* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Hypotonic infants and the Prader-Willi Syndrome
Survey
Document related concepts
Genetic testing wikipedia , lookup
Epigenetics in learning and memory wikipedia , lookup
Epigenomics wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
X-inactivation wikipedia , lookup
Neocentromere wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Cell-free fetal DNA wikipedia , lookup
Microevolution wikipedia , lookup
Bisulfite sequencing wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Epigenetics of diabetes Type 2 wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Medical genetics wikipedia , lookup
Genome (book) wikipedia , lookup
Down syndrome wikipedia , lookup
Hemiparesis wikipedia , lookup
Transcript
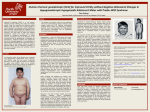
246 Jornal de Pediatria - Vol. 76, Nº3, 2000 0021-7557/00/76-03/246 Jornal de Pediatria Copyright © 2000 by Sociedade Brasileira de Pediatria CASE REPORT Hypotonic infants and the Prader-Willi Syndrome Cintia Fridman,1 Fernando Kok,2 Célia P. Koiffmann3 Abstract Objective: to describe 6 patients with less than 3 years of age that were diagnosed with Prader-Willi syndrome (PWS) due to hypotonia, poor sucking, slight facial anomalies and minor abnormalities of hands and feet. PWS is a neurobehavioural disorder characterized by two distinct phases; in the first, the neonate presents variable degree of hypotonia, feeding problems with none or poor sucking; hypogonadism, characteristic facial features with almond shaped eyes, narrow bifrontal diameter and down-turned corners of the mouth. Neuropsichymotor development is delayed. Hypotonia is non progressive and tends to improve between 8 and 11 months of age. The second phase then starts and is characterized by increasing hyperphagia and obesity, among other features. Unfortunately, most PWS patients are diagnosed only after obesity is installed. Methods: Methylation, microsatellites analysis and karyotypic studies by traditional and in situ hybridization techniques were done. Results: A deletion of chromosome segment 15q11q13 was disclosed in 4 and maternal disomy in two patients. Conclusion: the diagnosis of PWS is generally established after the onset of obesity. So, we suggest that the genetic analysis must be carried out in children with severe hypotonia of unknown cause, poor sucking and some facial features of PWS (small hands and feet, hypogonadism, hypopigmentation, almond eyes and narrow bifrontal diameter). This can allow the early diagnosis and avoid invasive exams necessary for neuromuscular disorder diagnosis like muscle biopsy and electroneuromiography, wich frequently are associated with inconclusives results. J Pediatr (Rio J) 2000; 76(3): 246-50: Prader-Willi syndrome, hypotonia, genomic imprinting, deletion 15q11q13, maternal UPD15, hypogonadism. Introduction Prader-Willi syndrome (PWS), a neurobehavioral disorder which was first described in 19561, is currently one of the most frequent syndromes with chromosomal microdeletions, and the most common type of obesity of genetic origin.2 In addition, PWS and the Angelman syndrome (AS) (delay in neuropsychomotor development, mental retardation, absence of speech, convulsions, and happy disposition) were the first human diseases acknowledged as being determined by the genomic imprinting mechanism. 3 The incidence of PWS is approximately 1/10,000 to 1/30,000 births4,5 and it is usually sporadic, with few familial cases reported.6 Although many PWS clinical manifestations result from hypothalamic deficiencies, no structural defect of the hypothalamus has been found in postmortem exams. 1. MSc, Biology/Genetics. Genetic Counseling Unit, Biology Department IBUSP, São Paulo, Brazil. 2. Ph.D, Assistant Physician. Infant Neurology Service, Hospital das Clínicas - FMUSP, São Paulo, Brazil. 3. Ph.D., Professor, Chief of the Genetic Counseling Unit, Biology Department - IBUSP, São Paulo, Brazil. 246 Hypotonic infants and the Prader-Willi Syndrome - Fridman C et alii Therefore, the deficiency seems to be functional, but its nature remains unknown.2 During the past few years, the genetic base of PWS has been extensively investigated; still, the clinical diagnosis of this disorder is complex, considering that some characteristics change according to the age and can be present in other syndromes as well. PWS can be defined as presenting two distinct phases.4,7,8 The first is characterized by different levels of hypotonia during the neonatal period and the early childhood years (94%). Hypotonia is nonprogressive, and it starts to improve on average between the age of 8 and 11 months. Hypotonia is also characterized by hypothermia or hyperthermia without any apparent cause, hypogenitalism (95%), poor sucking (93%), small