* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download AANA Journal Course 3: Aortic stenosis: A review
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Turner syndrome wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Artificial heart valve wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Rheumatic fever wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
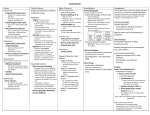
3 AANA Journal Course Update for nurse anesthetists 6 CE Credits* Aortic stenosis: A review David Phillips, CRNA, MSN Wake Forest, North Carolina 2005 Student Writing Contest Honorable Mention The prevalence of aortic stenosis has been increasing in recent decades, and nurse anesthetists are more likely to encounter this problem as the population ages. Fortunately, the widespread use of echocardiography has expanded our understanding of valvular heart disease. The purpose of this course is to evaluate the current literature regarding aortic stenosis with a focus on anesthetic management. The 2 most common causes of aortic stenosis are calcific tricuspid disease and congenital bicuspid valves. An inflammatory, atherosclerotic disease process also has been identified in aortic stenosis. Patients with aortic stenosis are at high risk for perioperative cardiac complications. Anesthetic management often includes invasive hemodynamic monitoring and carefully tailored anesthetic techniques. Objectives AVR surgeries, constituting 72% of all valve replacements that year.2 These trends suggest that anesthesia providers are increasingly likely to care for these patients during cardiac and noncardiac surgery. Few cardiovascular diseases present more of a challenge to anesthesia professionals than aortic stenosis (AS). People who live with this disease often have little or no cardiac reserve, and they may not tolerate the stress response associated with surgery. Likewise, most anesthetic techniques produce hemodynamic changes that can be disastrous in the presence of significant AS. It is estimated that 2% of elderly Americans have AS.1 The prevalence has risen in recent decades because of a growing elderly population and improved diagnostic techniques. The number of patients with a diagnosis of AS and the number of aortic valve replacement (AVR) surgeries has climbed steadily since 1990 (Figure 1).2 In 2002, there were 56,000 Diagnoses AVR 100 400 80 300 60 200 40 AVR (in thousands ) Introduction Figure 1. Increasing prevalence of aortic stenosis (AS) Diagnoses (in thousands ) At the conclusion of this course, the reader should be able to: 1. List the most common causes of aortic stenosis. 2. Describe the pathophysiology of aortic stenosis. 3. Differentiate mild, moderate, and severe aortic stenosis. 4. Explain the significance of aortic stenosis in patients undergoing noncardiac surgery. 5. Discuss the anesthetic management of patients with aortic stenosis. Key words: Anesthesia, anesthetic management, aortic stenosis, noncardiac surgery, risk. 100 20 0 0 90 92 994 996 998 000 002 2 1 1 19 19 2 1 Year The number of patients discharged from hospitals with a diagnosis of nonrheumatic AS and the number of patients undergoing aortic valve 2 replacement (AVR). Data from the National Center for Health Statistics. * AANA Journal Course No. 26: The American Association of Nurse Anesthetists is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center Commission on Accreditation. The AANA Journal course will consist of 6 successive articles, each with objectives for the reader and sources for additional reading. At the conclusion of the 6-part series, a final examination will be printed in the AANA Journal. Successful completion will yield the participant 6 CE credits (6 contact hours), code number: 28327, expiration date: July 31, 2007. www.aana.com/aanajournal.aspx AANA Journal/August 2006/Vol. 74, No. 4 309 Causes Rheumatic heart disease was the primary cause of AS in the United States before 1950. The widespread use of penicillin and improved diagnostic criteria have led to a decline in the prevalence of rheumatic AS.3 During the same period, calcification of a tricuspid aortic valve emerged as a major cause of AS.3 This condition is associated with advanced age and is more prevalent now