* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 3. ECG ANALYSIS 3.1. Heartbeat
Heart failure wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Myocardial infarction wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
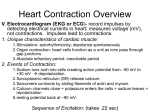
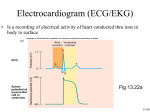
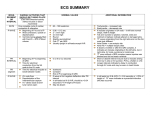
3. ECG ANALYSIS The following parameters are assessed on ECG (in undermentioned sequence): 1. Heartbeat 2. Heart rate 3. Rhythm 4. Electric axis 5. Description of waves, intervals and segments on ECG. The advanced electrocardiographs evaluate some parameters automatically (for example heart rate). A useful tool for ECG assessment is a special ruler shown in Figure 3.1.). Fig. 3.1. EGG ruler Zdroj:http://www.pharmainsight.ca/pharmaceutical-images/slcardiac%20ruler.gif 3.1. Heartbeat The heartbeat can be regular or irregular. Regularity or irregularity is determined by analyzing the time intervals between two identical successive components of the electrocardiogram, usually R-R intervals. If durations of these intervals are constant, the heartbeat is regular (Fig. 3.2). If the durations of R-R intervals differ significantly, the heartbeat is irregular (Fig. 3.3.). R-R interval Fig. 3.2. Regular heartbeat R-R interval R-R interval R-R interval Fig. 3.3. Irregular heartbeat The irregular heart beat is called arrhythmia (or dysrhythmia). The arrhythmia can occur in healthy person (so-called physiological arrhythmia) or can be induced by some pathological cause. The most common physiological arrhythmia is respiratory arrhythmia that is usually present in young persons. It is characterized by an increase in the heart rate during inspiration and a decrease in the heart rate during expiration (Fig. 3.4). The cause of respiratory arrhythmia is a tone fluctuation of vagus nerve nuclei (the decrease in tone during inspiration and the increase in tone during expiration). These nuclei are located close to a respiratory center in brainstem. Respiratory arrhythmia probably positively influences a gas exchange between alveolar air and the blood in pulmonary capillaries (the inspiration increases the pulmonary blood supply and thereby stimulates the gas exchange). The heartbeat variability provides the optimum ventilation-perfusion ratio during the entire respiratory cycle. Fig. 3.4. Respiratory arrhythmia VT – tidal volume 3.2. Heart rate Heart rate is the number of ventricular systoles per one minute. Normal heart rate (in adult person under resting conditions) is 60 - 90 beats per minute (BPM). A decreased heart rate is called bradycardia, an increased heart rate is tachycardia. Since many healthy individuals have the heart rate out of abovementioned interval, the optimum heart rate is the value ensuring a sufficient cardiac output. For example in endurance sportsmen having a stroke volume higher compared to the common population the resting heart rate is markedly lower whereas the resting cardiac output 2 is comparable to untrained people (cardiac output is equal to stroke volume multiplied by heart rate). The method of heart rate determination depends on regularity or irregularity of the heartbeat. 3.2.1 Regular heartbeat At the regular heartbeat the heart rate is calculated by means of following formulas: BPM = 60 R − R ( s) R-R (s) is a time interval of two successive R waves expressed in second (Fig. 3.5). 0,75 s Fig. 3.5. Heart rate determination at the regular heartbeat R-R interval has duration 0.75 s. The heart rate according the abovementioned formula is 60 = 80 BPM. 0.75 At a standard paper movement the following formula can be used: BPM = 150 R − R (cm) R-R (cm) is a distance of two successive R waves expressed in centimeters; 150 cm corresponds to 1 minute at the paper speed of 2.5 cm/s (Fig. 3.6). 3 2 cm Fig. 3.6. Heart rate determination at the regular heartbeat The distance of two successive R waves is 2 cm. The heart rate is 150 = 75 BPM. 2 3.2.2. Irregular heartbeat At the irregular heartbeat the following procedure is recommended (Fig. 3.7): ¾ To count number of R waves in the definite time interval. ¾ To transform the accounted value into minute interval. 10 s Fig 3.7. Heart rate determination at the irregular heartbeat 10-sec interval contains 12 R waves. Number of R waves is multiplicated by 6 (six 10-sec intervals in 1 minute) to calculate the heart rate, i.e. 72 BPM. 3.3. Rhythm The rhythm of the heart is determined by a pacemaker region spontaneously producing electric impulses. Under physiological conditions the source of cardiac rhythm is usually the fastest pacemaker, i.e. sino-atrial (SA) node – sinus rhythm. If the spontaneous activity of SA node is disturbed its function is replaced by the activity of atrioventricular (AV) node – nodal rhythm. The complete failure of conduction between the atria and ventricles leads to the complete independence of the atrial and ventricular electric activity. The atria are controlled by SA node whereas the ventricular impulses are produced by Purkyne fibers – idioventricular rhythm. The frequency of produced impulses is the highest in SA node (60 – 90 BPM), lower in AV node (46 – 60 BPM) and the lowest in Purkyne fibers (30 BPM). 