* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download DYSRHYTHMIAS
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Jatene procedure wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Atrial fibrillation wikipedia , lookup
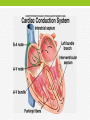
DYSRHYTHMIAS NUR – 224 MS. GARDNER DYSRHYTHMIAS • Disorder of conduction of the electrical impulse within the heart. • Cause disturbances with heart rate/heart rhythm or both. • Diagnosed by analyzing the electrocardiographic (ECG/EKG). • Treatment based on frequency and severity of symptoms • Named according to the site of origin of the impulse and the conduction involved. Normal Electrical Conduction • Electrical impulse stimulates and paces the cardiac muscle and normally originates in the SA node. • Rate 60-100 bpm • All beats appear in a similar pattern, equally spaced, and have three major units: P wave, QRS complex, and T wave. Heart/ECG • Each wave represents transmission of an electrical • • • • • impulse through the heart muscle (depolarization) causes the muscle to contract and eject blood. P wave – reflects impulse going through the atria. QRS complex - reflects impulse going through the ventricles. T wave - is produced by the electrical recovery (repolarization) of the ventricle. Depolarization – electrical stimulation/contraction Repolarization – electrical relaxation Normal Electric Pathway • Electrical impulse originates in the sinoatrial (SA) node. • The impulse spreads through the intra-atrial pathways to • • • • the atrio-ventricular(AV) node. The structure of the AV node slows the electrical impulse giving the atria time to contract and fill ventricles with blood. (atrial kick) After a brief delay, the impulse continues through the bundle of His, the R/L bundle branches, Purkinje fibers located in the ventricular muscle. This stimulation causes the ventricles to contract (systole) The heart rate is influenced by the autonomic nervous system sympathetic/parasympathetic nerve fibers Electrocardiogram • Electrical impulse travels through the heart the end • • • • product is an ECG. ECG is obtained by placing electrodes on the body – on the limbs and chest. The electrodes create an imaginary line lead. Waveforms that appear on the paper/cardiac monitor represent the electrical current in relation to the lead. Electrodes are attached to a cable wire which may be connected to ECG machine, cardiac monitor, telemetry monitor, Holter monitoring. 12-lead ECG 10 electrodes, reflects the activity in the left ventricle. Interpretation • ECG waveforms are printed on graph paper that is divided by light and dark vertical and horizontal lines. • ECG waveform moves to the top of the paper positive deflection • ECG moves toward the bottom of the paper negative deflection • Each waveform should be compared and examined with others. Interpretation • ECG – composed of waveforms (P wave, QRS complex, T wave) P wave – first upward deflection represents atrial depolarization. usually not more than 3 small blocks. QRS complex – ventricular depolarization. consist of three deflections: Q wave, the first downward stroke, R wave first upward stroke; S wave downward stroke following the R wave. normal duration of the QRS complex is less than three small blocks (0.12 seconds). Interpretation T wave • represents ventricular repolarization/electrical recovery of the ventricular contraction. PR interval • measures from the beginning of the P wave to the onset of the Q wave. • represents conduction of the impulse through the atria and into the AV node. ST segment • begins at the end of the S wave and ends at the beginning of the T wave. U wave Small upward deflection following the T wave. Seldom present. Interpretation PP interval • measured from one P wave to the beginning to the next P wave • used to determine atrial rhythm and atrial rate RR interval • measured from one QRS complex to the next QRS complex. • RR interval used to determine ventricular rate and rhythm. Analyzing the Rhythm Strip • Count the number of complexes in a 6 –second strip and multiply that number by 10. (useful for irregular rhythms) Analyze in a systematic manner: • Rhythm – regular • Rate – 60-100 beats/minute • P wave – present and upright /all shaped alike • PR interval - P wave precedes QRS duration (0.12 -0.20 sec.) time interval same for all