Arvai AS, Ghosh DK et al. Structure of nitric oxide synthase oxygenase dimer with pterin and substrate. Science 1998;279:2121–2126. ´ Raman CS, Li H, Martasek P et al. Crystal structure of constitutive endothelial nitric oxide synthase: a paradigm for pterin function involving a novel metal center. Cell 1998;95:939–950. Klatt P, Pfeiffer S, List BM et al. Characterisation of heme-deficient neuronal nitric oxide synthase reveals a role for heme in subunit dimerisation and binding of the amino acid substrate and tetrahydrobiopterin. J Biol Chem 1996;271:7336–7342. Baek KJ, Thiel BA, Lucas S, Stuehr DJ. Macrophage nitric oxide synthase subunits: Purification, characterisation, and role of prosthetic groups and substrate in regulating their association into a dimeric enzyme. J Biol Chem 1993;268:21120–21129. ¨ ¨ List BM, Klosch B, Volker C et al. Characterization of bovine endothelial nitric oxide synthase as a homodimer with down-regulated uncoupled NADPH oxidase activity: tetrahydrobiopterin binding kinetics and role of haem in dimerization. Biochem J 1997;323:159–165. Chen P, Tsai A, Wu KK. Cysteine 184 of endothelial nitric oxide synthase is involved in heme coordination and catalytic activity. J Biol Chem 1994;269:25062–25066. Xie Q-W, Leung M, Fuortes M, Sassa S, Nathan C. Complementation analysis of mutants of nitric oxide synthase reveals that the active site requires two hemes. Proc Natl Acad Sci USA 1996;93:4891–4896. Richards MK, Marletta MA. Characterization of neuronal nitric oxide synthase and a C415H mutant, purified from a baculovirus overexpression system. Biochemistry 1994;33:14723–14732. P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 [37] Hemmens B, Gorren ACF, Schmidt K, Werner ER, Mayer B. Haem insertion, dimerization and reactivation of haem-free rat neuronal nitric oxide synthase. Biochem J 1998;332:337–342. [38] Brunner K, Tortschanoff A, Hemmens B et al. Sensitivity of flavin fluorescence dynamics in neuronal nitric oxide synthase to cofactorinduced conformational changes and dimerization. Biochemistry 1998;37:17545–17553. [39] Pufahl RA, Marletta MA. Oxidation of N-hydroxy-L-Arg by nitric oxide synthase: Evidence for involvement of heme in catalysis. Biochem Biophys Res Commun 1993;193:963–970. [40] Presta A, Liu J, Sessa WC, Stuehr DJ. Substrate binding and calmodulin binding to endothelial nitric oxide synthase co-regulate its enzymatic activity. Nitric Oxide 1997;1:74–87. [41] Abu-Soud HM, Feldman PL, Clark P, Stuehr DJ. Electron transfer in the nitric-oxide synthases. Characterization of L-arginine analogs that block heme iron reduction. J Biol Chem 1994;269:32318– 32326. [42] Salerno JC, McMillan K, Masters BS. Binding of intermediate, product, and substrate analogs to neuronal nitric oxide synthase: ferriheme is sensitive to ligand-specific effects in the L-arginine binding site. Biochemistry 1996;35:11839–11845. [43] McMillan K, Masters BSS. Optical difference spectrophotometry as a probe of rat brain nitric oxide synthase heme-substrate interaction. Biochemistry 1993;32:9875–9880. [44] Sennequier N, Stuehr DJ. Analysis of substrate-induced electronic, catalytic, and structural changes in inducible NO synthase. Biochemistry 1996;35:5883–5892. ´ [45] Rodrıguez-Crespo I, Gerber NC, OrtizdeMontellano PR. Endothelial nitric-oxide synthase. Expression in Escherichia coli, spectroscopic characterization, and role of tetrahydrobiopterin in dimer formation. J Biol