* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Anatomy and myoarchitecture of the left ventricular wall in normal
Quantium Medical Cardiac Output wikipedia , lookup
Coronary artery disease wikipedia , lookup
Echocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Artificial heart valve wikipedia , lookup
Aortic stenosis wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Heart failure wikipedia , lookup
Jatene procedure wikipedia , lookup
Electrocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
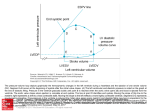
European Journal of Echocardiography (2009) 10, iii3–iii7 doi:10.1093/ejechocard/jep159 Anatomy and myoarchitecture of the left ventricular wall in normal and in disease Siew Yen Ho* Cardiac Morphology Unit, Imperial College London, Royal Brompton Hospital, London, UK KEYWORDS Anatomy; Myocardium; Myoarchitecture; Ventricular function The normal left ventricle comprises an inlet, apical trabecular, and an outlet portion although these portions do not have discrete anatomical borders. The ventricular wall is thickest near the cardiac base and thins to 1–2 mm at the apex. Characteristically, the muscle bundles at the apical portion are thin, but there are also thicker bundles and very fine strands that may be mistaken on imaging as pathologies. Transmurally through the ventricular wall, the myoarchitecture has a typical arrangement of myocardial strands that change orientation from being oblique in the subepicardium to circumferential in the middle and to longitudinal in the subendocardium. The circumferential portion is the thickest with the longitudinal portion the thinnest. In the hypertrophied ventricle the circumferential portion is reduced. In combination with alterations in the quality and quantity of the connective tissue matrix, myoarchitecture impacts on myocardial function. Introduction This review focuses on the myocardial component of the left ventricle, leaving aside the aortic and mitral valves. First, the muscular structures and normal variants within this chamber are described and then the potential misinterpretation of normal structures is discussed. Secondly, the orientation of the myocardial strands in the normal and abnormal left ventricle is reviewed together with a consideration of the connective tissue matrix of the myocardium. Anatomy of the left ventricle The normal left ventricle comprises an inlet portion containing the mitral valve apparatus, an outlet portion leading to the aortic valve, and an apical portion containing fine trabeculations (Figure 1). From a simplistic viewpoint, the shape of the left ventricle approximates to a cone with the right ventricle hugging it. Consequently, the septal component of the ventricular wall is curved. Thus, when the heart is viewed from the anterior aspect, most of the left ventricle is hidden by the right ventricle. Furthermore, the left ventricular outlet overlaps the inlet. Normally, the left ventricular free wall is thickest at the cardiac base and it gradually becomes thinner towards the apex. At the very tip of the ventricle, the musculature is only 1–2 mm thick, even in hypertrophied ventricles (Figure 2). The normal thickness at the obtuse margin of the left ventricle for an adult heart is 12–15 mm, excluding trabeculations, when * Correspondending author: Tel: þ44 207 351 8751, fax: þ44 207 351 8230. E-mail address: [email protected] measured approximately 1.5 cm below the mitral hingeline (annulus). The endocardial aspect of the ventricle is characterized by a criss-crossing meshwork of thin muscle bundles (trabeculations) at the apical third of the ventricle. Not infrequently, fine muscular strands or so-called false tendons extend between the septum and the papillary muscles or the parietal wall (Figure 2). Autopsy series of normal hearts have reported an incidence of 55 and 62%.1,2 On echocardiography they may be mistaken for ruptured chords of the valve apparatus or vegetations. In contrast, the outlet portion of the septum is relatively smooth whereas relatively thick muscle bundles line the anterosuperior, postero-inferior, and posterior walls (Figure 2). The latter, described as numbering three or fewer, are normal structures that when prominent may cause overdiagnosis of non-compaction of the left ventricular myocardium on echocardiography.3 The pathological entity of non-compaction cardiomyopathy, or spongy myocardium, is characterized by prominent and excessive trabeculations with correspondingly deep recesses in between within the hypertrophied wall.4,5 The left ventricular