* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ischemic dysfunction in transgenic mice expressing - AJP
Survey
Document related concepts
Transcript
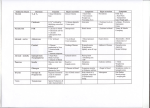
Am J Physiol Heart Circ Physiol 280: H835–H843, 2001. Ischemic dysfunction in transgenic mice expressing troponin I lacking protein kinase C phosphorylation sites Received 1 March 2000; accepted in final form 13 September 2000 MacGowan, Guy A., Congwu Du, Douglas B. Cowan, Christof Stamm, Francis X. McGowan, R. John Solaro, Alan P. Koretsky, and Pedro J. Del Nido. Ischemic dysfunction in transgenic mice expressing troponin I lacking protein kinase C phosphorylation sites. Am J Physiol Heart Circ Physiol 280: H835–H843, 2001.—To determine the in vivo functional significance of troponin I (TnI) protein kinase C (PKC) phosphorylation sites, we created a transgenic mouse expressing mutant TnI, in which PKC phosphorylation sites at serines-43 and -45 were replaced by alanine. When we used high-perfusate calcium as a PKC activator, developed pressures in transgenic (TG) perfused hearts were similar to wild-type (WT) hearts (P ⫽ not significant, NS), though there was a 35% and 32% decrease in peak-systolic intracellular calcium (P ⬍ 0.01) and diastolic calcium (P ⬍ 0.005), respectively. The calcium transient duration was prolonged in the TG mice also (12–27%, ANOVA, P ⬍ 0.01). During global ischemia, TG hearts developed ischemic contracture to a greater extent than WT hearts (41 ⫾ 18 vs. 69 ⫾ 10 mmHg, perfusate calcium 3.5 mM, P ⬍ 0.01). In conclusion, expression of mutant TnI lacking PKC phosphorylation sites results in a marked alteration in the calcium-pressure relationship, and thus susceptibility to ischemic contracture. The reduced intracellular calcium and prolonged calcium transients suggests that a potent feedback mechanism exists between the myofilament and the processes controlling calcium homeostasis. PROTEIN KINASE C (PKC) may have multiple and varied effects on myocyte function through phosphorylation of several intracellular sites, including L-type calcium channels (23), ATP-sensitive K⫹ (KATP) channels (14), and several myofilament proteins, including troponin I (TnI) (19, 29). Noland et al. (19) have shown in reconstituted myofilaments that PKC may mediate a reduction in the maximal calcium-stimulated ATPase rate of reconstituted actomyosin S-1, and apparent affinity of myosin S-1 for the thin filament. These effects are largely mediated through phosphorylation of serines-43 and -45 of TnI, and replacement of these with alanine results in nearcomplete preservation in ATPase activity in response to PKC. Also, Takeishi et al. (27) have demonstrated that in vivo phosphorylation of TnI by PKC decreases myofilament responsiveness to calcium and contractility. In hearts, in which the PKC sites are phosphorylated, it would be expected that the force generated (developed pressure) for a given level of intracellular calcium is reduced. Alteration in the force-calcium relationship may have several functional consequences. During ischemia there is a gradual increase in intracellular calcium and reduction in ATP, with ultimate development of ischemic contracture (25). PKC is activated during ischemia (1), and its effects on the force-calcium relationship mediated through TnI may protect against the development of contracture during states of high intracellular calcium. Another consequence of alteration in the force-calcium relationship may be an increase in energy utilization. When these PKC sites are phosphorylated, the maintenance of high calcium levels with reduced force would be expected to adversely effect the relationship between developed pressure and oxygen consumption, because cycling of calcium may use a significant proportion of ATP consumption and thus oxygen consumption (10). The present study examined the functional and energetic effects of PKC phosphorylation of serine residues 43 and 45 by generating a transgenic mouse Address for reprint requests and other correspondence: G. A. MacGowan, Cardiovascular Institute of the Univ. of Pittsburgh Medical Center, S550 Scaife Hall, 200 Lothrop St., Pittsburgh, PA 15213 (E-mail: [email protected]). The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked ‘‘advertisement’’ in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. calcium; ischemia http://www.ajpheart.org H835 Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 GUY A. MACGOWAN,1,4 CONGWU DU,3 DOUGLAS B. COWAN,7 CHRISTOF STAMM,7 FRANCIS X. MCGOWAN,7 R. JOHN SOLARO,6 ALAN P. KORETSKY,1,2,5 AND PEDRO J. DEL NIDO7 1 Pittsburgh Nuclear Magnetic Resonance Center for Biomedical Research, 2Department of Biological Sciences, and 3Center for Light Microscope Imaging and Biotechnology, Carnegie Mellon University, Pittsburgh 15213; 4Cardiovascular Institute of the University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania 15261; 5National Institute of Neurological Disease and Stroke, Bethesda, Maryland 20814; 6Department of Physiology and Biophysics, College of Medicine, University of Illinois, Chicago, Illinois 60612; and 7Harvard Medical School, Boston, Massachusetts 02115 H836 ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE expressing mutant TnI, in which these phosphorylation sites are replaced with alanine. METHODS Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 Generation of transgenic mice. All of the studies were performed in accordance with institutional guidelines. cDNA for mutant TnI, in which the PKC phosphorylation sites (serines-43 and -45) were replaced with alanine (19), was placed under the control of the cardiac-specific ␣-myosin heavy chain promoter (26). To generate transgenic mice, the transgene was microinjected into FVB zygotes with the use of standard methods (12). Microinjected embryos were reimplanted into pseudopregnant FVB female mice. By using the polymerase chain reaction (PCR) with the following primer sequences: CCG AGA TTT CTC CAT CCC AAG 5⬘ and GCA TCG CTG CTT TCA TCA GCC 3⬘, we detected the presence of mutant cardiac TnI transgene, making use of the heterologous junction between the myosin heavy chain promoter and TnI cDNA. RNA isolation and RT-PCR. Total RNA was isolated from mouse hearts using standard procedures, then digested with RQ1 RNase-free DNase (Promega) to remove any contaminating DNA. Spectrophotometric quantitation of purified RNA was confirmed visually by agarose-formaldehyde electrophoresis of RNA. RT-PCR was performed with the use of an Access System (Promega) with primer pairs designed to the cDNA sequences of mus musculus CD-1 cardiac TnI (Genbank Accession, U09181) and mouse G3PDH (Clontech). The CD-1 primers correspond to the 3⬘ end (⫹627 to ⫹607: AAACTTTTTCTTGCGGCCTTC) and the wild-type (AAGTCTAAGATCTCCGCCT) or mutant (AAGTCTAAGATCGCCGCCG) ⫹115 to ⫹133 region. We used 100 ng of purified total RNA for the reactions. The primer sets produced predicted product sizes of 512 bp for CD-1 and 452 bp for G3PDH. A linear range of amplification profile for each primer set was established on the basis of the following cycling parameters: reverse transcription step (1 cycle of 48°C for 45 min and 94°C for 2 min), PCR step (up to 40 cycles of 94°C for 30 s, 60°C for 60 s, and 68°C for 120 s), and extension step (1 cycle of 68°C for 7 min; 4°C soak). A midpoint of the linear amplification range was determined for CD-1 and G3PDH RT-PCR products to be at cycles 30 and 24, respectively. Negative controls included tubes that lacked RNA, avian myeloblastosis virus (AMV) reverse transcriptase, or Tfl DNA polymerase. The identity of each PCR product was confirmed by ligating the DNA fragments into the PCRII vector (Invitrogen) and sequencing these by using standard molecular biology techniques. Equal volumes of amplified products were loaded in each lane of a 1% Tris, acetic acid, and EDTA (TAE)-buffered agarose gel and electrophoresed with the 100-bp ladder (Life Technologies). The results are not strictly semiquantitative; however, care was taken to assure that starting total RNA amounts were the same for each sample and the cycling parameters were adjusted for each primer pair to ensure PCR was stopped during the linear segment of the amplification profile. All samples contained an equal amount of G3PDH amplification product (not shown). Immunoblot analyses. Hearts were snap-frozen in liquid nitrogen and stored at ⫺80°C. To determine total cardiac TnI levels, proteins were isolated from the frozen hearts by Dounce homogenization in a small volume of ice-cold lysis solution, consisting of 150 mM NaCl, 20 mM Tris 䡠 HCl pH 7.6, 1 mM EDTA, 0.5% sodium deoxycholate, 70 mM NaF, 1% Nonidet P-40, a protease inhibitor cocktail (Complete; Boehringer Mannheim), 200 M sodium orthovanadate, and 2 M phenylmethylsulfonyl fluoride (PMSF). Debris was pelleted and the supernatants were stored at ⫺80°C. Protein concentrations were established using the Pierce BCA protein determination kit. SDS-PAGE and transfer to nitrocellulose were performed by using standard procedures, and identical gels were stained with Coomassie brilliant blue R250 to confirm equal protein loading. Nitrocellulose membranes were rinsed in Tris-buffered saline pH 7.4 containing 0.1% Tween 20 (TBS-T) and blocked in 5% nonfat milk; TBS-T for 1 h at 22°C on a rocking platform. Membranes were rinsed four times in TBS-T then incubated overnight at 4°C on an orbital shaker with primary antibodies diluted in TBS-T. The anti-human cardiac-specific TnI monoclonal antibodies (either 3314 11E1.3 or 3350 2F6.6, a gift from Dr. Jack Ladenson, Washington University, St. Louis, MO) were used at a final concentration of 1 g/ml and found to react equally well. The primary antibody was detected with horseradish peroxidase-conjugated anti-mouse secondary antibody and the ECL kit (Amersham) according to the manufacturer’s directions before exposure to X-Omat AR film (Kodak). Experimental design and isolated perfused mouse heart studies. Because calcium-induced inotropy is partly mediated by PKC (15, 17), high calcium was used as an activator of protein kinase C. In other studies, global ischemia, which is also associated with high calcium (25) and PKC activation (1), was used. Anesthesia was induced with 1.5–3.0 mg of intraperitoneal pentobarbital sodium, and the animal was anticoagulated with 100 units of heparin sodium. Hearts were gravity perfused with a perfusion pressure of 55 mmHg and stimulated at the physiological mouse heart rate of 8 Hz. Left ventricular pressure was measured with a balloon within the left ventricle. The left ventricular diastolic pressure was set at 0–10 mmHg with the use of a microsyringe. The modified Krebs solution used consisted of 113 mM NaCl, 4.7 mM KCl, 1.2 mM MgSO4, 0.5 mM Na-EDTA, 28.0 mM NaHCO3, 5.5 mM glucose, 5.0 mM pyruvate, 2.5 mM CaCl2, and 50 M octanoate. The solution was oxygenated with 95% O2-5% CO2 and pH adjusted to 7.4. In some studies, perfusate calcium was increased to 3.5 mM, and therefore the concentration of NaCl was adjusted accordingly to maintain osmolarity. To eliminate the effects of cathecholamine release by pacing, 0.1 M esmolol (DuPont; Wilmington, DE) was added to the perfusate. In a subgroup of experiments myocardial oxygen consumption was measured. The perfused mouse heart was placed in a glass, water-jacketed chamber, which was sealed at the top. Myocardial oxygen consumption was determined from influent and effluent oxygen content measured by a blood gas analyzer (model 30; ABL, Copenhagen, Denmark) and flow rate. Ischemia experiments. In another group of experiments, hearts were perfused as described above for a baseline period of 10 min and then underwent 15 min of global no-flow ischemia, followed by 20 min of reperfusion. To determine that PKC-⑀ translocated during ischemia, hearts were exposed to the same ischemic conditions and time as above and then flash frozen in liquid nitrogen and compared with control hearts not exposed to ischemia. Left ventricular tissue was homogenized in ice-cold buffer containing 20 mM Tris 䡠 HCl, 2 mM EDTA, 0.5 mM EGTA, 1 mM PMSF, 25 g/ml leupeptin, 0.3 mM sucrose at pH 7.4 and centrifuged at 1,000 g for 5 min to remove tissue debris. Cytosolic and particulate fractions were separated by ultracentrifugation of the supernatant (100,000 g for 60 min). The resulting supernatant (cytosolic fraction) was collected, and the pellet (particulate fraction) was resuspended in sucrose-free buffer containing 1% Triton X, incubated for 60 min at 4°C, and ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE RESULTS Description of mice. All studies were performed in isolated perfused mouse hearts from transgenic mice and FVB age-matched controls. Mice were aged between 8 and 40 wk. All experiments were done in males, except for three females in the wild-type group, and one female in the transgenic group. Founders 2, 7, and 9 were identified as the highest expressers by mRNA levels. In founders 2 and 7 amounts of wild-type and mutant mRNA were approximately equal, and in Fig. 1. Agarose gel of RT-PCR products from wild-type (WT) and transgenic (TG) mice. Lanes 2–5 are from 2 WT controls, lanes 6 and 7 from founder 2 (m2), lanes 8 and 9 