Chem 1996;271:11462–11467. [46] Salerno JC, Martasek P, Roman LJ, Masters BS. Electron paramagnetic resonance spectroscopy of the heme domain of inducible nitric oxide synthase: binding of ligands at the arginine site induces changes in the heme ligation geometry. Biochemistry 1996; 35:7626–7630. [47] Gorren ACF, List BM, Schrammel A et al. Tetrahydrobiopterin-free neuronal nitric oxide synthase: Evidence for two identical highly anticooperative pteridine binding sites. Biochemistry 1996;35: 16735–16745. [48] Venema RC, Ju H, Zou R, Ryan JW, Venema VJ. Subunit interactions of endothelial nitric-oxide synthase: Comparisons to the neuronal and inducible nitric-oxide synthase isoforms. J Biol Chem 1997;272:1276–1282. [49] Wu C, Zhang J, Abu-Soud H, Ghosh DK, Stuehr DJ. High-level expression of mouse inducible nitric oxide synthase in Escherichia coli requires coexpression with calmodulin. Biochem Biophys Res Commun 1996;222:439–444. [50] Klatt P, Schmidt K, Lehner D et al. Structural analysis of porcine brain nitric oxide synthase reveals a role for tetrahydrobiopterin and L-arginine in the formation of an SDS-resistant dimer. EMBO J 1995;14:3687–3695. [51] Mayer B, Wu C, Gorren ACF et al. Tetrahydrobiopterin binding to macrophage inducible nitric oxide synthase: heme spin shift and dimer stabilization by the potent pterin antagonist 4-amino-tetrahydrobiopterin. Biochemistry 1997;36:15091–15095. [52] Ghosh DK, Wu C, Pitters E et al. Characterization of the inducible nitric oxide synthase oxygenase domain identifies a 49 amino acid segment required for subunit dimerization and tetrahydrobiopterin interaction. Biochemistry 1997;36:10609–10619. [53] Werner ER, Pitters E, Schmidt K, Wachter H et al. Identification of the 4-amino analogue of tetrahydrobiopterin as a dihydropteridine reductase inhibitor and a potent pteridine antagonist of rat neuronal nitric oxide synthase. Biochem J 1996;320:193–196. [54] Pfeiffer S, Gorren ACF, Pitters E et al. Allosteric modulation of rat brain nitric oxide synthase by the pterin-site enzyme inhibitor 4-aminotetrahydrobiopterin. Biochem J 1997;328:349–352. 529 [55] Mayer B, Werner ER. In search of a function for tetrahydrobiopterin in the biosynthesis of nitric oxide. Naunyn-Schmiedeberg’s Arch Pharmacol 1995;351:453–463. [56] Giovanelli J, Campos KL, Kaufman S. Tetrahydrobiopterin, a cofactor for rat cerebellar nitric oxide synthase, does not function as a reactant in the oxygenation of arginine. Proc Natl Acad Sci USA 1991;88:7091–7095. [57] Kaufman S. Tyrosine hydroxylase. Adv Enzymol Relat Areas Mol Biol 1995;70:103–220. [58] Presta A, Siddhanta U, Wu C et al. Comparative functioning of dihydro- and tetrahydropterins in supporting electron transfer, catalysis, and subunit dimerization in inducible nitric oxide synthase. Biochemistry 1998;37:298–310. [59] Abu-Soud HM, Gachhui R, Raushel FM, Stuehr DJ. The ferrousdioxy complex of neuronal nitric oxide synthase: Divergent effects of L-arginine and tetrahydrobiopterin on its stability. J Biol Chem 1997;272:17349–17353. [60] Venema RC, Sayegh HS, Kent JD, Harrison DG. Identification, characterisation, and comparison of the calmodulin-binding domains of the endothelial and inducible nitric oxide synthases. J Biol Chem 1996;271:6435–6440. [61] Salerno JC, Harris DE, Irizarry K et al. An autoinhibitory control element defines calcium-regulated isoforms of nitric oxide synthase. J Biol Chem 1997;272:29769–29777. [62] Venema