* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ch 11 The Heart
History of invasive and interventional cardiology wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Aortic stenosis wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Artificial heart valve wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
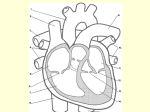
Chapter 11 The Cardiovascular System The Cardiovascular System A closed system of the heart and blood vessels -heart pumps blood -blood vessels - circulate to all parts of body Deliver oxygens & nutrients and to remove carbon dioxide & waste products The Heart In thorax between lungs Pointed apex toward left hip Size of fist Figure 18.1a Location of the heart in the mediastinum. Midsternal line 2nd rib Sternum Diaphragm (a) Copyright © 2010 Pearson Education, Inc. Point of maximal intensity (PMI) Heart Coverings & Wall Layers Pericardium – double Three layers serous membrane Visceral - next to heart Parietal - 1.Epicardium- Outside visceral pericardium Connective tissue outside layer 2.Myocardium- Middle Serous fluid fills space between the layers Mostly cardiac muscle 3.Endocardium - Inner Endothelium Figure 18.2 The pericardial layers and layers of the heart wall. Pulmonary trunk Pericardium Myocardium Copyright © 2010 Pearson Education, Inc. Fibrous pericardium Parietal layer of serous pericardium Pericardial cavity Epicardium (visceral layer Heart of serous wall pericardium) Myocardium Endocardium Heart chamber External Heart Anatomy Figure 11.2a The Heart: Chambers Right and left act as separate pumps Four chambers 2 Atria - Receiving - Right atrium - Left atrium 2 Ventricles - Discharging - Right ventricle - Left ventricle Septum - divides the right from left side of the heart. Figure 18.6 Anatomical differences between the right and left ventricles. Left ventricle Right ventricle Interventricular septum Copyright © 2010 Pearson Education, Inc. The Heart: Associated Great Vessels Aorta - Leaves left ventricle Pulmonary arteries - Leave right ventricle Vena cava - Enters right atrium Pulmonary veins (four) - Enter left atrium The Heart: Valves Allow blood to flow in only one direction Four valves 2 Atrioventricular valves – between atria & ventricles Bicuspid valve (left) Tricuspid valve (right) 2 Semilunar valves - between ventricle & artery Pulmonary semilunar valve Aortic semilunar valve Held in place by chordae tendineae (“heart strings”) Pulmonary valve Aortic valve Area of cutaway Mitral valve Tricuspid valve Myocardium Tricuspid (right atrioventricular) valve Mitral (left atrioventricular) valve Aortic valve Fibrous skeleton (a) Copyright © 2010 Pearson Education, Inc. Pulmonary valve Anterior Figure 18.8b Heart valves. Myocardium Tricuspid (right atrioventricular) valve Mitral (left atrioventricular) valve Aortic valve Pulmonary valve Pulmonary valve Aortic valve Area of cutaway Mitral valve Tricuspid valve Copyright © 2010 Pearson Education, Inc. (b) Figure 18.8c Heart valves. Chordae tendineae attached to tricuspid valve flap (c) Copyright © 2010 Pearson Education, Inc. Papillary muscle Pulmonary valve Aortic valve Area of cutaway Mitral valve Tricuspid valve Opening of inferior vena cava Tricuspid valve Mitral valve Chordae tendineae Myocardium of right ventricle Myocardium of left ventricle Papillary muscles (d) Copyright © 2010 Pearson Education, Inc. Interventricular septum Pulmonary valve Aortic valve Area of cutaway Mitral valve Tricuspid valve Operation of Heart Valves 1 Blood returning to the 2 As ventricles fill, 3 Atria contract, forcing heart fills atria, putting pressure against atrioventricular valves; atrioventricular valves are forced open. atrioventricular valve flaps hang limply into ventricles. additional blood into ventricles. Direction of blood flow Atrium Cusp of atrioventricular valve (open) Chordae tendineae Ventricle Papillary muscle (a) AV valves open; atrial pressure greater than ventricular pressure Copyright © 2010 Pearson Education, Inc. 1 Ventricles contract, forcing blood against atrioventricular valve cusps. 