4 Under pathological conditions the source of pacemaker activity can be a tissue area located outside the conductive system. If the frequency of thus produced impulses is high enough to take a control over the whole heart an arrhythmia arises. The areas elsewhere than in SA node producing electric impulses are called ectopic (ectopicus - occurring in an abnormal position or place, displaced). Criteria for the sinus rhythm are: 1. P wave appears before QRS complex (the atrial depolarization precedes the ventricular depolarization). 2. PQ interval has normal duration, i.e. from 0.12 to 0.2 s (transmission of the electric signal from the atria to ventricles is normal). 3. Heart rate ranges between 60 and 90 BPM. This condition cannot be applied to everybody. As mentioned above, although the resting heart rate of trained person is lower compared to untrained population the trained person can have the sinus rhythm. The nodal rhythm is characterized by a change in shape and position of P wave. Three types of nodal rhythm are distinguished according to the pacemaker location: 1. Upper nodal rhythm originates in the atrial part of AV node. P wave precedes QRS complex but the duration of PQ interval is shorter (transmission of the electric signal from place of origin to ventricles is faster due to a shorter distance). P wave is negative in leads II, III, aVF, V5 and V6 (Fig. 3.8a). 2. Middle nodal rhythm originates in the middle part of AV node. The electric impulse spreads towards the atria and ventricles simultaneously to initiate atrial and ventricular depolarization at the same time. Since the ventricular myocardium is thicker then atrial one, P wave is covered by QRS complex being invisible on ECG recording (Fig. 3.8b). 3. Lower nodal rhythm originates in the ventricular part of AV node. The ventricular depolarization precedes the atrial depolarization hence P wave comes after QRS complex (Fig. 3.8c). The idioventricular rhythm is characterized by a very slow frequency. This rhythm results from a block of atrioventricular transmission when the atria are controlled by the sinus rhythm and the ventricles by the idioventricular rhythm. P waves and QRS complexes are visible on electrocardiogram without any time relationship. 5 AV node a b c Fig. 3.8. Nodal rhythm The cells of AV node form the source of pacemaker activity in the nodal rhythm. a – upper nodal rhythm, b – middle nodal rhythm, c – lower nodal rhythm. 3.4. Electric heart axis The electric heart axis is the direction and size of vector of the electric heart field. As explained earlier, the changes of the electric heart field are detectable only during propagation of depolarization or repolarization, i.e. during atrial depolarization (P wave), ventricular depolarization (QRS complex) or ventricular repolarization (T wave). The direction of an average vector of QRS complex is the most important for diagnosis of cardiac diseases, and usually, as the electrical heart axis, the mean QRS vector is understood. In most healthy persons the direction of electric heart axis corresponds to the direction of the anatomic heart axis which is oriented forward, leftward and downward. It is evident, that the vector of the electric heart field is defined in threedimensional space (3D). But ECG recording of limb leads makes possible projection of vector only in the frontal plane (2D). The direction of the heart electric axis in healthy people ranges between -30° and 105° (Fig. 3.9). Shift of the electric axis to the right is called right axis deviation or vertical axis (more than 105°, Fig. 3.10). Shift the electric axis to the left is called left axis deviation or horizontal axis (less than -30°, Fig. 3.11). 6 Fig. 3.9. Normal electric heart axis Shaded area defines the direction of the normal heart axis. lead I lead I lead III lead II lead III lead II Fig. 3.10. The heart axis deviation Left – the black area defines the left axis deviation, right – the black area defines the right axis deviation. The deviation of the heart electric axis is usually caused by hypertrophy of cardiac chamber, conduction abnormalities or deviations of the heart position in the thorax. The right axis deviation can be induced by the right ventricle hypertrophy, left anterior hemiblock or by extreme slimness (the diaphragm in a slim person is moved downwards and consequently the cardiac apex leaning on the diaphragm is shifted downwards as well). On the other hand, the left axis deviation is caused by the left ventricle hypertrophy, left posterior hemiblock, obesity or by advanced pregnancy (the diaphragm 7 in obese people or in pregnant women is shifted upwards to push the cardiac apex up). The direction of the electric heart axis is also influenced by deep breathing – the right axis deviation during deep inspiration due to the diaphragm movement downwards and the left axis deviation during deep expiration due the diaphragm movement upwards. 