RC, Sayegh HS, Arnal J-F, Harrison DG. Role of the enzyme calmodulin-binding domain in membrane association and phospholipid inhibition of endothelial nitric oxide synthase. J Biol Chem 1995;270:14705–14711. [63] Abu-Soud HM, Stuehr DJ. Nitric oxide synthases reveal a role for calmodulin in controlling electron transfer. Proc Natl Acad Sci USA 1993;90:10769–10772. [64] Gorren ACF, Schrammel A, Schmidt K, Mayer B. Thiols and neuronal nitric oxide synthase: complex formation, competitive inhibition, and enzyme stabilization. Biochemistry 1997;36:4360– 4366. [65] Abe J, Berk BC. Reactive oxygen species as mediators of signal transduction in cardiovascular disease. Trends Cardiovasc Med 1998;8:59–64. [66] Laursen JB, Rajagopalan S, Galis Z et al. Role of superoxide in angiotensin II-induced but not catecholamine-induced hypertension. Circulation 1997;95:588–593. ¨ [67] Mugge A, Elwell JH, Peterson TE et al. Chronic treatment with polyethylene glycolated superoxide dismutase partially restores endothelium-dependent vascular relaxations in cholesterol-fed rabbits. Circ Res 1991;69:1293–1300. [68] White CR, Brock TA, Chang L-Y et al. Superoxide and peroxynitrite in atherosclerosis. Proc Natl Acad Sci USA 1994;91:1044–1048. [69] Presta A, Weber-Main AM, Stankovich MT, Stuehr DJ. Comparative effects of substrates and pterin cofactor on the heme midpoint potential in inducible and neuronal nitric oxide synthases. J Am Chem Soc 1998;120:9460–9465. [70] Gonzalez-Zulueta M, Ensz LM, Mukhina G et al. Manganese superoxide dismutase protects nNOS neurons from NMDA and nitric oxide-mediated neurotoxicity. J Neurosci 1998;18:2040–2055. [71] Albina JE, Mills CD, Henry Jr. WL, Caldwell MD. Temporal expression of different pathways of L-arginine metabolism in healing wounds. J Immunol 1990;144:3877–3880. [72] Xia Y, Roman LJ, Masters BS, Zweier JL. Inducible nitric-oxide synthase generates superoxide from the reductase domain. J Biol Chem 1998;273:22635–22639. ´ [73] Cosentino F, Patton S, dUscio LV et al. Tetrahydrobiopterin alters superoxide and nitric oxide release in prehypertensive rats. J Clin Invest 1998;101:1530–1537. [74] Pritchard KA, Groszek L, Smalley DM et al. Native low-density lipoprotein increases endothelial cell nitric oxide synthase generation of superoxide anion. Circ Res 1995;77:510–518. [75] Xia Y, Tsai A-L, Berka V, Zweier JL. Superoxide generation from 530 [76] [77] [78] [79] [80] [81] [82] [83] [84] [85] [86] [87] [88] [89] [90] [91] [92] [93] [94] [95] [96] [97] P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 endothelial nitric-oxide synthase: A Ca 21 / calmodulin-dependent and tetrahydrobiopterin regulatory process. J Biol Chem 1998;273:25804–25808. ´ ´ Vasquez-Vivar J, Kalyanaraman B, Martasek P et al. Superoxide generation by endothelial nitric oxide synthase: The influence of cofactors. Proc Natl Acad Sci USA 1998;95:9220–9225. Beckman JS, Koppenol WH. Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and the ugly. Am J Physiol 1996;40:C1424–C1437. Mayer B, Pfeiffer S, Schrammel A et al. A new pathway of nitric oxide / cyclic GMP signaling involving S-nitrosoglutathione. J Biol Chem 1998;273:3264–3270. Griscavage JM, Fukoto JM, Komori Y, Ignarro LJ. Nitric oxide inhibits neuronal nitric oxide synthase by interacting with the heme prosthetic group. J Biol Chem 1994;269:21644–21649. Abu-Soud HM, Wang J, Rousseau DL et al. Neuronal nitric oxide synthase self-inactivates by