2 Atrioventricular valves close. Atrium Cusps of atrioventricular valve (closed) Blood in ventricle 3 Papillary muscles contract and chordae tendineae tighten, preventing valve flaps from everting into atria. (b) AV valves closed; atrial pressure less than ventricular pressure Copyright © 2010 Pearson Education, Inc. Figure 18.10a The semilunar valves. Aorta Pulmonary trunk As ventricles contract and intraventricular pressure rises, blood is pushed up against semilunar valves, forcing them open. (a) Semilunar valves open Copyright © 2010 Pearson Education, Inc. Figure 18.10b The semilunar valves. As ventricles relax and intraventricular pressure falls, blood flows back from arteries, filling the cusps of semilunar valves and forcing them to close. (b) Semilunar valves closed Copyright © 2010 Pearson Education, Inc. Pathway of Blood Through the Heart • Right atrium tricuspid valve right ventricle • Right ventricle pulmonary semilunar valve pulmonary trunk pulmonary arteries lungs PLAY Animation: Rotatable heart (sectioned) Pathway of Blood Through the Heart • Lungs pulmonary veins left atrium • Left atrium bicuspid valve left ventricle • Left ventricle aortic semilunar valve aorta • Aorta systemic circulation PLAY Animation: Rotatable heart (sectioned) Figure 18.19 Aortic Areasvalve of sounds the thoracic surface heard in 2nd intercostal space at where the heart can be best detected. rightsounds sternal margin Pulmonary valve sounds heard in 2nd intercostal space at left sternal margin Mitral valve sounds heard over heart apex (in 5th intercostal space) in line with middle of clavicle Tricuspid valve sounds typically heard in right sternal margin of 5th intercostal space Copyright © 2010 Pearson Education, Inc. • Mitral Regurgitation • Aortic Stenosis Current Event • Causes of elevated cholesterol levels in our blood and typical medical methods to reduce high cholesterol. Then focus on if/how hypercholesterolemia can be controlled without the use of drugs. Be very specific about how it can be done if it is possible. Coronary Circulation Blood in heart doesn’t nourish the heart Heart’s nourishing circulatory system - Coronary arteries - Come off the aorta - Cardiac veins - Blood empties into the right atrium via the coronary sinus Figure 18.7a Coronary circulation. Aorta Superior vena cava Anastomosis (junction of vessels) Right atrium Pulmonary trunk Left atrium Left coronary artery Circumflex artery Right coronary artery Left ventricle Right ventricle Anterior Right interventricular artery marginal Posterior artery interventricular artery (a) The major coronary arteries Copyright © 2010 Pearson Education, Inc. Figure 18.7b Coronary circulation. Superior vena cava Anterior cardiac veins Great cardiac vein Coronary sinus Small cardiac vein Middle cardiac vein (b) The major cardiac veins Copyright © 2010 Pearson Education, Inc. Coronary Circulation Pattern Aorta Coronary Arteries Myocardium Coronary Circulation Pattern Aorta Coronary Arteries Myocardium Cardiac Veins Coronary Sinus Right Atrium •Collateral Circulation • Most organs receive blood from more than one arterial branch. • Arterial anastomosis - where arteries supplying the same area join. • Embolism • Angina pectoris • Myocardial Infarction (MI) • Coronary bypass surgery • Open Heart Surgery • Coronary artery disease (Adam) • Atherosclerosis Heart Dissection (Lab Manual pg 306) • Heart Dissection I • Heart Dissection II The Heart: Cardiac Cycle Cardiac cycle – events of one heart beat Terms: Systole = contraction Atria contract simultaneously Atria relax, then ventricles contract Diastole = relaxation Phases of the Cardiac Cycle 1. Ventricular filling—takes place in mid-to-late diastole • AV valves are open • 80% of blood passively flows into ventricles • Atria contract occurs, delivering the remaining 20% Phases of the Cardiac Cycle 2. Ventricular systole • Atria relax and ventricles begin to contract • Rising ventricular pressure results in closing of AV valves • In ejection phase, ventricular pressure exceeds pressure in the large arteries, forcing the SL valves open Phases of the Cardiac Cycle 3. Early diastole • Ventricles relax • Backflow of blood in aorta and pulmonary trunk closes SL valves. The Heart: Conduction System Intrinsic conduction system (nodal system) Heart muscle cells contract, without nerve impulses, in a regular, continuous way - Sinoatrial node – Pacemaker initiates contraction - Sequential stimulation occurs at other autorhythmic cells - Atrioventricular node - Atrioventricular bundle - Bundle branches - Purkinje fibers • Heart rate controlled by its own internal control center. The SA Node (known as the pacemaker, 75/min) is located in the wall of the right atrium and sends out signals that cause the atria to contract. • These signals also travel to the AV Node (50/min) located in the septum between the atria, which relays the signals to the ventricles via the bundle of His (30/min) and Purkinje fibers causing them to contract. Animation Figure 18.14 Cardiac intrinsic conduction system and action potential succession during one heartbeat. Superior vena cava Right atrium 1 The sinoatrial Pacemaker potential (SA) node (pacemaker) generates impulses. Internodal pathway 2 The impulses SA node Left atrium pause (0.1 s) at the atrioventricular (AV) node. 3 The atrioventricular (AV) bundle connects the atria to the ventricles. 