* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Artificial heart valve wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
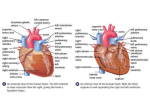
Warm-Up 1. What is the pacemaker? Where is it located? 2. List the parts of the intrinsic conduction system of the heart. 3. Draw and label the 3 waves of a typical EKG tracing. What is happening at each wave? 4. What causes the heart sounds (lub-dub)? Warm-Up 1. Compare arteries, capillaries, & veins. 2. Imagine you are a red blood cell. List the pathway you would travel through the body in a complete circuit starting at a pinky toe. 3. Explain how blood pressure is measured. Warm-Up 1. What is hypertension? What are possible causes? 2. What is atherosclerosis? 3. What can you do to prevent atherosclerosis? 4. What treatment options are available for patients with coronary atherosclerosis? Warm-Up Draw the human heart and the main blood vessels in/out of the heart. Label the following on your diagram: 4 chambers 4 valves All blood vessels going into/out of heart Using a blue pencil, indicate oxygen-poor blood flow Using a red pencil, indicate oxygen-rich blood flow Chapter 13 Cardiovascular System Major Functions Transport O2 and nutrients to tissues Remove wastes from tissues Anatomy and Location of Heart Size of fist Weight < 1 lb. Within mediastinum of thoracic cavity Apex points toward left hip Flanked by lungs Surrounded by pericardium (double-walled sac) Pericardium – encloses the heart 3 layers Fibrous pericardium - outer layer; attached to diaphragm Visceral pericardium - inner layer; covers heart Parietal pericardium - inner lining of the fibrous pericardium Pericardial Cavity Space between parietal and visceral pericardium filled with serous fluid to reduce friction during heart contractions Pericarditis – inflammation of pericardium Pericarditis Layers of the Heart Wall 1. Epicardium – outer layer (pericardium) Heart chamber 2. Myocardium – cardiac muscle 3. Endocardium – endothelium lines chambers Heart Chambers Right Side Atrium (R & L): receive blood (entryway) Ventricle (R & L): pump blood out Septum: wall between atria & ventricles Valves: prevent backflow of blood Left Side Atria Upper chambers Thin walls Left atrium Receives blood returning from the lungs via pulmonary veins Right atrium Receives blood from superior and inferior vena cava and the coronary sinus Auricles on top of atria Help atria receive more blood Ventricles Lower chambers Thick-muscled to pump blood to body Contains: Papillary muscles Contract when the ventricle contracts; attached to Chordae tendinae Chordae tendinae Attach to valves to keep them from swinging back into the atria Right Ventricle Pulmonary circuit = low pressure Left Ventricle Systemic circuit = high resistance to blood flow More powerful pump 3x as thick as right ventricle Heart Valves Prevent back flow of blood Atrioventricular (A-V) valves: Tricuspid valve Between Bicuspid (mitral) valve Between left atria and left ventricle Pulmonary semilunar valve right atria and right ventricle Between right ventricle and pulmonary artery Aortic semilunar valve Between the left ventricle and aorta Mitral Valve Prolapse Affects up to 6% of the population Bicuspid valves stretch and bulge into the left atrium Susceptible to endocarditis Bacterial infection Prevent with antibiotics Symptoms Chest pain, palpitations, fatigue, anxiety Endocarditis Double Circulation Loop Pulmonary circuit: blood to/from lungs Systemic circuit: blood to/from all body tissues Pathway of Blood Through Heart Pathway of Blood Vena cava/coronary sinus Right atrium Tricuspid Right ventricle Pulmonary semilunar valve Pulmonary arteries (deoxygenated blood) Lungs Pulmonary veins (oxygenated blood) Left atrium Bicuspid Left ventricle Aortic semilunar valve Aorta Body organs, tissues, and cells Coronary Vessels First 2 branches of the aorta Supply heart tissue with blood Myocardium Contains MANY capillaries Drained by coronary veins Veins empty into coronary sinus Returns the blood to the right atria Cardiac Cycle Series of events that constitute a heartbeat Pressure within the heart chambers rises and falls with the contraction and relaxation of atria and ventricles 70% - flows naturally 30% - needs to be pumped 0.8 seconds for one cycle to be completed Heart Sounds “Lub”: closing of AV valves “Dub”: semilunar valves close at end of systole Murmur – abnormal sounds that indicate valve problem Heart Rhythm Cardiac muscle cells can contract spontaneously and independently Regulation of heart activity: 1. Autonomic nervous system ▪ Epinephrine, thyroxine: heart rate ▪ Low Ca2+ levels: heart rate 2. Intrinsic conduction system ▪ Built into heart tissue & sets basic rhythm ▪ Pacemaker = Sinoatrial (SA) Node Intrinsic conduction system Sequence of action: 1. Sinoatrial (SA) node – right atrium Generates impulses Starts each heartbeat 2. Atrioventricular (AV) node – between atria & ventricles Atria contract 3. Bundle of His (or AV bundle) 4. Bundle branches – interventricular septum 5. Purkinje fibers – spread within ventricle walls Ventricles contract Homeostatic Imbalances Angina pectoris: Heart muscle deprived of O2 Crushing chest pain Myocardial infarction (Heart Attack): Prolonged angina Heart cells may die Homeostatic Imbalances Ischemia: lack of adequate blood supply to heart Fibrillation: uncoordinated shuddering of heart muscle, useless pump Major cause of death from heart attacks Heartbeat Regulation Amount of blood pumped at any one time must adjust to the current needs of the body (more is needed during strenuous exercise) S-A node is innervated by branches of the sympathetic and parasympathetic divisions Medulla oblongata maintains a balance between the sympathetic and parasympathetic divisions of the nervous system Impulses from cerebrum or hypothalamus may also influence heart rate So do body temperature and the concentrations of certain ions Norepinephrine - increases contractions Acetylcholine - decreases contractions Electrocardiogram (ECG/EKG) Records the electrical activity of the heart Electrocardiograph: graphic record of heart activity How to read an ECG P wave: atria contact QRS complex: ventricles contract T wave: ventricles relax Abnormal EKG Tachycardia - >100 beats/min Bradycardia - <60 beats/min Flutter - rapid; 250-350 beats/min. Fibrillation - rapid; uncoordinated Heart becomes useless as a pump Overview of EKG Blood Vessels Vascular System: blood circulates inside closed transport systems Types of Blood Vessels: Arteries (takes blood away from heart) Arterioles Capillary beds Venules Veins (return blood back to heart) Arteries Capillaries Blood away from heart • Walls 1-cell thick Thicker walls • Exchange gases Withstand high pressure between blood and Aorta - largest tissue cells Vasoconstriction • Form connections • Contract between arterioles and • Diameter reduced venules • Vasodilation • • • • • • Relax • Diameter increased Veins Blood back to heart Thinner walls Low pressure Large lumen Valves: prevent blood backflow • Skeletal muscles enhance venous return • • • • • Varicose Veins People stand for long periods of time inactivity or pressure on veins Blood pools in feet and legs Valves weaken veins become twisted & dilated Treatment: compression stockings, exercise, laser treatment, surgery Homeostatic Imbalances Atherosclerosis – artery walls thicken due to fatty deposits (plaques) Treatments By-pass Angioplasty (stent) Atherosclerosis Angioplasty vs. Bypass Surgery Bypass Congestive Heart Failure Progressive weakening of heart Low heart efficiency circulation inadequate to meet tissue needs Caused by: Coronary atherosclerosis Persistent high blood pressure Multiple heart attacks – scar tissue New heart surgery technology Untold stories of the ER Vital Signs Pulse: expansion & recoil of an artery with each beat of left ventricle Pressure points (eg. carotid artery, radial artery) Normal resting: 70-76 beats/min Vital Signs Blood pressure: pressure of blood on inner walls of blood vessels Directly What related to volume of blood happens to when blood is lost? Stroke volume ~ 70ml discharged Blood volume = sum of blood cells + plasma Hypertension – persistent elevated blood pressure (>140/90) Measuring Blood Pressure Systolic pressure: peak of ventricular contraction (top #) Diastolic pressure: ventricles relaxed (bottom #) Written: Systolic/Diastolic Normal: (120 mm Hg)/(70 mm Hg) or 120/70 Using a Sphygmomanometer Wrap cuff around upper arm Place stethoscope on brachial artery Inflate cuff to 180 mm Hg Slowly release air listen for whooshing sounds in brachial artery (Korotkoff sounds) Systolic: when sound begin to appear Diastolic: when sounds disappear