forming a ferrous-nitrosyl complex during aerobic catalysis. J Biol Chem 1995;270:22997–23006. Mayer B, Klatt P, Werner ER, Schmidt K. Kinetics and mechanism of tetrahydrobiopterin-induced oxidation of nitric oxide. J Biol Chem 1995;270:655–659. Myers PR, Minor Jr. RL, Guerra Jr. R, Bates JN, Harrison DG. Vasorelaxant properties of the endothelium-derived relaxing factor more closely resemble S-nitrosocysteine than nitric oxide. Nature 1990;345:161–163. Davidson CA, Kaminski PM, Wu M, Wolin MS. Nitrogen dioxide causes pulmonary arterial relaxation via thiol nitrosation and nitric oxide formation. Am J Physiol 1996;270:H1038–H1043. Beckman JS, Ye YZ, Anderson P et al. Extensive nitration of protein tyrosines observed in human atherosclerosis detected by immunohistochemistry. Biol Chem Hoppe-Seyler 1994;375:81–88. Pfeiffer S, Mayer B. Lack of tyrosine nitration by peroxynitrite generated at physiological pH. J Biol Chem 1998;273:27280–27285. Eiserich JP, Hristova M, Cross CE et al. Formation of nitric oxide-derived inflammatory oxidants by myeloperoxidase in neutrophils. Nature 1998;391:393–397. Vanhoutte PM. Endothelial dysfunction and atherosclerosis. Eur Heart J 1997;18(Suppl E):E19–E29. Harrison DG. Cellular and molecular mechanisms of endothelial cell dysfunction. J Clin Invest 1997;100:2153–2157. Balligand J-L, Kelly RA, Marsden PA, Smith TW, Michel T. Control of cardiac muscle cell function by an endogenous nitric oxide signalling system. Proc Natl Acad Sci USA 1993;90:347–351. Schulz R, Smith JA, Lewis MJ, Moncada S. Nitric oxide synthesis in cultured endocardial cells of the pig. Br J Pharmacol 1991;104:21–24. Liao JK, Zulueta JJ, Yu F-S et al. Regulation of bovine endothelial constitutive nitric oxide synthase by oxygen. J Clin Invest 1995;96:2661–2666. Goetz RM, Morano I, Calovini T, Studer R, Holtz J. Increased expression of endothelial constitutive nitric oxide synthase in rat aorta during pregnancy. Biochem Biophys Res Commun 1994;205:905–910. Sessa WC, Pritchard K, Seyedi N, Wang J, Hintze TH. Chronic exercise in dogs increases coronary vascular nitric oxide production and endothelial cell nitric oxide synthase gene expression. Circ Res 1994;74:349–353. Rees DD, Palmer RM, Moncada S. Role of endothelium-derived nitric oxide in the regulation of blood pressure. Proc Natl Acad Sci USA 1989;86:3375–3378. Boulanger CM, Vanhoutte PM. G proteins and endothelium-dependent relaxations. J Vasc Res 1997;34:175–185. Nishida K, Harrison DG, Navas JP et al. Molecular cloning and characterisation of the constitutive bovine aortic endothelial cell nitric oxide synthase. J Clin Invest 1992;90:2092–2096. Awolesi MA, Sessa WC, Sumpio BE. Cyclic strain upregulates nitric oxide synthase in cultured bovine aortic endothelial cells. J Clin Invest 1995;96:1449–1454. [98] Ohno M, Gibbons GH, Dzau VJ, Cooke JP. Shear stress elevates endothelial cGMP. Role of a potassium channel and G protein coupling. Circulation 1993;88:193–197. [99] Shaul PW, Smart EJ, Robinson LJ et al. Acylation targets endothelial nitric-oxide synthase to plasmalemmal caveolae. J Biol Chem 1996;271:6518–6522. ˜ G, Martasek ´ ´ [100] Garcıa-Cardena P, Masters BSS et al. Dissecting the interaction between nitric oxide synthase (NOS) and caveolin: Functional significance of the NOS caveolin binding domain in vivo. J Biol Chem 1997;272:25437–25440. [101] Ghosh S, Gachhui R, Crooks C, Wu C, Lisanti M, Stuehr DJ. Interaction between caveolin-1 