4 The bundle branches conduct the impulses through the interventricular septum. 5 The Purkinje fibers depolarize the contractile cells of both ventricles. (a) Anatomy of the intrinsic conduction system showing the sequence of electrical excitation Copyright © 2010 Pearson Education, Inc. Atrial muscle Purkinje fibers AV node Interventricular septum Ventricular muscle Pacemaker potential Plateau Milliseconds (b) Comparison of action potential shape at various locations Extrinsic Innervation of the Heart • Heartbeat is modified by the ANS • Cardiac centers are located in the medulla oblongata • Cardioacceleratory center innervates SA and AV nodes, heart muscle, and coronary arteries through sympathetic neurons • Cardioinhibitory center inhibits SA and AV nodes through parasympathetic fibers in the vagus nerves Figure 18.15 Autonomic innervation of the heart. The vagus nerve (parasympathetic) decreases heart rate. Dorsal motor nucleus of vagus Cardioinhibitory center Medulla oblongata Cardioacceleratory center Sympathetic trunk ganglion Thoracic spinal cord Sympathetic trunk Sympathetic cardiac nerves increase heart rate and force of contraction. SA node Copyright © 2010 Pearson Education, Inc. AV node Parasympathetic fibers Sympathetic fibers Interneurons Homeostatic Imbalances • Defects in the intrinsic conduction system may result in 1. Arrhythmias: irregular heart rhythms 2. Fibrillation: rapid, irregular contractions; useless for pumping blood Homeostatic Imbalances • Defective SA node may result in • Ectopic focus: abnormal pacemaker takes over • If AV node takes over, there will be a junctional rhythm (40–60 bpm) • Defective AV node may result in • Partial or total heart block • Few or no impulses from SA node reach the ventricles • Electrocardiogram • A graphic record of the hearts electrical activity. • 3 characteristic waves called the P wave, QRS complex, and the T wave. Figure 18.16 An electrocardiogram tracing (lead I). QRS complex Sinoatrial node Atrial depolarization Ventricular depolarization Ventricular repolarization Atrioventricular node P-Q Interval S-T Segment Q-T Interval Copyright © 2010 Pearson Education, Inc. Figure 18.17 The sequence of depolarization and repolarization of the heart related to the deflection waves of an ECG tracing. SA node Depolarization R Repolarization R T P Q S 1 Atrial depolarization, initiated by the SA node, causes the P wave. R AV node T P Q S 4 Ventricular depolarization is complete. R T P T P Q S 2 With atrial depolarization complete, the impulse is delayed at the AV node. R Q S 5 Ventricular repolarization begins at apex, causing the T wave. R T P T P Q S 3 Ventricular depolarization begins at apex, causing the QRS complex. Atrial repolarization occurs. Copyright © 2010 Pearson Education, Inc. Q S 6 Ventricular repolarization is complete. Figure 18.18 Normal and abnormal ECG tracings. (a) Normal sinus rhythm. (c) (b) Junctional rhythm. The SA node is nonfunctional, P waves are absent, and heart is paced by the AV node at 40 - 60 beats/min. Second-degree heart block. (d) Ventricular fibrillation. These chaotic, grossly irregular ECG Some P waves are not conducted deflections are seen in acute through the AV node; hence more heart attack and electrical shock. P than QRS waves are seen. In this tracing, the ratio of P waves to QRS waves is mostly 2:1. Copyright © 2010 Pearson Education, Inc. Animation • Depolarization describes the electrical activity just before contraction. • Repolarization begins just before the relaxation phase. • P wave is depolarization of the atria. • QRS complex is depolarization of the ventricles. • T wave is repolarization of the vetricles. • Repolarization of atria is hidden by the QRS complex. The Heart: Cardiac Output Cardiac output (CO) Amount of blood pumped by each side of the heart in one minute CO = (heart rate [HR]) x (stroke volume [SV]) Stroke volume [SV] Volume of blood pumped by each ventricle in one contraction The Heart: Regulation of Heart Rate Stroke volume usually remains relatively constant - Starling’s law of the heart: the more that the cardiac muscle is stretched, the stronger the contraction Changing heart rate is the most common way to change cardiac output Regulation of Heart Rate Increased Heart Rate Decreased Heart Rate 1. Sympathetic nervous system Crisis Low blood pressure 2. Hormones Epinephrine Thyroxine 3. Exercise 4. Decreased blood volume 1. Parasympathetic nervous system 2. High blood pressure or blood volume 3. Decreased venous return