wall most frequently affected is the apical, mid-lateral, and mid-inferior portions.6–8 On heart specimens the affected segments have two components transmurally: a thin compact, or normal, layer in the subepicardium and a thicker subendocardial layer of trabeculations with deep recesses giving a thickness ratio of approximately 1:2. It remains unclear whether non-compaction is a distinct entity from hypertrabeculation where there are more than three prominent trabeculations and is often associated with extracardiac disorders.9 Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2009. For permissions please email: [email protected]. iii4 S.Y. Ho Figure 1 (A) and (B) Two parts of the same heart sectioned longitudinally. The broken lines divide the left ventricle into three portions. Note the cross-over relationship between right and left ventricular outflow tracts and the smooth upper part of the ventricular septum leading to the aorta. RVOT, right ventricular outflow tract The ventricular septum in the normal heart is curved, convexing into the right ventricular cavity. It is muscular except for a small portion immediately beneath the aortic valve which is a thin fibrous structure, the ventricular component of the membranous septum. Together with the right fibrous trigone, this thin component forms the central fibrous body that encases the atrioventricular conduction bundle and is an anatomical landmark for the emergence of the conduction bundle onto the crest of the muscular septum (Figure 2). Over the age of 60 years, there is an increase in angulation of the basal part of the muscular septum, producing a sigmoid appearance on imaging that can produce features of hypertrophic cardiomyopathy.10,11 The papillary muscles supporting the mitral valve are an integral component of the left ventricular wall. There are usually two groups of papillary muscles disposed in anterolateral and postero-medial locations of the left ventricle when the ventricle is seen in short-axis cuts. The anterolateral group is often a single pillar or base whereas there is a more variation in the posteromedial group (Figure 2). Each pillar may have one head or multiple heads into which the tendinous cords insert. Occasionally, there is muscularization of cords with the muscular tip inserting into the undersurface of the leaflet.12 The belly of the papillary muscle Figure 2 (A) The papillary muscles in the left ventricle, fine apical trabeculations, a long false tendon (green arrows), and broad muscle bundles (triangles). The asterisk marks the membranous septum. Note the thin musculature at the apex (arrow). (B) Simulated ‘four-chamber’ cut through a heart with a dilated left ventricle. The bases of the papillary muscles are continuous with the trabeculations. This heart shows multiple fine strands of false tendons crossing the cavity, and trabeculations also on the posterior and postero-inferior walls. AL, anterolateral papillary muscle; PM, postero-medial papillary muscle. may be finger-like or broad, long or short, or nearly sessile with very short free length. There may be multiple bellies that interlink or are arranged in two tiers.13 In between the two groups, there may be additional papillary muscles. Relating to the mural (posterior) leaflet of the mitral valve, there are basal cords that arise directly from the free wall or via small papillary muscles to insert to the under-side of the leaflet. All in all, the bases of the papillary Anatomy and myoarchitecture of the LV wall muscles are attached to the middle to apical thirds of the ventricular wall but there are wide variations. But, the basal parts of the papillary muscles are not solid muscle (Figure 2). Multidetector-row computed tomography imaging in recent years has provided a novel observation that the bases are attached to muscular trabeculations rather than directly to the compact myocardium.14 The myocardium The bulk of the myocardium is formed by the contractile cardiac myocytes. The adult myocyte is usually 120 mm long and 20–30 mm in diameter. The ends of each myocyte branches and adjoin adjacent myocytes to produce a complex three-dimensional network, or syncytium, of anastomosing fibres. In any attempt to relate structure to function, however, one should not ignore the network of interstitial connective tissue (Figure 3A). A fine network of fibrocollagenous connective tissue, the endomysium, surrounds each myocyte providing it with the supportive frame work. The endomysial weave coordinate the transmission of force and prevent slippage between cells. A network