hands and feet and minor facial anomalies. Another aspect observed is that these children rarely vomit. When hypotonia improves, and the child becomes more alert, there is an increase in appetite and weight gain. The onset of obesity may take place between the ages of 1 and 6, with an average at 2 years8,9 and it may be a marker to signal the beginning of the second phase. This second phase is characterized by a delay in neuropsychomotor development (98%) - the child presents a delay in learning how to sit, walk, and in speech acquisition. Other characteristics that are present in this phase are hyperphagia, obesity (94%), low stature (76%), small hands and feet (83%), decreased physical activity, decreased sensitivity to pain,8,10 hypopigmentation of hair, skin and retina, learning impairment, and facial characteristics such as a narrow forehead (75%), almond-shaped eyes (75%), and strabismus (52%). Some children between 3 and 5 years of age may develop personality problems, such as depression, irritation, violence episodes, sudden mood changes, little interaction with people, immaturity, and inappropriate social behavior.11 PWS results from the absence of paternal genes that are usually active in chromosomal segment 15q11-q13; the maternal inherited alleles are usually inactive, due to the genomic imprinting mechanism. These paternal genes may be absent as a result of different mechanisms: 75% of the PWS cases present paternal deletion of segment 15q11q13; 20-25% present maternal uniparental disomy (inheritance of two maternal chromosomes 15);12,13 approximately 5% of the PWS cases present translocation or other structural chromosomal anomaly involving chromosome 15; around 1% of the patients (including all the families with recurrence of PWS that have been studied so far) do not present deletion or uniparental disomy, but instead present a microdeletion in the imprinting controller center, called imprinting center, located in segment 15q11q13.6,14,17 In this work, we describe the clinical characteristics and the genetic diagnosis of six patients younger than 3 years of age, emphasizing the importance of an early PWS diagnosis. Jornal de Pediatria - Vol. 76, Nº3, 2000 247 Patients and Methods Patients The patients were referred to the Genetic Counseling Service (IB-USP) with hypotonia, poor sucking and slight anomalies on the face and extremities (Figure 1). Consent for publication of the photographs was obtained from all parents. Genetic study The diagnosis of PWS was established through analysis of the exon 1 methylation pattern in the SNRPN gene, located in the PWS and AS critical region, using the Southern blot technique.18 The genetic mechanism was determined through the analysis of the chromosome 15 microsatellite segregation standard, using the polymerase chain reaction (PCR) technique,19 G-banding karyotype and fluorescent in situ hybridization (FISH). Results The patients’ clinical characteristics are summarized in Table 1. The karyotypic analysis was carried out in five out of six patients, with results in all of them. Regarding molecular results, all six patients presented a typical PWS methylation pattern, confirming the clinical suspicion. The analysis of microsatellites, along with FISH results, revealed that, out of six patients with PWS, four presented deletion of segment 15q11q13, and two presented maternal uniparental disomy. Discussion The differential diagnosis of hypotonia in infants includes neuromuscular diseases such as infant spinal amyotrophy and congenital myopathies. For the diagnosis of these diseases, the performance of electroneuromyography and muscle biopsy is indicated. The performance and interpretation of these invasive exams is sometimes difficult, and they may lead to wrong diagnoses. In PWS, muscle biopsy can reveal atrophy of type-II fibers, but this finding is not specific. The karyotype rarely defines a diagnosis of PWS or AS. Currently, the most efficient method to diagnose these diseases is a molecular test that determines the progenitorspecific methylation pattern in the PWS/AS region, using Southern blot and hybridization with probes that are sensitive to methylation of the SNRPN and PW71 loci.6,20-23 In patients with suspicion of PWS, a normal methylation pattern eliminates the possibility of PWS with 95% certainty. Although the prevalence of PWS in children with hypotonia is not known, the methylation test has to be considered for the differential diagnosis, mainly among infants presenting serious hypotonia of unknown cause. Hypotonic infants and the Prader-Willi Syndrome - Fridman C et alii 248 Jornal de Pediatria - Vol. 76, Nº3, 2000 A D B C E F Figure 1 - Patients with Prader-Willi syndrome. a) Patient 6 - 2 years and 4 months old; b) Patient 3 - 1 year