simply because people are living longer. A pathologic study of surgically removed valves demonstrated that the 2 most common cases of AS in the United States are calcification of tricuspid valves and congenital bicuspid valves (Figure 2).3 An estimated 1% to 2% of the general population is born with a bicuspid aortic valve.4 Most people with bicuspid aortic valves develop calcific changes by late middle age that require valve replacement by the seventh decade of life.5 Figure 2. Causes of aortic stenosis* Calcific bicuspid 36% Calcific tricuspid 51% Other 4% Rheumatic 9% * Data from Dare et al. 3 Pathogenesis Calcific tricuspid AS traditionally was thought to result from “wear and tear” of the valve that progressively worsened with age, thus the label “degenerative” or “senile” AS. It now is recognized that calcific AS involves an inflammatory, atherosclerotic process similar to that in coronary artery disease.4 The risk factors for calcific AS are remarkably similar to those of atherosclerotic disease and include increased age, male gender, height, smoking, hypertension, diabetes mellitus, high low-density lipoprotein levels, and low high-density lipoprotein levels.1,6 Indeed, people with AS have a high prevalence of coronary artery disease and peripheral arterial disease.7,8 Several series report similar immunohistological changes in the lesions of atherosclerotic disease and calcific AS.9,10 The initial injury in AS results from mechanical stress that disrupts the valvular endothelial basement membrane. This disruption promotes lipid accumulation, infiltration of macrophages and T lymphocytes, and, finally, calcification. Therefore, calcific AS is not merely a degenerative process but rather an active and potentially modifiable disease process. Bicuspid valves have 1 less cusp to share the workload and are prone to stenosis because of the greater mechanical stress. After the initial injury, the same inflammatory changes that take place in tricuspid stenosis are seen in bicuspid valves.11 However, calcification of a bicuspid valve occurs more rapidly and requires surgical replacement at an average of a decade earlier than in tricuspid stenosis.5 Rheumatic heart disease remains a significant cause of AS in the United States. This disease is initiated by a pharyngeal infection with group A streptococci. Susceptible individuals seem to develop an autoimmune 310 AANA Journal/August 2006/Vol. 74, No. 4 process that results in fibrosis of the cusps, fusion of the commissures, and calcification. Rheumatic AS is almost always seen with mitral stenosis.4 Pathophysiology All of the common causes of AS eventually result in calcification, regardless of the initial cause. Calcification of the cusps on the aortic side of the valve (Figure 3) impedes opening of the valve during systole. A reduced valve area produces an obstruction to left ventricular outflow. To maintain a normal stroke volume, the left ventricle compensates with concentric hypertrophy, a process in which the myocardium thickens without enlargement of the ventricular cavity. The myocardium hypertrophies over many years as the obstruction becomes more severe.4 The thick myocardium produces sufficiently high left ventricular pressures when contracting to force blood past the valvular obstruction. A pressure gradient results between the left ventricle and the ascending aorta during systole and frequently is reported on echocardiogram and catheterization reports. The ventricular hypertrophy maintains normal wall stress despite the increased pressure load on the left ventricle. As a result, contractility is preserved until late in the disease process when the obstruction becomes so severe that the pressure load overwhelms the ability of the ventricles to compensate. The left ventricle is the end organ affected in AS.4 Diastolic dysfunction can occur earlier in the disease process. The left ventricle becomes less compliant. Ventricular filling is impaired due to poor diastolic relaxation and becomes increasingly reliant on www.aana.com/aanajournal.aspx Figure 3. Calcific aortic stenosis Table 1. Aortic stenosis severity* 2 Severity Valve area (cm ) Normal 3-4 Mild >1.5 Moderate 1.0-1.5 Severe <1.0 15 * Data from Bonow et al. Diagnosis A tricuspid