and the reductase domain of endothelial nitric-oxide synthase. Consequences for catalysis. J Biol Chem 1998;273:22267–22271. [102] Ju H, Venema VJ, Marrero MB, Venema RC. Inhibitory interactions of the bradykinin B2 receptor with endothelial nitric-oxide synthase. J Biol Chem 1998;273:24025–24029. [103] Couet J, Li S, Okamoto T, Ikezu T, Lisanti MP. Identification of peptide and protein ligands for the caveolin-scaffolding domain. Implications for the interaction of caveolin with caveolae-associated proteins. J Biol Chem 1997;272:6525–6533. [104] Robinson LJ, Busconi L, Michel T. Agonist-modulated palmitoylation of endothelial nitric oxide synthase. J Biol Chem 1995;270:995–998. [105] Feron O, Michel JB, Sase K, Michel T. Dynamic regulation of endothelial nitric oxide synthase: Complementary roles of dual acylation and caveolin interactions. Biochemistry 1998;37:193– 200. [106] Ignarro LJ, Bush PA, Buga GM et al. Nitric oxide and cyclic GMP formation upon electrical field stimulation cause relaxation of corpus cavernosum smooth muscle. Biochem Biophys Res Commun 1990;170:843–850. [107] Rand MJ, Li CG. Nitric oxide as a neurotransmitter in peripheral nerves: Nature of transmitter and mechanism of transmission. Annu Rev Physiol 1995;57:659–682. [108] Kennedy MB. Origin of PDZ (DHR, GLGF) domains. Trends Biochem Sci 1995;20:350. [109] Brenman JE, Chao DS, Xia HH, Aldape K, Bredt DS. Nitric oxide synthase complexed with dystrophin and absent from skeletal muscle sarcolemma in Duchenne muscular dystrophy. Cell 1995;82:743–752. [110] Brenman JE, Chao DS, Gee SH et al. Interaction of nitric oxide synthase with the postsynaptic density protein PSD-95 and alpha 1-syntrophin mediated by PDZ domains. Cell 1996;84:757–767. [111] Stricker NL, Christopherson KS, Yi BA et al. PDZ domain of neuronal nitric oxide synthase recognizes novel C-terminal peptide sequences. Nat Biotechnol 1997;15:336–342. [112] Venema VJ, Ju H, Zou R, Venema RC. Interaction of neuronal nitric-oxide synthase with caveolin-3 in skeletal muscle. Identification of a novel caveolin scaffolding / inhibitory domain. J Biol Chem 1997;272:28187–28190. [113] Huang ZH, Huang PL, Panahian N et al. Effects of cerebral ischemia in mice deficient in neuronal nitric oxide synthase. Science 1994;265:1883–1885. [114] MacMicking JD, Nathan C, Hom G et al. Altered responses to bacterial infection and endotoxic shock in mice lacking inducible nitric oxide synthase. Cell 1995;81:641–650. [115] Gross SS, Jaffe EA, Levi R, Kilbourn RG. Cytokine-activated endothelial cells express an isotype of nitric oxide synthase which is tetrahydrobiopterin-dependent, calmodulin-independent, and inhibited by arginine analogues. Biochem Biophys Res Commun 1991;178:823–829. [116] Balligand J-L, Ungureanu-Longrois D, Simmons WW et al. Cytokine-inducible nitric oxide synthase (iNOS) expression in cardiac myocytes. J Biol Chem 1994;269:27580–27588. [117] Geller DA, Lowenstein CJ, Shapiro RA et al. Molecular cloning and expression of inducible nitric oxide synthase from human hepatocytes. Proc Natl Acad Sci USA 1993;90:3491–3495. P. J. Andrew, B. Mayer / Cardiovascular Research 43 (1999) 521 – 531 [118] Buttery LDK, Springall DR, Chester AH et al. Inducible nitric oxide synthase is present within human atherosclerotic lesions and promotes the formation and activity of peroxynitrite. Lab Invest 1996;75:77–85. [119] Kessler P, Bauersachs J, Busse R, Schini-Kerth VB. Inhibition of