and 8 months old; c) Patient 2 - 10 months old; d) Patient 4 - 9 months old; e) Patient 1 - 9 months old; f) Patient 5 - 10 months old. See slim fingers in b, c, e and f, strabismus in a, b, e and f, mouth bent downwards in a, c, and e Gillessen-Kaesbach et al.11 tested 65 children between 0 and 12 months of age with idiopathic hypotonia and detected 29 PWS cases (45%). Those authors emphasize that although this frequency is probably overestimated, due to an investigation bias, the methylation test should be performed in this group of patients, considering that it is non-invasive and extremely effective to diagnose PWS. The prenatal diagnosis through the study of the methylation pattern should be considered in families with rearrangements in chromosome 15, in women who already had a child with the syndrome, and in patients with trisomy of chromosome 15 on chorionic villus culture and a normal chromosome count on amniocentesis,24 since it is known that advanced maternal age is associated with cases of uniparental disomy 15, due to its association with meiotic errors.25 In our sample, we also observed that the mothers were older in uniparental disomy cases. The search for the genetic mechanism that causes PWS is important for the genetic counseling of parents and relatives. The risk for deletion and disomy is low, around 1%; the only high risk (50%) is associated with rare occurrences of mutations and translocations in the imprinting mechanism. The early diagnosis of PWS is important because it gives the parents the opportunity of providing adequate diets and stimulating appropriate eating and exercise habits, so as to reduce the problems related to obesity, e.g. diabetics, hypertension, and respiratory problems, which are the main causes of death among these individuals during adolescence. In addition, children and teenagers with PWS present a developmental delay in several fields, and an early diagnosis prompts the parents to look for professional help (teachers, pedagogues, physical therapists, and speech therapists). During adolescence, the family may lose control over the child’s diet, since teenagers seem to use their intelligence and shrewdness to obtain food, becoming aggressive when it is denied to them. These individuals may eat leftovers, pet food, and some of them even eat dirt; some children may develop “psychotic” behaviors. 11 Experience shows that psychological support to the patient and to the parents and Hypotonic infants and the Prader-Willi Syndrome - Fridman C et alii Table 1 - Jornal de Pediatria - Vol. 76, Nº3, 2000 249 Clinical characteristics and complementary exams of PWS carriers Patient 1 2 3 4 5 6 Sex F M M F F M Age (months) 9 10 20 9 10 28 Mother’s age (years) 45 22 28 30 20 48 Father’s age (years) 41 24 25 34 29 52 Fetal movements 0 Normal Decreased Normal Normal Decreased Birth weight (g) 2110 2390 2680 3025 2440 1780 Length (cm) 42 47 48 51 45 36 Hypotonia + + + + 0 + Poor sucking + + + + + - Delay in neuropsychomotor development + + + + + + Weight 10<P<25% 10% 25<x<50% 50% 90<x<97% <2.5% Height 10<P<25% 0 2,5% 75% 75% <2.5% 50% 25<P<50% 50<x<75% 75% 0 <2.5% - + + + - - Cephalic perimeter Hypertelorism Almond-shaped eyes + + + 0 + 0 Strabismus + + - + + + Narrow forehead + + + - + + Small hands and feet + + 0 + + + Muscle biopsy NP type II FA type II FA NP NP type II FA Electroneuromyography NP Normal Myopathic NP NP Myopathic UPD* Deletion Deletion Deletion Deletion UPD Genetic mechanism + = presence of characteristic - = absence of characteristic 0 = data not available NP = not performed type II FA = type II fiber atrophy UPD = uniparental disomy * = prenatal exam performed, showing chromosome 15 trisomy on chorionic villus sampling and normal complement on amniocentesis brothers/sisters should begin during childhood and continue throughout adulthood, when the major problem is weight and behavior control, with the occurrence of irritation periods, and sometimes of psychotic episodes. Since in our setting the diagnosis of PWS is generally established after the beginning of obesity, we suggest genetic testing for this disease be requested in newborns and infants presenting hypotonia, poor sucking, and some of the phenotypic characteristics of PWS (small hands and feet, signs of hypogonadism, hypopigmentation in relation to relatives, almond-shaped eyes, narrow forehead). This may help the establishment of an early diagnosis, decreasing the need for more invasive diagnostic resources, sometimes of difficult interpretation, such as electroneuromyography and muscle biopsy. Acknowledgment This work was spondored by FAPESP (C.F.) and PRONEX (C.P.K.). References 1. Prader A, Labhart A, Willi H. Ein syndrom von Adipositas, kleinwuchs, kryptochismus und ologophrenie nach myotonieartigem zustand in neugeborenalter. Schweiz Med Wochenschr 1956; 86:1260-1. 