* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Packet 18- Kidneys
Survey
Document related concepts
Transcript
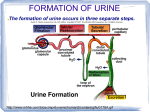
Lecture 18: Kidneys Silverthorn Chapter 19 Primary functions of the kidneys 10. Regulating osmolarity (blood concentration!) A. Regulating blood pressure B. Maintaining ion balance C. Regulating blood pH 11. Excretion of waste products (either ingested or produced through metabolic reactions) Important Kidney Anatomy 1. Nephron- functional unit of the kidney A. Up to 1 million nephrons/kidney (med pg 310) B. After age 40, number of nephrons decreases 1%/year…but the body compensates, so it isn’t usually a problem… 2. Each nephron is associated with a unique blood supply… A. Big picture—renal artery flows IN, renal vein flows OUT B. Little picture? i. Afferent arteriole → glomerulus (capillary bed) → efferent arteriole → peritubular capillaries (sometimes specialize as vasa recta) → veins… Mechanisms of kidney function 1. Filtration: removing fluid and solutes, en masse, from the blood, and collecting the “stuff” in the nephron tubules. A. This produces FILTRATE in the nephron tubule…but if the substance should be kept in the body, it must be reabsorbed! 2. Reabsorption: taking substances from the filtrate and returning them to the blood 3. Secretion: Selectively removing molecules from the blood and adding them to the filtrate. (Note: This is much different from filtration which is non-specific) 4. Excretion: Removal of substances from the body FILTRATION 1. 180L fluid filtered OUT of the blood EVERY SINGLE DAY! Or entire plasma volume is filtered out 60x per day! Whaaaat?! 2. Occurs in the glomerulus/Bowman’s capsule 3. Filtration is powered by hydrostatic pressure in the blood (180L net filtration) A. Anatomical (structural) characteristics enable filtration i. Fenestrations in epithelium of glomerular capillaries (slits that allow fluid through, but are generally too small for plasma proteins to pass) ii. This creates very LEAKY capillaries in the glomerulus! iii. Leaky epithelial cells in Bowman’s Capsule B. First, review blood pressure in other capillaries…3 L net filtration… i. Hydrostatic pressure: 32 mmHg → 15 mmHg OUT (over the length of the capillary) ii. Osmotic pressure: 25 mmHg IN (constant over cap length, b/c # prot doesn’t change) iii. Net filtration OUT (3 L) C. Blood pressure in the glomerulus is HIGH! i. 55 mmHg OUT… a. Blood pressure (32 mmHg) b. Where does the extra “pressure” come from? Big afferent, small efferent vessels… ii. 45 mmHg IN a. (Osmotic pressure pushing IN due to proteins…30 mm Hg) b. (Hydrostatic pressure in the bowman’s capsule pushing IN: 15) iii. 10 mmHg push stuff OUT. a. This total pressure influences GFR b. Increase this pressure (HOW???) and you increase GFR c. Decrease this pressure and you decrease GFR… 4. You now have filtrate in Bowman’s capsule (180L/day) that is similar in composition to plasma (but no plasma proteins). 5. At any given moment, only 20% of the plasma is filtered OUT…(why not more?) Bio 7: Human Physiology 60 Spring 2014: Riggs A. Rate of filtration is quantified by the Glomerular Filtration Rate (GFR), which is influenced by changes in resistance in afferent or efferent arterioles 6. Now you’ve got a LOT of filtrate…what do to with it??? REABSORB the stuff you need (water, ions, sugars…) Cells of the Nephron The characteristics of the cells making up the nephron tubules determine whether REABSORPTION (from tubule back into the blood) and/or SECRETION (from blood into tubule) will occur next. Proximal convoluted tubule 1. 2. 3. 4. Very permeable to water and solutes High surface area, to maximize reabsorption (70% of fluid reabsorbed here!) Lots of mitochondria (to fuel active transport of Na+) On the luminal (aka “apical”) membrane (touching tubule lumen) A. SGLT transporters… Na+ comes into the cell (down the conc gradient) and brings glucose with it! 5. On the basolateral membrane (touching the interstitial fluid): A. NaK Pump!!! (3 Na+ out, 2 K+ in…)…uses ATP B. Maintains the Na+ conc gradient C. (K+ leaks out of open channels, preventing too much K+ from accumulating in the cell, or being excreted in the urine) D. GLUT takes advantage of the glucose conc gradient, allowing reabsorption of glucose into interstitial fluid! 6. The actions on both membranes essentially reabsorb solutes into the interstitium… inevitably, water will follow. 7. 70% of all filtrate is reabsorbed here utilizing these mechanisms! 8. The amount of solute that can be absorbed is directly dependent on the number of transport proteins available! Therefore, there is a Transport maximum (Tm= the maximum rate of transport when ALL carriers are being used) for various solutes. SEE FIGURE 19-15 Descending Loop of Henle 1. Lower surface area… 2. Still permeable to water A. Much water leaves… B. This is due to a crazy interstitial concentration gradient in the kidney’s medulla 3. Not permeable to solutes… A. No carrier proteins! (or VERY few!) Ascending Loop of Henle 1. (note: thin and thick ascending loops…) 2. Not permeable to water anymore! A. “Tight” tight junctions B. Covered in a glycoprotein that is impermeable to water 3. Lots of mitochondria 4. Very permeable to solutes…especially NaCl A. Na transported out of lumen (down conc grad), and other ions hitch a ride (2 Cl, 1 K) i. Cl- channels are open on the basolateral membrane allowing it to follow Na+ down its conc gradient… (no buildup of Cl) ii. Open K+ channels allow K+ to go down the conc gradient on both the luminal and basolateral sides! B. This makes cell more concentrated, but water can’t follow! C. Also has NaK pump on basolateral membrane…so Na+ gets pumped back OUT maintaining the conc. gradient! Bio 7: Human Physiology 61 Spring 2014: Riggs Distal Convoluted Tubule 1. 