* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Mood Disorders Mental Health vs Mental Illness
Schizoaffective disorder wikipedia , lookup
Antipsychotic wikipedia , lookup
Bipolar disorder wikipedia , lookup
Abnormal psychology wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Causes of mental disorders wikipedia , lookup
History of mental disorders wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Postpartum depression wikipedia , lookup
Child psychopathology wikipedia , lookup
Mental status examination wikipedia , lookup
Major depressive disorder wikipedia , lookup
Behavioral theories of depression wikipedia , lookup
Epigenetics of depression wikipedia , lookup
Biology of depression wikipedia , lookup
Antidepressant wikipedia , lookup
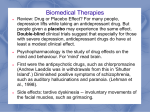
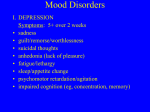
Mood Disorders Mental Health vs Mental Illness Maslow • Identified self actualization as being “psychologically healthy, fully human, highly evolved, and fully mature.” • Appropriate perception of reality • Ability to accept oneself and others • Ability to focus (concentrate) and problem solve • Ability to have satisfactory interpersonal relationships • Creativeness • Desire for a certain amount of privacy and ability to detach if needed • Sense of ethics • Creativity • A degree of conformance Jahoda • Positive attitude • Growth, development, and the Ability to Achieve Self-Actualization • Integration • Autonomy • Perception of reality • Environmental mastery Locus of Control • External • Internal Mental Health Viewed as the successful adaptation to stressors from the internal or external environment, evidenced by thoughts, feelings, and behaviors that are age-appropriate and congruent with local and cultural norms. Mental Illness • Universal concept is difficult because of the influence of cultural factors. • Maladaptive responses to stressors from the internal or external environment, evidenced by : Anxiety and Grief • Two major primary responses to stress • Continuum of health to illness Mild anxiety or feelings of sadness or life’s everyday disappointments-use coping mechanisms such as smoking, talking it out Moderate anxiety-add in defense mechanisms (such as denial) and/or psychophysiological responses (such as headaches, ulcers). Also see Neurotic responses, dysthymia (non psychotic depression) Severe anxiety to panic- add in psychoneurotic responses such as obsessions, amnesia. Can even become delusional (psychotic) Depression Non psychotic mood disorders • An occasional bout with the blues Short lived, normal, utilized learned coping skills. Transient depression –life’s everyday disappointments Seasonal depression • Grief Normal response to losses perceived as important to the individual. What might cause grief in one person can cause little or no sadness in another. • Cyclothymia Possible nursing diagnoses for mood disorders • Mild depression May experience anorexia or overeating, insomnia or hypersomnia, headaches, backaches, chest pain, tearfulness, blaming others, guilt, anger • Moderate depression Signs and Symptoms: • Severe Depression • Major Depression • Will learn more about this in Soph II but we will have a brief description Affect: Blunted: significantly reduced intensity of emotional expression Flat: absent or nearly absent affective expression Inappropriate: expression does not reflect the content of speech or ideation Labile: varied, rapid, abrupt shifts in affective expression Bipolar disorder • Theory -Etiology is unclear. Most believe that biological and psychosocial factors come into play. • Affect- • May or may not have delusions/hallucinations. • Delusions-many times grandiosity or paranoia Grandiosity is an exaggerated sense of self importance, power, or status. Employed to reduce feelings of insecurity and increases feeling of power. • Hallucinations Interventions • Accurate assessment of s/sx • Develop a trusting relationship, encourage client to express feelings openly • Encourage them to express anger (do not become defensive) • Participation in large motor activities just as physical exercises, volleyball, punching bag help discharge pent-up anger • • • • Assist in problem solving Encourage support groups Intake and output Teach effective communication (I message, etc) • Provide helpful measures to promote sleep • Watch for suicidal gestures or ideation • Suicide watch if nurse feels it is warranted (usually 1:1 to closely monitor patient) Remember that when in deepest depression, patients aren’t as likely to commit suicide because of decreased energy. It’s when they start to feel more energy that they are more likely to harm self. But be