aortic valve with large calcium nodules (black arrow), unfused commissures (white arrow), and a small valve area. left atrial contraction to fill. Left ventricular end-diastolic pressures often are elevated. Left atrial enlargement and pulmonary hypertension can result.4 In a person with asymptomatic AS, cardiac output can increase in response to stresses through an increase in heart rate but not through an increase in stroke volume. When the heart rate accelerates, there is a decreased systolic period during which stroke volume is maintained by an increase in the pressure gradient, an increased flow rate through the aortic valve, and a slight increase in valve area. However, when the stenosis becomes severe, the leaflets become more rigid and stroke volume cannot be maintained when the heart rate increases. The person becomes symptomatic with activity or stress. Heart failure is the end result.4 Clinical manifestations The classic triad of symptoms for AS are dyspnea, angina, and syncope. Exertional dyspnea is the most common initial symptom and is a sign of impending left ventricular failure. Angina is seen even in the absence of coexisting coronary artery disease. Coronary flow is inadequate to meet the increased demands of the hypertrophied left ventricle. Exertional syncope is a symptom specific to AS and helps rule out other valvular disorders. In a prospective study that looked at 397 patients (95% were symptomatic), the incidence of symptoms were as follows: dyspnea, 63%; angina, 51%; syncope, 42%; and other, 13%.12 www.aana.com/aanajournal.aspx Aortic stenosis usually is detected during physical examination by the presence of a grade 3 or 4 systolic murmur that is heard over the right second intercostal space. Other specific findings include a late peaking of the murmur and a significant delay and decrease in the carotid upstroke.13 These are useful screening tools in asymptomatic patients; however, echocardiography is the “gold standard” for confirming the diagnosis and determining the severity of stenosis. Echocardiography is noninvasive and cost-effective compared with cardiac catheterization, and it provides superior information on the morphologic features and motion of the aortic valve.14 The aortic valve area and the aortic pressure gradient are the 2 most commonly used determinants of stenosis severity. These parameters can be measured with echocardiography and cardiac catheterization. Severe AS is categorized as a valve area less than 1 cm2 (Table 1) and a pressure gradient of more than 50 mm Hg.15 Most patients with a valve area less than 0.5 cm2 have severe hemodynamic alterations and can have pressure gradients of more than 100 mm Hg.12 Disease course This disease begins with a latent period that extends over several decades. Outcome remains good in the absence of symptoms, with few cardiac deaths reported.16 The hemodynamic progression of the disease is rather linear, with the valve area decreasing 0.12 cm2 per year and the pressure gradient increasing 7 mm Hg per year.17 Once the valve area is reduced to about one fourth of its original size, more rapid hemodynamic alterations occur.18 Noticeable symptoms do not usually occur until severe stenosis is present. The average valve area at symptom onset is 0.93 cm2, and the average pressure gradient is 49 mm Hg17; however, there is wide individual variation. The presence of symptoms is the best indicator of outcome. The onset of symptoms is associated with a high risk for sudden cardiac death.16 A study of patients who refused AVR revealed that mor- AANA Journal/August 2006/Vol. 74, No. 4 311 tality was 57% at 3 years after the onset of symptoms.19 The average age at which patients become symptomatic depends on the cause: rheumatic disease, 39 years; bicuspid disease, 48 years; and calcific tricuspid disease, 66 years.20 Treatment There are no definitive medical treatments for AS other than antibiotic prophylaxis to prevent infective endocarditis and limitations on physical activity.15 However, there is hope for new medical therapies because calcific aortic stenosis now is believed to involve an active inflammatory atherosclerotic process. For example, recent retrospective trials demonstrated a slowing of disease progression