of thicker connective tissue surrounds groups of myocytes. Known as the perimysium, this weave bears the shearing forces between groups of cardiomyocytes and its lateral strands prevent malalignment between bundles.15 Abnormal accumulation and/or change in the quality of the connective tissue increases myocardial stiffness.16 iii5 Ventricular myoarchitecture Myoarchitecture has been and remains a contentious issue right from the early days. Indeed, Keith,17 in his Harveian lecture in 1918, commented that such meticulous work was dismissed by Hunter in the phrase ‘Much more pains than were necessary have been taken to dissect and describe the course and arrangement of the muscular fibres of the heart’. Based on investigation techniques, some argue that there are discrete systems of myocyte arrangements in each ventricle while others are insistent of a single rope-like configuration that encompasses both ventricles.18–20 Even in more recent years, using advanced reconstruction techniques and imaging tools there is much discussion on this subject.21–23 Despite obvious limitations of gross dissections, the myocardial strands (previously termed myocardial or muscle fibres) that are revealed using this basic technique provide a guide to the general longitudinal orientation of the myocytes and serve as an overview of myocyte arrangement, the myoarchitecture.24–27 Normal left ventricle On gross dissection, the left ventricular wall comprises three ‘layers’ according to the longitudinal alignment of the myocardial strands: superficial (subepicardial), middle, and deep (subendocardial). Importantly, these ‘layers’ represent changes in orientation of the myocardial strands transmurally. They are not separated by cleavage planes or sheets Figure 3 (A) Diagram showing the network like arrangement of the connective tissue matrix around individual myocytes and groups of myocytes. (B) The diagrams are of the frontal aspect of a heart rotated so as to show more of the left ventricle. They depict the orientation of the myocardial strands from subepicardium to subendocardium. The superficial strands are oblique, middle strands are circumferential, while deep strands are longitudinal. The circumferential portion is thickest in the normal heart. LV, left ventricle; RV, right ventricle. iii6 of fibrous tissue since strands of one ‘layer’ interconnect with strands of the next ‘layer’ in a continuum. When traced from the base to the apex, the superficial layer extends from one ventricle to the other (Figure 3B). The myocardial strands arise from the insertions of the cardiac valves at the cardiac base. The superficial strands on the sternocostal aspect run obliquely crossing the interventricular groove, sweep leftward over the obtuse margin and descend towards the cardiac apex. The strands arising from the mitral insertions continue to the diaphragmatic aspect rightward where they cross the inferior (posterior) interventricular groove. At the obtuse margin, they are at an angle of 10–208 to the long axis of the left ventricular inlet.26 The superficial ‘layer’ occupies approximately 25% of the wall thickness.28 At the vortex of the left ventricle, the myocardial strands invaginate in a spiral pattern to give rise to the subendocardial ‘layer’. There is a similar continuity between superficial and deep ‘layers’ at the base of the ventricle. The middle ‘layer’ occupies approximately 53–59% of the ventricular wall thickness. It is thicker in the elderly.29 The myocardial strands are more circumferentially arranged, nearly parallel to the plane of the mitral orifice (Figure 3B). They do not insert into the mitral or aortic valves, nor to the ventricular apex. This layer is thickest near the base, thinning out towards the cardiac apex. At the base, it encircles the inlet together with the outlet portions. From the apex of the left ventricle, the deep ‘layer’ of myocardial strands radiate in longitudinal fashion in the subendocardium, to insert into the aortic and mitral valves and the membranous septum (Figure 3B). They fuse with the trabeculations and broader muscle bundles that line the ventricular cavity, and also continue into the papillary muscles. Consequently, the deep myocardial strands form a meshwork determined by the trabeculations at the apical third, muscle bundles on the middle, and the valvar insertion at the basal third. This is the thinnest ‘layer’, accounting for ,20% of the wall thickness.28 The myoarchitecture of the ventricular septum reflects the parietal wall of both right and left ventricles, the major