3.4.1. Determination of the electric heart axis The electric axis can be determined by many methods. Two techniques will be explained in the following text: 1. Estimate based on leads I and III. 2. Determination by means of Einthoven’s triangle. Estimate of the electric axis based on leads I and III Based on the QRS complex shape in bipolar leads I and III the heart electric axis may be estimated: • The maximum positive QRS deflection in lead I and the maximum negative QRS deflection in lead III → the left axis deviation. • The maximum negative QRS deflection in lead I and the maximum positive QRS deflection in lead III → the right axis deviation. • Either the maximum positive QRS deflection in both lead or the maximum negative QRS ones in both leads → normal heart axis (Fig. 3.11). 8 Fig. 3. 11. Estimate of the electric heart axis by means with limb leads Determination the electric heart axis by means of Einthoven’s triangle The Einthoven’s triangle is an equilateral triangle whose sides are formed by leads I, II and III. The polarity of triangle’s sides (i.e. ECG electrodes) is given by a convention (Fig. 3.12). Fig. 3.12. Einthoven’s triangle 9 The procedure of the axis determination is following: 1. Draw an equilateral triangle and mark the polarity of sides. Plot three perpendiculars in the midpoints of the triangle’s sides. The cross point of perpendiculars forms the onset of the heart electric axis (Fig 3.13a). 2. Measure the amplitude of positive wave (R) and the maximum negative wave (Q or S) in any two bipolar leads*. Calculate the difference of both measured amplitudes as the absolute value of positive wave amplitude minus the absolute value of the negative wave amplitude (Fig. 3.13b). 3. Mark out the calculated difference on an appropriate lead (lead I – upper side, lead II – left side, lead III – right side). The direction of vector is towards positive electrode if the difference of amplitudes is positive. Conversely, the vector of negative difference directs towards the negative electrode (Fig. 3.13c). 4. Plot perpendiculars in the end points of coordinates (Fig. 3.13d). 5. Mark the cross point of perpendiculars. The electric heart axis directs towards the found cross point. Determine the axis direction by means of protractor (Fig. 3.13e). * Einthoven’s rule is stated as follows: Lead I – Lead III = Lead II. In other words, if any two leads are known at a given time, the third lead can be determined mathematically. 10 +8 a I - + - b - - II II /8/ - /2/ = 6 0 -2 I - + II II c - - I - + 6 - -7 +3 0 II II -10 heart axis beginning + + d - /3/ - /10/ = - 7 + + I - + 6 e - - I - + 6 - -7 -7 II II + + II II heart axis + + + + Fig. 3.13. Determination of the electric heart axis by means of Einthoven’s triangle 3.5. Description of waves, intervals and segments on ECG The individual waves, segments and intervals on ECG should be assessed in all leads. It is necessary to point out that lead aVR is the least useful. 3.5.1. P wave P wave caused by the atrial depolarization has maximum amplitude of 0.25 mV and its duration is up 0.1 s (Fig 3.14). This wave is positive in most leads, it can be positive or negative in lead III, usually biphasic in lead V1 (i.e. positive in the first phase and negative in the second phase) and always negative in lead aVR. 11 max. 0.25 mV P max. 0.1 s Fig. 3.14. P wave P wave caused by atrial depolarization precedes QRS complex under physiological conditions. 3.5.2. PQ (PR) interval The time interval from the beginning of P wave to the onset of QRS complex is called PQ interval (if QRS complex starts with Q wave) or PR interval (ORS complex starts with R wave). PQ (PR) interval representing the period from the beginning of atrial depolarization to the beginning of ventricular one normally lasts 0.12 – 0.2 s (Fig. 3.15). The duration of PQ interval is inversely proportional to the heart rate (it shortens with increasing heart rate and prolongs with decreasing heart rate). The prolongation of PQ interval can be physiological (in sportsmen with resting bradycardia) or pathological (due to an abnormal conduction in AV node). 0,1 s PQ PR Fig. 3.15. PQ and PR intervals PQ (PR) interval comprises the isoelectric PQ (PR) segment (Fig 3.16). During this segment all atrial cells are completely depolarized and simultaneously neither atrial repolarization nor ventricular depolarization has started thus no deflection is present on ECG. 12 0,1 s PQ segment PR segment Fig. 3.16. PQ a PR segments 3.5.3. QRS complex QRS complex is produced by the ventricular depolarization. The sequence of the ventricular depolarization is following: AV node – interventricular septum (from the left to the right) – cardiac apex – free ventricular walls – atrioventricular groove. Depolarization in the free walls travels from endocardium to epicardium. Normal duration of QRS complex ranges between 0.06 and 0.11 s. QRS complex consists of three waves (Q, R and S). But all three waves are not ordinarily found in each lead. R wave is always positive. Q and S waves are always negative, Q wave precedes R wave whereas S wave follows R wave. The complex formed by only one negative wave is called QS (the absence of R wave makes the exact designation impossible). The other positive waves in QRS complex are specified by apostrophe R, R´, R´´ …). The various forms of QRS complex are shown in the picture 3.17. 