in patients receiving statin therapy.21,22 Randomized clinical trials are currently evaluating this therapy. Asymptomatic patients are evaluated with echocardiography every 1 to 5 years. Once symptoms appear, the recommended treatment for AS is valve replacement.15 The mortality rate for AVR is 4% and, when combined with coronary revascularization, 6%.23 After the obstruction is removed, there is symptomatic improvement and a regression in left ventricular hypertrophy.4 Ventricular wall mass returns to normal after 8 years.21 Long-term survival after the procedure is comparable to age-related norms.24 Percutaneous balloon aortic valvuloplasy is a less invasive procedure that is clearly inferior to valve replacement in adult patients. Still, it can modestly increase valve area for a few months and is recommended for some patients who are not candidates for AVR and need temporary improvement.15 The search for other less invasive procedures has persisted. In 2002, the first human case of a percutaneous aortic valve replacement was reported.25 This experimental procedure is performed under local anesthesia and mild sedation. This new technology is being proposed as a possible treatment for patients with severe AS whose risk for surgery is too high due to comorbidities. Research in this area is ongoing. Aortic stenosis and noncardiac surgery The current guideline is for patients with severe or symptomatic AS to undergo AVR before elective noncardiac surgery.26 This is not always possible because the patient may be a poor candidate for AVR, the patient may refuse AVR, or the procedure is too urgent. If noncardiac surgery must be performed, some patients can benefit from preoperative balloon valvuloplasty.26 Several studies have looked at the risk associated with AS and noncardiac surgery (Table 2). The classic report by Goldman et al27 was the first to report an increased risk of cardiac complications. This was followed by a few trials in the 1980s and 1990s that suggested a more modest risk.28-30 The authors attributed these results to more aggressive monitoring and therapy. However, these studies had small samples, and the study by O’Keefe et al28 consisted mostly of minor procedures with sedation and local anesthesia. More recently, Rohde et al31 found that patients with a pressure gradient or more than 40 mm Hg have 6.8 times the risk for cardiac complications, and Kertai et al32 Table 2. Reported risk for patients with aortic stenosis undergoing noncardiac surgery* Reference Year Design No. of cases Outcomes measured 108 Nonfatal MI, death Relative risk for gradient >25 after adjustment for clinical factors, 5.2 Reported risk 32 2004 Retrospective 31 2001 Prospective 67 Major cardiac events Relative risk for gradient >40 after adjustment for clinical factors, 6.8 1998 Retrospective 55 Major cardiac events 5/55 had event; 2 MI, 2 CHF, 1 VF; same risk as control group 29 1998 Retrospective 22 Cardiac events, death 2/22 had event; 1 fatal MI, 1 noncardiac death 28 1989 Retrospective 48 Perioperative complications 1/48 had event, 1 VT 1977 Retrospective 23 Postoperative cardiac events Relative risk, 3.2 Kertai et al Rohde et al 30 Raymer and Yang Torsher et al O’Keefe et al 27 Goldman et al † * MI indicates myocardial infarction; CHF, congestive heart failure; VF, ventricular fibrillation; and VT, ventricular tachycardia. † This does not include 6 cases of hypotension included by the authors. 312 AANA Journal/August 2006/Vol. 74, No. 4 www.aana.com/aanajournal.aspx reported that patients with a gradient of more than 25 mm Hg have 5.2 times the risk. The recent studies confirm the early results by Goldman and colleagues.27 Patients with AS are clearly at higher risk for developing cardiac complications, including myocardial infarction, heart failure, and ventricular arrhythmias. In the study by Rohde et al,31 AS had the highest risk of all the echocardiographic variables studied, including mitral regurgitation. Finally, the report by Kertai et al32 indicated that the degree of stenosis is proportional to the level of risk. Patients with a pressure gradient of 25 to 49 mm Hg had a 15% complication rate, whereas patients with a gradient of more than 50 mm Hg had a 30% complication rate. Anesthetic