inducible nitric oxide synthase restores endothelium-dependent relaxations in proinflammatory mediator-induced blood vessels. Arterioscler Thromb Vasc Biol 1997;17:1746–1755. [120] Shears II LL, Kawaharada N, Tzeng E et al. Inducible nitric oxide synthase suppresses the development of allograft arteriosclerosis. J Clin Invest 1997;100:2035–2042. ˜ G, Nathan CF, Weiss ´ [121] Wheeler MA, Smith SD, Garcıa-Cardena RM, Sessa WC. Bacterial infection induces nitric oxide synthase in human neutrophils. J Clin Invest 1997;99:110–116. [122] Vodovotz Y, Russell D, Xie Q-W, Bogdan C, Nathan C. Vesicle membrane association of nitric oxide synthase in primary mouse macrophages. J Immunol 1995;154:2914–2925. ¨ [123] Schmidt HHHW, Warner TD, Nakane M, Forstermann U, Murad F. Regulation and subcellular location of nitrogen oxide synthases in RAW264.7 macrophages. Mol Pharmacol 1992;41:615–624. ´ ´ [124] Vidal F, Colome´ C, Martınez-Gonzalez J, Badimon L. Atherogenic concentrations of native low-density lipoproteins down-regulate nitric-oxide-synthase mRNA and protein levels in endothelial cells. Eur J Biochem 1998;252:378–384. [125] Bogle RG, Baydoun AR, Pearson JD, Moncada S, Mann L GE. L-Arginine transport is increased in macrophages generating nitric oxide. Biochem J 1992;284:15–18. ¨ [126] Nussler AK, Billiar TR, Liu Z-Z, Morris Jr. SM. Coinduction of nitric oxide synthase and argininosuccinate synthetase in a murine macrophage cell line: implications for regulation of nitric oxide production. J Biol Chem 1994;269:1257–1261. [127] Corraliza IM, Soler G, Eichmann K, Modolell M. Arginase induction by suppressors of nitric oxide synthesis (IL-4, IL-10 and [128] [129] [130] [131] [132] [133] [134] [135] 531 PGE2) in murine bone-marrow-derived macrophages. Biochem Biophys Res Commun 1995;206:667–673. Werner ER, Werner-Felmayer G, Mayer B. Tetrahydrobiopterin, cytokines and nitric oxide. Proc Soc Exp Biol Med 1998;219:171– 182. Hecker M, Sessa WC, Harris HJ, Anggard EE, Vane JR. The metabolism of L-arginine and its significance for the biosynthesis of endothelium-derived relaxing factor: Cultured human endothelial cells recycle L-citrulline to L-arginine. Proc Natl Acad Sci USA 1990;87:8612–8616. ¨ Arnal JF, Munzel T, Venema RC et al. Interactions between L-arginine and L-glutamine change endothelial NO production: An effect independent of NO synthase substrate availability. J Clin Invest 1995;95:2565–2572. ¨ Pollock JS, Forstermann U, Mitchell JA et al. Purification and characterisation of particulate endothelium-derived relaxing factor synthase from cultured and native bovine aortic endothelial cells. Proc Natl Acad Sci USA 1991;88:10480–10484. Theilmeier G, Chan JR, Zalpour C et al. Adhesiveness of mononuclear cells in hypercholesterolemic humans is normalized by dietary L-arginine. Arterioscler Thromb Vasc Biol 1997;17:3557– 3564. Bode-Boger SM, Boger RH, Kienke S, Junker W, Frohlich JC. Elevated L-arginine / dimethylarginine ratio contributes to enhanced systemic NO production by dietary L-arginine in hypercholesterolemic rabbits. Biochem Biophys Res Commun 1996;219:598– 603. Giugliano D, Marfella R, Verrazzo G et al. The vascular effects of L-arginine in humans. The role of endogenous insulin. J Clin Invest 1997;99:433–438. MacAllister RJ, Calver AL, Collier J et al. Vascular and hormonal responses to arginine: provision of substrate for nitric oxide or non-specific effect? Clin Sci Colch 1995;89:183–190.