contribution coming from the middle ‘layer’ of the left ventricle except at the apical portion where the middle ‘layer’ is lacking. Abnormal left ventricle There are only a few anatomical studies on abnormal myoarchitecture. A study comparing hearts from normal patients with hearts from patients with history of hypertension without clinical heart failure, and patients with both ventricular overload and congestive failure showed the orientation of the myocardial strands is not altered. Instead, there was an increase in connective tissue content with the greatest increase in the failing heart.30 Another study, an experimental study on dogs in which histological sections were sampled only at the equator of the left ventricle revealed the myoarchitecture in the pressure, volume, and exercise-overloaded hearts, was remarkably similar to normals.31 However, these investigators reported an increase in the proportion of longitudinally aligned strands in the subepicardial and subendocardial regions of the wall thickness, with corresponding decrease of circumferential strands in the middle. S.Y. Ho Figure 4 (A) Reduced left ventricular cavity in a heart with hypertrophic cardiomyopathy. (B) Histological section showing myocyte disarray (red) and fibrosis (green). Masson’s trichrome stain. The ‘classical’ heart with hypertrophic cardiomyopathy presents with asymmetric thickening of the ventricular septum, with endocardial thickening representing mitral impact lesion in approximately a third of cases at autopsy. Septal thickening can exceed twice that of the parietal wall. Many hearts with hypertrophic cardiomyopathy, however, show symmetric hypertrophy presenting with an evenly thick-walled left ventricle and a reduced cavity (Figure 4). Cross-sectional slices often display a macroscopic whorl-like appearance reflecting a combination of myocyte disarray and fibrosis. Mid-ventricular cross sections of human heart specimens with hypertrophic cardiomyopathy were sampled in the study by Kuribayashi and Roberts.32 They reported extensive loss of the circular orientation of myocardial strands and deep endocardial clefts in the junctional regions of the parietal wall with the septum. The affected regions showed marked disarray and usually, but not always, accompanied by increased interstitial and focal fibrosis. There is an increase in the thickness of the longitudinal deep ‘layer’, an observation also reported in a study carried out using cardiac diffusion and strain magnetic resonance imaging.33 It is known that the connective tissue matrix supporting the myocardium is altered in disease.34 In the hypertrophied heart, there is an increase in the diameter of the perimysial tendons and density of the weave leading to a loss of intercellular contact and conductivity.16,35 In contrast, the cross connections are lost in dilated cardiomyopathy resulting in slippage and realignment of adjacent bundles of myocytes and wall thinning. Anatomy and myoarchitecture of the LV wall Conclusions The normal left ventricular wall has characteristic muscle bundles and myoarchitecture. The myoarchitecture may be altered in ventricular hypertrophy by fibre disarray and/or increased proportion of longitudinally orientated myocardial strands. Myoarchitecture in combination with alterations in the connective tissue matrix provide the structural basis for abnormalities in myocardial function. Conflict of interest: none declared. Funding The Cardiac Morphology Unit at the Royal Brompton Hospital receives funding support from the Royal Brompton and Harefield Hospital Charitable Fund. References 1. Luetmer PH, Edwards WD, Seward JB, Tajik AJ. Incidence and distribution of left ventricular false tendons: an autopsy study of 483 normal human hearts. J Am Coll Cardiol 1986;8:179–183 2. Loukas M, Louis RG Jr, Black B, Pham D, Fudalej M, Sharkees M. False tendons: an endoscopic cadaveric approach. Clin Anat 2007;20:163–169. 3. Boyd MT, Seward JB, Tajik AJ, Edwards WD. Frequency and location of prominent left ventricular trabeculations at autopsy in 474 normal human hearts: implications for evaluation of mural thrombi by twodimensional echocardiography. J Am Coll Cardiol 1987;9:323–326. 4. Ritter M, Oechslin E, Sütsch G, Attenhofer C, Schneider J, Jenni R. Isolated noncompaction of the myocardium in adults. Mayo Clin Proc 1997;72:26–31. 