management The principles of anesthetic management for AS are similar for cardiac and noncardiac surgery. The preoperative assessment is focused on determining the severity of AS. Whenever possible, the patient should be evaluated before surgery by a cardiologist and have an echocardiogram. Routine auscultation of heart sounds for a loud systolic murmur can identify undiagnosed patients admitted for surgery. The level of suspicion is raised if there is a history of angina, dyspnea, syncope, rheumatic disease, or a known bicuspid valve. Patients with AS and bicuspid valves are considered at moderate risk for the development of bacterial endocarditis and should receive antibiotic prophylaxis according to the American Heart Association guidelines.33 Light premedication with anxiolytics during the preoperative period can minimize the release of catecholamines in anxious patients. Intraoperative management is directed toward maintaining hemodynamic stability and cardiac output. Patients with AS usually are vasoconstricted before induction and easily become hypotensive with the administration of anesthesia. Hypotension should be treated aggressively with an alpha-adrenergic agonist such as phenylephrine to maintain coronary perfusion, which is dependent on diastolic pressure at the aortic root.34 The ischemic cascade that follows hypotension is illustrated in Figure 4. The ideal heart rate ranges from 50 to 70 beats per minute.35 Tachycardia can result in ischemia and also does not allow enough systolic time for flow across the stenotic aortic valve. Excessive bradycardia decreases cardiac output. Maintenance of sinus rhythm is important to maintain the atrial contribution to ventricular filling. Supraventricular tachycardias and atrial fibrillation should be treated immediately with synchronized cardioversion.35 External defibrillators are used for prompt conversion of ventricular fibrillation because www.aana.com/aanajournal.aspx Figure 4. Potential downward hemodynamic spiral Coronary perfusion Blood pressure Cardiovascular collapse Myocardial ischemia Preload SVR Anesthetics Ventricular dysfunction SVR indicates systemic vascular resistance. chest compressions are not effective in pushing blood through a stenotic valve.4 Fluid status should be optimized so the noncompliant left ventricle can maintain stroke volume. There is a low threshold for the placement of invasive hemodynamic monitors in patients with AS. Arterial catheters commonly are used for beat-to-beat blood pressure monitoring. Pulmonary artery catheters are useful for evaluating fluid status and cardiac output. Left-sided filling pressures normally are elevated in AS because of a noncompliant ventricle, and volume status is easily underestimated.34 Central venous catheters are poor indicators of fluid status in AS.34 Transesophageal echocardiography is a useful direct measure of preload and contractility, but the probe cannot be inserted until after the critical induction period.35 A 5-lead electrocardiogram is recommended for detection of ischemia and arrhythmias. Close monitoring should continue into the postoperative period, especially if the surgery involves significant fluid shifts.4 Anesthetic technique There is little research supporting one anesthetic technique over another for AS. The literature regarding this issue consists primarily of case reports. Some authors of anesthesia texts recommend general anesthesia over regional anesthesia because it allows greater control over blood pressure.36,37 If general anesthesia is chosen, the sympathetic response to direct laryngoscopy should be attenuated to prevent ischemia. An opioid-based technique produces minimal cardiovascular effects.33-37 Any medication that causes significant myocardial depression, hypotension, tachycardia, bradycardia, or histamine release should be used cautiously. Volatile anesthetics are used in low concentrations to avoid myocardial AANA Journal/August 2006/Vol. 74, No. 4 313 depression and nodal arrythmias.34 Some authors consider severe AS to be a contraindication to spinal and epidural anesthesia.36 The sympathectomy produced can result in rapid hypotension and deterioration in the patient’s condition (see Figure 4). However, epidural anesthesia results