aware IT CAN HAPPEN ANYTIME. • Clients are usually very withdrawn when depressed with little energy. We don’t want to overtax, but we want them to participate as soon as possible. Maybe have to walk them to their activity. • Newly admitted depressed patients do better with one on one interaction, then progressed to socialization with others/groups. Therapies • Cognitive therapy-individual is taught about thought distortions (individual and/or group) • Group therapy-used once acute phase of depression passed. Peer support provides feeling of security. Yalom’s curative factors • Family therapy- aimed at restoring family functioning • Behavioral therapy • Light therapy • ECT • Psychopharmacology Medications for depression Antidepressants • • • • Tricyclics Monoamine Oxidase Inhibitors Selective Serotonin Reuptake Inhibitors Others Antidepressants may cause sedation at first. But over time, the patient’s body gets used to the medication, and the patient is not sleepy from taking it. Many antidepressant will lower the seizure threshold. Many cause anticholinergic side effects. • Tricyclic antidepressants Blocks the absorption (reuptake) of the neurotransmitters serotonin and norepinephrine, making more of these chemicals available in the brains. Helps brain cells send and receive messages, which in turn, boosts mood. There is also a drug that is a tetracyclic that you may see (Maprotiline) • Side effects of tricyclics: Anticholinergic effects (dry mouth, urinary retention) Increased appetite Drop in blood pressure when moving to a standing position. Increased sweating Other side effects • Interactions Taking a tricyclic with other drugs can cause many drug interactions. Always note this when you look up and read about an antidepressant. For example: when used with phenothiazines (antipsychotic drugs) risk for seizure increases. . • Decreased or increased effects of other drugs can occur . • Example-increased anticoagulation effects may occur with dicumarol. (So patient could have bleeding) • Some names you might see Amitriptyline-Elavil Amoxapine Imipramine-(Tofranil) Nortriptyline-Pamelor Tricyclic antidepressants are ordered per their generic name at this time. • Monoamine Oxidase Inhibitors Major problem-Interaction with tyramine-rich foods and certain medication that can result in hypertensive crisis. Names: Isoboxazid (Marplan), Tranylcypromine (Parnate), and Phenelzine (Nardil) • Tyramine Rich Foods: • Sympathomimetics • SSRI’s Citalopram (Celexa) Escitalopram (Lexapro) Fluoxetine (Prozac) Paroxetine (Paxil) Sertraline (Zoloft) • SSRI’s Action: Decreased serotonergic neurotransmission has been proposed to play a key role in depression. Prozac was the first of a class of drugs that acted “selectively” on serotonin. All SSRIs inhibit the reuptake of serotonin by blocking its transport into the presynaptic neuron, which in turn increases the concentration of synaptic serotonin. • Side effects of SSRIs Headache, anxiety, insomnia, transient nausea and vomiting, diarrhea. Sedation may occur. See chapter 11 for other side effects. • Norepinephrine Dopamine Reuptake Inhibitors Bupropion (Wellbutrin) inhibits reuptake of norepinephrine, serotonin, and dopamine. Some have experienced anxiety, insomnia, appetite suppression. A few have experienced hallucinations and delusions. Lowers seizure threshold. (So not good to give to head injury pt) Lithium • Once dosage adjusted, don’t change salt intake. • Lithium levels • Drink plenty of fluids • Lithium is prescribed as a mood stabilizer for the treatment of bipolar disorder. It acts to help control the associated mania, hypomania, depression and psychosis. • Lithium is formally approved to treat manic episodes of bipolar disorder when symptoms such as grandiosity, racing thoughts, hypersexuality, delusions, hallucinations, and decreased need for sleep appear. • However, it has also been shown to help with depressive symptoms • Some research has shown that lithium can be effective in treating unipolar depression when added to one or more other depression medications, so it is sometimes prescribed for this use. • • • • • • • • Warnings About Lithium There are several important warnings for people taking lithium. These include:•Serum blood level must be monitored regularly. Lithium can be toxic if this gets too high. Symptoms of lithium toxicity include diarrhea, vomiting, tremor, mild problems walking, drowsiness, or muscular weakness. Report such symptoms to a doctor immediately. •There is a danger of a condition called lithium nephrogenic diabetes insipidus (NDI). If you notice that you are excessively thirsty and are urinating too often, check with a doctor at