beats • QRS interval – present /all shaped alike duration not more than 3 small squares (0.12 sec.) Normal Sinus Rhythm • Rhythm – regular • Rate – 60-100 beats/minute • P wave – present and upright /all shaped alike • PR interval - P wave precedes QRS • • • • • duration (0.12 -0.20 sec.) time interval same for all beats QRS interval – present /all shaped alike duration not more than 3 small squares (0.12 sec.) Sinus Bradycardia • Dysrhythmias heart rate below 60, complex remain normal • Causes: sleep, athletic training, hypothyroidism, medications, myocardial infarction • Atropine IV medication of choice for treatment bradycardia Sinus Tachycardia • All complexes are normal. The heart rate is more than100. • Causes: Physiologic stress Medication • Treatment: usually secondary to factors outside the heart, treatment is directed to treat the underlying cause Sinus Arrhythmia • All complexes are normal, but the heart rate is irregular. • The rate increases with inspiration and decreases with expiration • Does not cause any significant hemodynamic effect and usually is not treated Atrial Dysrhythmias • Portions of atrial tissue may become excitable and initiate impulses. • These impulses will control the heartbeat if they occur at a rate faster than impulses from the SA node. • Premature atrial complex • Atrial flutter • Atrial fibrillation Premature Atrial Complex • A single complex beat that occurs when an electrical impulse appears early in the cycle – before the next sinus beat. • Cause: caffeine, nicotine, anxiety, hypokalemia • PACs are common normal heartbeats • If infrequent - no treatment is necessary. Atrial Flutter • Is a rapid, regular fluttering of the atrium. • The atrial rate is between 250/400 times/minute. • P wave takes on a saw toothed appearance • Cause: open heart surgery, valvular disease • Treatment: Adenosine, vagal maneuvers, electrical cardioversion, medications, catheter ablation Atrial Fibrillation • Uncoordinated atrial electrical activity that causes a rapid • • • • disorganization and uncoordinated twitching of the atria P waves – (fibrillatory waves) assume different shapes because they are coming from different foci in the atrium. No PR interval can be determined Cause: CAD, open heart surgery, obesity, diabetes Treatment: Ventricular Dysrhythmias Ventricular tissue becomes more excitable as a result of ischemia, drug effect or electrolyte imbalance. These dysrhythmias may diminish the ability of the heart to function as a pump. Without adequate blood flow, all organs deteriorate. Premature ventricular complex Ventricular tachycardia Ventricular fibrillation Ventricular asystole Premature Ventricular Complex • Impulse that starts in the ventricles and is conducted • • • • throughout the ventricle before the next normal sinus impulse. Can occur in healthy people coffee, smoking, alcohol. PVCs are usually not serious Treatment: correct the underlying cause, if PVCs are frequent and consistent amiodarone/lidocaine Bigeminy, trigeminy, multifocal Multifocal PVC - Quadrigeminy Ventricular Tachycardia • Three or more PVCs in a row, rate exceeds 100 bpm. • Is an emergency the patient is usually unresponsive and pulseless, leads to reduce cardiac output. • Treatment: antiarrhythmic medication, pacing, or cardioversion • If patient is unconscious and without a pulse immediate defibrillation Ventricular Fibrillation • Most common dysrhythmia in patients with cardiac arrest • Rapid, disorganized ventricular rhythm that cause • • • • ineffective quivering of the ventricles No atrial activity is seen on ECG Characterized by: absence of an audible heartbeat, a palpable pulse, and respirations There is no coordinated cardiac activity cardiac arrest and death are imminent if the dysrhythmia is not corrected Defibrillation/cardiopulmonary resuscitation (CPR) Ventricular Asystole Ventricular Asystole • Flatline, • No QRS complex • P waves may be apparent for a short duration • There is no heartbeat, no palpable pulse, and no respiration • Without immediately treatment – fatal • Treatment – CPR, intubation, IV access Assessment • Cardiac dysrhythmias – either begin/critical • Diagnostic Test electrocardiogram cardiac monitoring electrophysiology Nursing Interventions • Monitoring/ECG monitoring • Administration of medications/medication effects • Adjunct therapy: cardioversion, defibrillation, pacemakers • Other Adjunctive Modalities • Medications not working • Common therapies: elective cardioversion defibrillation implantable devices internal cardio defibrillators Pacemakers Is a pulse generator used to provide an electrical stimulus to the heart when the heart fails to generate/conduct its own rate that maintains cardiac output. Are programmed to stimulate the atria or the ventricles, or both Pacing is detected on the ECG strip by the presence of pacing artifact – a sharp spike is noted • Power source may be internal/external • Several different types: Temporary Permanent Pacemaker • Paces the heart when normal conduction pathway is damaged. • Basic unit – power source, one or more conducting leads • The electrical signal travels from the pacemaker, through the leads, the walls of the myocardium. • The myocardium is “captured” and stimulated to contract Pacemaker • Permanent • Implanted totally within the body • The power source is placed subcutaneously, usually over the pectoral muscle on the patient’s nondominant side • The pacing leads are leads are threaded transvenously to right atrium and one/both ventricles and attached to the power source. Pacemakers • Temporary • Power source is outside the body • Different types Epicardial pacing Transvenous pacing Transcutaneous pacing Epicardial pacing Pacing on Demand Pacemaker Patient teaching • Follow-up care • Report s/s infection • Keep incision dry • Avoid lifting arm on pacemaker site • Airport travel is not restricted • Carry pacemaker information card • Wear Medic-alert ID band Cardioversion and Defibrillation • Treat tachy dysrhythmias by delivering electrical current that depolarizes myocardial cells • When cells repolarize, sinus node usually able to recapture role as heart pacemaker • Cardioversion current delivered is synchronized with patient’s ECG • Defibrillation current delivered is unsynchronized and immediate Paddle placement Cardioversion • A synchronized circuit in the defibrillator delivers a direct • • • • • • • electrical current synchronized with the patient’s heart rhythm. Countershock that is programmed to occur with the R wave of the QRS complex. Used for nonemergency basis – Used to treat – atrial fibrillation, atrial flutter, stable ventricular tachycardia Patient is awake/hemodynamically stable Sedation prior to the procedure Patent airway Initial energy less than what is needed for defibrillation – 50 – 100 joules Defibrillation • Choice of treatment of choice to terminate VF/pulseless • • • • VT. Defibrillation is accomplished by delivering direct current without regard to the cardiac cycle. The output of the defibrillator is measured in joules/watts – 200 -360 joules If defibrillation is unsuccessful, CPR is immediately initiated Defibrillation, CPR, medication administration continues until a stable rhythm resumes or until it is established that the patient will not recover. Safety Measures • Assure good contact between skin, pads or paddles • Use conductive medium, 20 to 25 pounds of pressure • Place paddles so they do not touch bedding or clothing, • • • • • are not near medication patches or oxygen flow If cardioverting, turn synchronizer on If defibrillating, turn synchronizer off Do not charge device until ready to shock Call “clear” three times; follow checks required for clear Assure no one is in contact with patient, bed, or equipment Implantable Cardioverter Defibrillator (ICD) • Detect changes in cardiac rhythm and automatically delivers an electric shock to convert the dysrhythmia back into normal sinus rhythm. • Used for sudden death survivors, recurrent ventricular tachycardia • Monitors the heart rate and rhythm and identifies VT. Approximately 25 seconds after system detects a lethal dysrhythmia, the mechanism delivers 25 joules or less of shock to the patient’s heart. • If the first shock is unsuccessful , the generator will recycle itself and continue to deliver shock ICD Nursing Management • Complications similar to those associated with pacemaker • • • • • • • • insertion Avoid driving until instructed by HCP No MRI Air travel not restricted If ICD fires – contact HCP immediately If fires and client does not feel well – contact HCP Medic-Alert ID Caregivers should know CPR Teaching – lifestyle changes, periodic device monitoring, safety, surgical site care