2. Cassidy SB. Prader-Willi syndrome. J Med Genet 1997; 34:917-23. 3. Nicholls RD, Knoll JHM, Butler MG, Karam S, Lalande M. Genetic imprinting suggested by maternal heterodisomy in nondeletion Prader-Willi syndrome. Nature 1989; 342:281-5. 250 Jornal de Pediatria - Vol. 76, Nº3, 2000 4. Cassidy SB. Prader-Willi syndrome. Curr Prob Pediatr 1984; 14:1-55. 5. Mascari MJ, Gottlieb W, Rogan PK, Butler MG, Waller DA, Armour JAL, et al. The frequency of uniparental disomy in Prader-Willi syndrome. N Engl J Med 1992; 326:1599-607. 6. Saitoh S, Buiting K, Cassidy SB, Conroy JM, Driscoll DJ, Gabriel JM, et al. Clinical spectrum and molecular diagnosis of Angelman and Prader-Willi syndrome imprinting mutation patients. Am J Med Genet 1997; 68:195-206. 7. Butler MG, Meaney FJ, Palmer CG. Clinical and cytogenetic survey of 39 individuals with Prader-Labhart-Willi syndrome. Am J Med Genet 1986; 23:793-809. 8. Butler MG. Prader-Willi syndrome: current understanding of cause and diagnosis. Am J Hum Genet 1990; 35:319-32. 9. Holm VA, Cassidy SB, Butler MG, Hanchett JM, Greenswag LR, Whitman BY, et al. Prader-Willi syndrome: consensus diagnostic criteria. Pediatrics 1993; 91:398-402. 10. Ledbetter DH, Riccardi VM, Airhart SD, Strobel RJ, Keenan BS, Crawford JD. Deletions of chromosome 15 as a cause of the Prader-Willi syndrome. N Engl J Med 1981; 304:325-9. 11. Einfeld SL, Smith A, Durvasula S, Florio T, Tonge BJ. Behavior and emotional disturbance in Prader-Willi syndrome. Am J Med Genet 1999; 123-7. 12. Robinson WP, Bottani A, Yagang X, Balakrishman J, Binkert F, Machler M, et al. Molecular cytogenetic, and clinical investigations of Prader-Willi syndrome patients. Am J Hum Genet 1991; 49:1219-34. 13. Mascari MJ, Gottlieb W, Rogan PK, Butler MG, Waller DA, Armour JAL, et al. The frequency of uniparental disomy in Prader-Willi syndrome. N Engl J Med 1992; 326:1599-607. 14. Reis A, Dittrich B, Greger V, Buiting K, Lalande M, GillessenKaesbach G, et al. Imprinting mutations suggested by abnormal DNA methylation patterns in familial Angelman and PraderWilli syndromes. Am J Hum Genet 1994; 54:741-7. 15. Sutcliffe JS, Nakao M, Christian S, Örstavik KH, Tommerup N, Ledbetter DH, et al. Deletions of a differentially methylated CpG island at the SNRPN gene define a putative imprinting control region. Nature Genet 1994; 8:52-8. 16. Buiting K, Saitoh S, Gross S, Dittrich B, Schwartz S, Nicholls RD, et al. Inherited microdeletions in the Angelman and PraderWilli syndromes define an imprinting center on human chromosome 15. Nature Genet 1995; 9:395-400. 17. Saitoh S, Buiting K, Rogan PK, Buxton JL, Driscoll DJ, Arnemann J, et al. Minimal definition of the imprinting center and fixation of a chromosome 15q11-q13 epigenotype by imprinting mutations. Proc Natl Acad Sci USA 1996; 93:7811-15. Hypotonic infants and the Prader-Willi Syndrome - Fridman C et alii 18. Southern EM. Detection of specific sequences among DNA fragments separated by gel eletroforesis. J Mol Biol 1975; 98:503-17. 19. Mutirangura A, Greenberg F, Butler MG, Malcolm S, Nicholls RD, Chakravarti A, et al. Multiplex PCR of three dinucleotide repeats in the Prader-Willi/Angelman critical region (15q1113): molecular diagnosis and mechanism of uniparental disomy. Hum Molec Genet 1993; 2:143-51. 20. Gillessen-Kaesbach G, Gross S, Kaya-Westerloh S, Passarge E, Horsthemke B. DNA methylation based testing of 450 patients suspected of having Prader-Willi syndrome. J Med Genet 1995; 32:88-92. 21. Butler MG. Molecular dignosis of Prader-Willi syndrome: comparison of cytogenetic and molecular genetic data including parent of origin dependent methylation DNA patterns. Am J Hum Genet 1996; 61:188-90. 22. Glenn CC, Saitoh S, Jong MTC, Filbrandt MM, Surti U, Driscoll DJ, et al. Gene structure, DNA methylation, and imprinted expression of the human SNRPN gene. Am J Hum Genet 1996; 58:335-46. 23. Kubota T, Sutcliffe JS, Aradhya S, Gillessen-Kaesbach G, Christian SL, Horsthemke B, et al. Validation studies of SNRPN methylation as a diagnostic test for Prader-Willi syndrome. Am J Med Genet 1996; 66:77-80. 24. Clayton-Smith J, Driscoll DJ, Waters MF, Webb T, Andrews T, Malcolm S, et al. Difference in methylation patterns within the D15S9 region of chromosome 15q11-13 in first cousins with Angelman syndrome and Prader-Willi syndrome. Am J Med Genet 1993; 47:683-6. 25. Robinson WP, Langlois S, Schuffenhauer S, Horsthemke B, Michaelis RC, Christian S, et al. Cytogenetic and age-depend risk factors associated with uniparental disomy 15. Prenatal Diagnosis 1996; 16:837-44. Correspondence: Dra. Cintia Fridman Unidade de Aconselhamento Genético, IBUSP Caixa Postal 11461 CEP 05522-970 – São Paulo, SP, Brazil E-mail: [email protected]