once. Precautions When Taking Lithium •Make sure you maintain normal fluid and salt intake when taking lithium. Dehydration or low levels of sodium in the blood may have serious consequences. •Prolonged sweating, diarrhea, or a high fever can cause your tolerance to lithium to decrease and may require medical treatment. Check with your doctor if any of these conditions occurs. •Lithium can cause increased thyroid and parathyroid activity. Your doctor should check blood calcium levels periodically, as these are connected to the workings of the parathyroid gland, as well as for overactive thyroid. Be extremely careful when used with diuretic. • Serum blood level describes the amount of a given medication present in your blood at the time of testing. Blood serum is the liquid part of the blood that contains no clotting factors or blood cells. • Some medications used to treat bipolar disorder require serum blood level testing. People taking lithium in particular must be tested regularly, as there is a narrow "therapeutic window" for lithium. That means that the difference between a therapeutic level and toxic level can be small in some individuals. .5-1.5 mEq/L • Above 1.5 is considered critical • Other medications that require serum blood level testing include Tegretol (carbamazepine) and Depakote / Depakene (sodium valproate, valproic acid). (These are anti seizure meds but are also used for mood disorders) Anticonvulsants: ( also used for mood stabilizers) Need blood levels Tegretol (Carbamazepine)-watch for hematologic and hepatic toxicity. Also may have neurotoxic side effects and EKG changes. Sedation is common. Decreases blood levels of doxycycline, theophylline, coumadin, and birth control pills. May aggravate CV disease, so no smoking when on drug. Depakote (divalproex sodium) -Fewer drug interactions than carbamazepine. Neurotin (gabapentin)- Side effect of gait instability. Trileptal-(Oxcarbazepine) -Watch for adverse neurologic events such as speech problems, gait disturbance, fatigue, somnolence, abnormal cooridation. ECT • Electroconvulsive Therapy • Meds used: Short acting anesthetic Succinylcholine- Muscle relaxant Airway applied Shock applied-seizure must be 25 sec Ventilation Airway removed Confusion when awakes-protect and reorient Suicide Risk for suicide Ask the client directly, “Have you thought about killing/harming yourself today”? If yes, do they have a plan. If so, risk is higher that it happens soon. Create a safe environment. No sharps, etc. Short term verbal or written contract with the client that he /she won’t harm self during a specific time period. Have them commit to Notifying staff if the thought enters their mind. Maintain close observation. Encourage verbalization of honest feelings. Identify community resources/support people, etc. Orient as needed. Spend time with the client. Conveys the message “You are important”. Signs of possible suicide ideation Signs/symptoms of suicidal thoughts • • • • • • • Talking about suicide Obtaining the means to do it Withdrawal Mood swings Preoccupied with death Feeling trapped or hopeless Increased use of drugs or alcohol • Giving away belongings or getting affairs in order • Changing normal routine, including eating or sleeping patterns • Doing risky or self destructive things • Saying goodbye to people • Personality changes or being severely agitated • What do you do when a client is suicidal? • If a patient says he’s thinking of harming himself, ask him if he has a plan. Find out what the plan is/lethality • No suicide contract • 1:1 • No sharps, eating utensils, strings, ropes, cords, etc. High risk for suicide • Elderly men (especially if wife dead) • Adolescents taking antidepressants-not as high risk typically as elderly men • Others Aging Adult • Cognitive Changes: Depression NOT a normal part of aging Contributing factor to social/physical limitations Complicates/interferes with medical tx Decrease in overall happiness-Isolates Increases risk for suicide Often caused by transitions in life and loss During retirement • Causes of stressors are often: economic, relationships, loss to death of loved ones and friends, changes in routine • Affects spouse, children, grandchildren • Early planning for retirement smooths transition Psychosocial changes • Correlation with extent of isolation and age • Attitudes/problems that may be seen: “My family no longer needs me” Inability to provide adequate self care May exhibit odd/off putting behaviors If no longer able to drive self or institutionalized, may suffer from not seeing loved ones Children and Adolescents • Two week period of change of behavior-may indicate an underlying depressive disorder