13 R R R r q q s S S R R 0,1 s R R´ r S QS Fig 3.17. Various forms of QRS complex Small and capital letters determine the wave height – small letters (q, r, s) for waves bellow 5 mm and capital letters (Q, R, S) for waves above 5 mm. 3.5.4. Q wave The Q wave is caused by the depolarization of the ventricular septum and papillary muscles. Its duration should be less than 0.03 s and the amplitude maximum ¼ of R wave amplitude (in the same lead). The wave with parameters outside these ranges is called pathological Q. Q wave is usually found in leads located above the surface of the left ventricle (V5 and V6). 3.5.5. R wave Always positive R wave is produced by free ventricular walls depolarization. The maximum R wave amplitude in the limb leads is 10 mm. In the chest leads R wave amplitude increases from V1 to V5 to reach the same or smaller amplitude in V6 compared to V5 (Fig. 3.18). The time interval from the onset of Q wave to the peak of R wave called the ventricular activation time corresponds to the depolarization of the whole ventricular walls. The ventricular 14 activation time measured in V1 shows the activation of the right ventricle (normally up to 0.03 s) whereas in V6 the left ventricular activation (up to 0.04 s). An extended ventricular activation time is usually an indication of the ventricular hypertrophy. R S V1 V2 V3 V4 V5 V6 Fig 3.18 . R and S waves in chest leads The amplitude of R wave increases from lead V1 to V5 (rarely V6), S wave decreases. 3.5.6. S wave The amplitude of S wave in chest leads decreases from V1 to V6. In lead V6 this wave is usually not present (Fig. 3.18). 3.5.7. ST segment The ST segment represents the period from the end of ventricular depolarization to the beginning of ventricular repolarization. The normally isoelectric ST segment lies between the end of the QRS complex and the initial deflection of the T wave. The point marking the end of the QRS complex and the beginning of the ST segment is called J point. This point should be at the same level as beginning of Q wave (i.e. on the isoelectric line). The shift of ST segment above the baseline is called ST elevation. The tolerated elevation is 0.1 mV in the limb leads and 0.2 mV in the chest leads. The shift of ST segment below the baseline is called ST depression; the tolerated depression is 0.1 mV. A variation of ST segment can result from a lot of causes both trivial (e.g. an activation of sympathetic nervous system due to fear, angriness or physical effort) and severe (angina pectoris, myocardial infarction, ion imbalance or cardiotonics overdose). 15 3.5.8. T wave The ventricular repolarization spreads from the atrioventricular groove through the cardiac apex to the ventricular septum to produce T wave on ECG. The direction of the ventricular repolarization is opposite to the depolarization. In the free ventricular walls the repolarization travels from epicardium to endocardium hence the polarity of T wave corresponds to the polarity of the QRS wave with the highest amplitude (if R wave has the highest amplitude T wave is positive; if S or Q wave is maximum T wave is negative). Under physiological conditions negative T wave is found in leads aVR, III, V1 and V2. T wave duration is about 0.2 s, its amplitude ranges between 0.2 and 0.8 mV. 3.5.9. U wave U wave is a small positive wave sometimes visible after T wave (Fig. 3.19). It can be normally present in young people and sportsmen. The pathological appearance of U wave is due to hypokalemia (a decrease in plasmatic concentration of potassium). U wave probably results from the delayed repolarization of Purkyne fibers or some areas of the ventricular myocardium. U wave Fig 3.19. U wave 3.2.10. QT Interval QT interval is defined by the onset of QRS complex and the end of T wave. This interval comprises the depolarization and repolarization of ventricles (so-called an electric systole of ventricles). Duration of QT interval is significantly influenced by changes in heart rate (shortening due to tachycardia and prolongation due to bradycardia). Therefore the duration of QT interval is corrected for the heart rate and the corrected value is marked QTc. (Various formulas are used for the correction but 16 their explanation is beyond the scope of this study material). A normal value of QTc is from 0.32 to 0.42 s. The most important time intervals for remembering are shown in the following table: PQ interval 0.12 – 0.2 s QRS complex 0.06 – 0.11 s QT interval 0.32 – 0.42 s 17