2. 3. 4. Similar to ALH! Carries dilute filtrate to the collecting duct Can reabsorb more solutes, creating very dilute urine (50 mOsm) Can also allow the reabsorption of water by inserting water pores into the membrane…this ability is dependent on hormonal control…(because the DCT is normally NOT permeable to water) Collecting Duct 1. 2. 3. 4. (Final site of urine modification before EXCRETION) Again, permeability of wall is VARIABLE and HORMONALLY CONTROLLED!!!! Hormones control permeability to water and urea… With hormonal input, the CD can reabsorb MORE water, creating a very concentrated urine (up to 1200 mOsm!)…How is this possible??? 5. 2 cell types line the CD: A. Intercalated cells i. Play a role in pH homeostasis ii. Reabsorb potassium ions and secrete H ions into the lumen… B. Principal cells i. Reabsorb Na+ and water from the lumen and secrete potassium into the lumen… ii. Respond to hormones and adjust reabsorption and secretion to create the perfect urine! Concentrating the urine 1. Countercurrent exchange mechanism: When 2 vessels flow by each other in opposite directions, allowing exchange over a “longer” length of vessel! 2. Countercurrent multiplier: When ACTIVE TRANSPORT enhances the exchange caused by a countercurrent mechanism (text 659) 3. The actions of the Loops of Henle actually establish a concentration gradient in the interstitial fluid. 4. Because the concentration gradient is enhanced by active transport of solutes OUT of the ALH, this is considered a COUNTERCURRENT MULTIPLIER Establishing the medullary concentration gradient 1. First, assume that the interstitial fluid started out ISOSMOTIC to the filtrate…which enters at about 300mOsm. 2. Next, remember that solutes are actively pumped OUT of the Ascending Loop of Henle. A. This will DECREASE concentration of the filtrate… B. This will also INCREASE concentration of the interstium. C. The only rule is this: The Na/K pump can ONLY establish a concentration difference of 200mOsm…no greater. This fact effectively “stops” the pump’s action when there is a difference of 200mOsm between the filtrate and the interstitial fluid. 3. The action of the Na/K pumps in the ALH create an increased osmolarity in the interstitial fluid…creating an osmotic gradient that draws WATER out of the DLH (effectively concentrating the filtrate in the DLH!) 4. When the filtrate moves, new concentration gradients are established, and the process repeats itself… Blood is still needed to fuel the nephron cells…why doesn’t the blood carry away the solutes, and eliminate the concentration gradient? The VASA RECTA is a COUNTERCURRENT EXCHANGER (Why is it considered an “exchanger” and not a “multiplier”?) 1. Vasa recta does not ESTABLISH the medullary concentration gradient…however, it HELPS MAINTAIN IT. (Med 350) 2. Hydrostatic pressure in vasa recta capillaries is 10mmHg! (compare to 55 mmHg in the glomerulus!) Fluid rushes back into the caps to return to circulation… 3. Because vasa recta flows COUNTERCURRENT to the filtrate, it can pick up the reabsorbed fluid/solute WITHOUT eliminating the medullary concentration gradient. A. Draw a picture of this to help you visualize it! Bio 7: Human Physiology 62 Spring 2014: Riggs External Brain 18: Kidneys Study Guide Questions 1. Distinguish between the following words: Filtration, Reabsorption, Secretion, Excretion 2. Be able to describe (or draw) the flow of blood through the nephron. 3. Know the function of the glomerulus, as well as all sections of the nephron tubule. 4. Understand how the structure of the glomerulus enables its unique function. 5. Explain the various pressures acting within the glomerulus that promote filtration. Compare these pressures to the pressures present in systemic capillaries where nutrient and waste exchange occurs. 6. Describe the cells that make up the proximal convoluted tubule. Include a clear explanation of how the cell’s unique features enable its unique action. 7. Distinguish between “luminal” or “apical” and “basolateral”. 8. What is the hydrostatic pressure in the peritubular capillaries? How does this promote reabsorption? 9. What is the transport maximum (Tm)? 10.Describe the relationship between filtration rate, reabsorption rate, excretion rate and renal threshold. Use Fig 19-15 as your guide. 11. Describe the cells that make up the descending loop of Henle. Include a clear explanation of how the cell’s unique features enable its unique action 12.Describe the cells that make up the ascending loop of Henle. Include a clear explanation of how the cell’s unique features enable its unique action. 13.What happens in the distal convoluted tubule? What are those cells like? 14.What happens in the collecting duct? 15.Describe the concept of “countercurrent exchange” found in the “countercurrent multiplier” in the descending and ascending loops of henle. (See pgs 659-661 in your text....) 16.Compare and contrast the countercurrent mechanism found in the loop of Henle to the one found in the vasa recta. 17.Compare and contrast the cells that make up the tubule walls in various locations of the nephron. Connect structure to function. 18.Be able to describe (or draw) the flow of filtrate (the fluid filtered out at the glomerulus) through the nephron. 19.Understand how the interstitial concentration gradient in the medulla of the kidney is established and maintained. Be able to list key features of involved cells. 20. Why is the medullary concentration gradient a key component in kidney function? 21.What is the hydrostatic pressure in the peritubular capillaries? How does this promote reabsorption? Bio 7: Human Physiology 63 Spring 2014: Riggs