5. Agmon Y, Connolly HM, Olson LJ, Khandheria BK, Seward JB. Noncompaction of the ventricular myocardium. J Am Soc Echocardiogr 1999;12: 859–863 6. Jenni R, Oechslin EN, van der Loo B. Isolated ventricular non-compaction of the myocardium in adults. Heart 2007;93:11–15 7. Sengupta PP, Mohan JC, Mehta V, Jain V, Arora R, Pandian NG, Khandheria BK. Comparison of echocardiographic features of noncompaction of the left ventricle in adults versus idiopathic dilated cardiomyopathy in adults. Am J Cardiol 2004;94:389–91. 8. Ichida F, Hamamichi Y, Miyawaki T, Ono Y, Kamiya T, Akagi T, Hamada H, Hirose O, Isobe T, Yamada K, Kurotobi S, Mito H, Miyake T, Murakami Y, Nishi T, Shinohara M, Seguchi M, Tashiro S, Tomimatsu H. Clinical features of isolated noncompaction of the ventricular myocardium: long-term clinical course, hemodynamic properties, and genetic background. J Am Coll Cardiol 1999;34:233–40. 9. Stöllberger C, Finsterer J. Left ventricular hypertrabeculation/noncompaction. J Am Soc Echocardiogr 2004;17:91–100. 10. Kitzman DW, Scholz DG, Hagen PT, Ilstrup DM, Edwards WD. Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity): a quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin Proc 1988;63:137–46. 11. Kitzman DW, Edwards WD. Age-related changes in the anatomy of the normal human heart. J Gerontol 1990;45:M33–9. iii7 12. Lam JH, Ranganathan N, Wigle ED, Silver MD. Morphology of the human mitral valve. I. Chordae tendineae: a new classification. Circulation 1970;41:449–58. 13. Victor S, Nayak VM. Variations in the papillary muscles of the normal mitral valve and their surgical relevance. J Card Surg 1995;10:597–607. 14. Axel L. Papillary muscles do not attach directly to the solid heart wall. Circulation 2004;109:3145–8. 15. Caulfield JB, Borg TK. The collagen network of the heart. Lab Invest 1979;40:364–72. 16. Weber KT, Brilla CG, Janicki JS. Myocardial fibrosis: functional significance and regulatory factors. Cardiovasc Res 1993;27:341–348. 17. Keith A. Harveian lecture on the functional anatomy of the heart. Br Med J 1918;1:361–3. 18. Mall FP. On the muscular architecture of the ventricles of the human heart. Am J Anat 1911;11:211–66. 19. Grant PP. Notes on the muscular architecture of the left ventricle. Circulation 1965;32:301–8 20. Torrent-Guasp F, Buckberg GD, Clemente C, Cox JL, Coghlan HC, Gharib M. The structure and function of the helical heart and its buttress wrapping. I. The normal macroscopic structure of the heart. Semin Thorac Cardiovasc Surg 2001;13:301–19. 21. Lunkenheimer PP, Redmann K, Kling N, Jiang X, Rothaus K, Cryer CW, Wübbeling F, Niederer P, Heitz PU, Ho SY, Anderson RH. Threedimensional architecture of the left ventricular myocardium. Anat Rec A Discov Mol Cell Evol Biol 2006;288:565–78. 22. Wu EX, Wu Y, Tang H, Wang J, Yang J, Ng MC, Yang ES, Chan CW, Zhu S, Lau CP, Tse HF. Study of myocardial fiber pathway using magnetic resonance diffusion tensor imaging. Magn Reson Imaging 2007;25:1048–57. 23. Buckberg GD. Architecture must document functional evidence to explain the living rhythm. Eur J Cardiothorac Surg 2005;27:202–9. 24. McLean M, Prothero J. Determination of relative fiber orientation in heart muscle: methodological problems. Anat Rec 1992;232:459–65. 25. Lev M, Simkins CS. Architecture of the human ventricular myocardium. Lab Invest 1956;5:396–409. 26. Greenbaum R, Ho SY, Gibson DG, Becker AE, Anderson RH. Left ventricular fibre architecture in man. Br Heart J 1981;54:248–63. 27. Fernandez-Teran MA, Hrule JM. Myocardial fiber architecture of the human heart. Anat Rec 1982;204:137–47. 28. Sanchez-Quintana D, Climent V, Ho SY, Anderson RH. Myoarchitecture and connective tissue in hearts with tricuspid atresia. Heart 1999;81:182–91. 29. Sanchez-Quintana D, Garcia-Martinez V, Climent V, Hurle JM. Morphological changes in the normal pattern of ventricular myoarchitecture in the developing human heart. Anat Rec 1995;243:483–95. 30. Pearlman ES, Weber KT, Janicki JS. Quantitative histology of the hypertrophied human heart. Fed Proc 1981;40:2042–7. 31. Carew TE, Covell JW. Fiber orientation in hypertrophied canine left ventricle. Am J Physiol 1979;236:H487–93. 32. Kuribayashi T, Roberts WC. Myocardial disarray at junction of ventricular septum and left and right ventricular free walls in hypertrophic cardiomyopathy. Am J Cardiol 1992;70:1333–40. 33. Tseng WY, Dou J, Reese TG, Wedeen VJ. Imaging myocardial fiber disarray and intramural strain hypokinesis in hypertrophic cardiomyopathy with MRI. J Magn Reson Imaging 2006;23:1–8. 34. Weber KT. Cardiac interstitium in health and disease: the fibrillar collagen network. J Am Coll Cardiol 1989;13:1637–1652. 35. Weber KT, Janicki JS, Shroff SG. Collagen compartment remodelling in the pressure overloaded left ventricle. J Appl Cardiol 1988;1:37–46.