in a more gradual decline in blood pressure and allows incremental titration of anesthetics. Epidural anesthetics have been used at some institutions for parturients with congenital AS.38,39 A sample of other regional anesthetic techniques used safely in case reports includes intrathecal sufentanil for lithotripsy,40 continuous spinal anesthesia for hip replacement,41 and a combined lumbar plexus and sciatic nerve block for hip replacement.42 Carefully planned regional techniques like these may be an option for select patients with AS. Summary Nurse anesthetists will encounter more patients with AS as the elderly population continues to grow. Patients with AS are at substantial risk for cardiac complications in the perioperative period. A coordinated effort is needed among surgeons, cardiologists, and anesthesia professionals to minimize the risk. Aggressive hemodynamic monitoring and gentle anesthetic techniques can provide the majority of these patients with favorable outcomes. REFERENCES 1. Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. J Am Coll Cardiol. 1997;29:630634. 2. National Center for Health Statistics. National Hospital Discharge Survey, Series 13. Hyattsville, Md: Centers for Disease Control and Prevention, 1990-2002. Available at: http://www.cdc.gov/nchs. Accessed April 13, 2005. 11. Wallby L, Janerot-Sjoberg B, Steffensen T, Broqvist M. T lymphocyte infiltration in non-rheumatic aortic stenosis: a comparative descriptive study between tricuspid and bicuspid aortic valves. Heart. 2002;88:348-351. 12. Lombard T, Selzer A. Valvular aortic stenosis: a clinical and hemodynamic profile of patients. Ann Intern Med. 1987;106:292-298. 13. Munt B, Legget ME, Kraft CD, Miyake-Hull CY, Fujioka M, Otto CM. Physical examination in valvular aortic stenosis: correlation with stenosis severity and prediction of clinical outcome. Am Heart J. 1999;137:298-306. 14. Popovic AD, Stewart WJ. Echocardiographic evaluation of valvular stenosis. Echocardiography. 2001;18:59-63. 15. Bonow RO, Carabello B, de Leon AC, et al. ACC/AHA guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Valvular Heart Disease). J Am Coll Cardiol. 1998:32:1486-1588. 16. Kelly TA, Rothbart RM, Cooper M, Kaiser DL, Smucker, ML, Gibson RS. Comparison of outcome of asymptomatic to symptomatic patients older than 20 years of age with valvular aortic stenosis. Am J Cardiol. 1988;61:123-130. 17. Otto CM, Burwash IG, Legget ME, et al. A prospective study of asymptomatic valvular aortic stenosis: clinical, echocardiographic, and exercise predictors of outcome. Circulation. 1997;95:2262-2270. 18. Carabello BA. Aortic stenosis. N Engl J Med. 2002;246:677-682. 19. Chizner MA, Pearle DL, de Leon AC. The natural history of aortic stenosis in adults. Am Heart J. 1980;99:419-424. 20. Horstkott D, Loogen F. The natural history of aortic valve stenosis. Eur Heart J. 1988;9(suppl E):57-64. 21. Novaro GM, Tiong IY, Pearce GL, Lauer MS, Sprecher DL, Griffin BP. Effect of hydroxymethylglutaryl coenzyme A reductase inhibitors on the progression of calcific aortic stenosis. Circulation. 2001;104:2205-2209. 22. Aronow WS, Ahn C, Kronzon I, Goldman ME. Association of coronary risk factors and use of statins with progression of mild valvular aortic stenosis in older persons. Am J Cardiol. 2001;88:693-695. 23. Society of Thoracic Surgeons. STS National Database Fall 2000 Executive Summary. Chicago, Ill: Society of Thoracic Surgeons. 2002. Available at: http://www.sts.org. Accessed April 18, 2005. 24. Monrad ES, Hess OM, Murakami T, Nonogi H, Corin WJ, Krayenbuehl HP. Time course of regression of left ventricular hypertrophy after aortic valve replacement. Circulation. 1988;77:1345-1355. 3. Dare AJ, Veinot JP, Edwards WD, Tazelaar HD, Schaff HV. New observations on the etiology of aortic valve disease: a surgical pathologic study of 236 cases from 1990. Hum Pathol. 1993;24: 1330-1338. 25. Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. 2002;106: 3006-3008. 4. Otto CM. Valvular Heart Disease. 2nd ed. Philadelphia, Pa: Saunders; 2004. 5. Davies MJ, Treasure T, Parker DJ. Demographic characteristics of patients undergoing aortic valve replacement for stenosis: relation to valve morphology. Heart. 1996;75:174-178. 26. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2002; 105:1257-1267. 6. Wilbert SA, Chul A, Kronzon I, Goldman ME. Association of coronary risk factors and use of statins with progression of mild valvular aortic stenosis in older persons. Am J Cardiol. 2001;88:693-695. 27. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977:297:845-850. 7. Aronow WS, Ahn C, Kronzon I. Association of valvular aortic stenosis with symptomatic peripheral arterial disease in older persons. Am J Cardiol. 2001;88:1046-1047. 28. O’Keefe JH, Shub C, Rettke SR. Risk of surgical procedures in patients with aortic stenosis. Mayo Clin Proc. 1989;64:400-405. 8. Rapp AH, Hillis D, Lange RA, Cigarroa JE. Prevalence of coronary artery disease in patients with aortic stenosis with and without angina pectoris. Am J Cardiol. 2001;87:1216-1217. 9. Otto CM, Kuusisto J, Reichenback DD, Gown AM, O’Brien KD. Characterization of the early lesion of “degenerative” valvular aortic stenosis: histological and immunohistochemical studies. Circulation. 1994;90:844-853. 10. Olsson M, Dalsgaard CJ, Haegerstrand A, Rosenqvist M, Ryden L, Nilsson J. Accumulation of T lymphocytes and expression of interleukin-2 receptors in nonrheumatic stenotic aortic valves. J Am Coll Cardiol. 1994;23:1162-1170. 314 AANA Journal/August 2006/Vol. 74, No. 4 29. Torsher LC, Shub C, Rettke SR, Brown DL. Risk of patients with severe aortic stenosis undergoing noncardiac surgery. Am J Cardiol. 1998;81:448-452. 30. Raymer K, Yang H. Patients with aortic stenosis: cardiac complications in non-cardiac surgery. Can J Anaesth. 1998;45:855-859. 31. Rohde LE, Polanczyk CA, Goldman L, Cook EF, Lee RT, Lee TH. Usefulness of transthoracic echocardiography as a tool for risk stratification of patients undergoing major noncardiac surgery. Am J Cardiol. 2001;87:505-509. 32. Kertai MD, Bountioukos M, Boersma E, et al. Aortic stenosis: an underestimated risk factor for perioperative complications in patients undergoing noncardiac surgery. Am J Med. 2004;116:8-13. www.aana.com/aanajournal.aspx 33. Dajani AS, Taubert KA, Bolger WW, et al. Prevention of bacterial endocarditis: recommendations by the American Heart Association. JAMA. 1997;277:1794-1801. 34. de Villiers PA, Starr NJ. Anesthesia for the surgical management of valvular heart disease. In: Thys DM, Hillel Z, Schwartz AJ, eds. Cardiothoracic Anesthesiology. New York, NY: McGraw-Hill: 2001:589-629. 35. Moore RA, Martin DE. Anesthetic management for the treatment of valvular heart disease. In: Hensley FA, Martin DE, Gravlee GP, eds. A Practical Approach to Cardiac Anesthesia. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2003:302-335. 36. Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 3rd ed. New York, NY: McGraw-Hill; 2002. 37. Dayton DB. Cardiovascular anatomy, physiology, and pathophysiology. In: Nagelhout JL, Zaglaniczny KL. Nurse Anesthesia. 2nd ed. Philadelphia, Pa: Saunders; 2001:413-447. 38. Lao TT, Sermer M, MaGee L, Farine D, Colman JM. Congenital aortic stenosis and pregnancy: a reappraisal. Am J Obstet Gynecol. 1993;169:540-545. 39. Brighouse D. Anaesthesia for caesarean section in patients with aortic stenosis: the case for regional anaesthesia. Anaesthesia. 1998;53:107-109. www.aana.com/aanajournal.aspx 40. Eaton M. Intrathecal sufentanil analgesia for extracorporeal shock wave lithotripsy in three patients with aortic stenosis. Anesth Analg. 1998;86:943-944. 41. Collard CD, Eappen S, Lynch EP, Concepcion M. Continuous spinal anesthesia with invasive monitoring for surgical repair of the hip in two patients with severe aortic stenosis. Anesth Analg. 1995;81:195-198. 42. Ho AM, Karmakar MK. Combined paravertebral lumbar plexus and parasacral sciatic nerve block for reduction of hip fracture in a patient with severe aortic stenosis. Can J Anesth. 2002;49:946-950. AUTHOR David Phillips, CRNA, MSN, is a staff nurse anesthetist at Franklin Regional Medical Center, Louisburg, NC. He was a student at Duke University Nurse Anesthesia Program, Durham, NC, when this course was written. Email: [email protected] ACKNOWLEDGMENT I thank all the nurse anesthetists and anesthesiologists at Durham Regional Hospital, Durham, NC, for sharing their wealth of knowledge in cardiac anesthesia. AANA Journal/August 2006/Vol. 74, No. 4 315