from founder 7 (m7), and 10 and 11 from founder 9 (m9). ⫹, WT mRNA and ⫺, mutant mRNA. In founders 2 and 7 amounts of mutant and WT mRNA are approximately equal, and in founder 9 mutant mRNA is less than in WT mice. cTnI, cardiac troponin I; bp, base pair. Fig. 2. A representative immunoblot of total cTnI levels from WT and TG mice. Lanes 1 and 2 are from 2 WT controls, lane 3 from m2, lane 4 from m7, and lane 5 from m9. founder 9 the amount of mutant mRNA was less than wild-type mRNA (Fig. 1). In preliminary studies no functional differences were noted between these founders in terms of developed pressures, heart-tobody weight ratios, ischemic contracture pressure, myocardial oxygen consumption, or intracellular calcium (data not shown). All of the founders were used in the ischemia experiments, and founder 7 was used for the myocardial oxygen consumption and founder 9 for the intracellular calcium experiments. TnI antibodies did not selectively identify the mutant protein from wild-type mice, though total immunoreactive TnI was similar in wild-type and transgenic mice (Fig. 2), suggesting that the total amount of TnI was closely regulated, and that any excess protein was degraded. Mice expressing mutant TnI appeared normal, and there was no significant difference in heart-to-body weight ratios (Table 1). Also, systolic and diastolic pressures were not significantly different between transgenic and wild-type mice (Table 1), and histology revealed no abnormalities in transgenic mouse hearts (Fig. 3). Intracellular calcium. Systolic and diastolic intracellular calcium was significantly lower in transgenic mice (ANOVA, P ⱕ 0.001). Levels of intracellular calcium were reduced by 35% and 32% at peak systole and diastole, respectively, at perfusate calcium of 3.5 mM (Table 2, and Fig. 4). Developed pressure was not significantly different between wild-type and controls, indicating that the pressure-calcium relationship in the transgenic mice was significantly altered compared with controls. The duration of the calcium transient (measured from the initial increase in intracellular calcium to 90% of return to baseline) was increased by 27% in the transgenic mice at perfusate calcium 2.5 mM, and 12% at perfusate calcium 3.5 mM (ANOVA, P ⬍ 0.01). Further information regarding the pressure-calcium relationship was obtained from pressure-calcium plots (Fig. 4). These were created from simultaneous pressure and calcium (derived from fluorescence) measurements, averaged over five to seven cardiac cycles. Consistent with the altered pressure-calcium relationship, pressure at the peak of the calcium transient was increased in the transgenic mice despite the prolongation of the calcium transient. The subsequent slope of calcium decay versus pressure (taken from peak calcium to peak pressure) was decreased in the transgenic mice reflecting both the prolonged calcium Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 centrifuged at 40,000 g for 15 min. SDS-PAGE and transfer to nitrocellulose was performed as described above. The membranes were incubated with a rabbit polyclonal antibody raised against murine PKC-⑀ (Upstate) at 1 g/ml and detected with a horseradish peroxidase-conjugated anti-rabbit secondary antibody and the ECL kit (Amersham). After exposure to film, quantitative protein analysis was performed by laser densitometry. Measurement of intracellular calcium in whole perfused mouse hearts with rhod 2. The methods used to measure intracellular calcium with rhod 2 (Molecular Probes, Eugene, OR) in perfused hearts have been previously extensively described (7, 8). Excitation at 524 nm and emission at 589 nm was used for fluorescence measurements. We quantified the relative amount of rhod 2 in the heart with the use of absorbance measurements, by taking the ratio of absorbance at 524 nm (rhod-2 sensitive) to 589 nm (rhod-2 insensitive). This procedure eliminated the effect of motion and scattering changes because both are equally affected by motion and concentration, though only 524 reflects the concentration of rhod 2 (7, 8). Rhod 2 (100 g) was dissolved with 4 l of DMSO and 200 l of H2O and loaded through the coronary perfusate. At the end of the perfusion protocol, maximal fluorescence, used in the calculation of intracellular calcium concentration, was determined by tetanizing the heart with a 20 mM bolus of calcium chloride and 10 M of cyclopiazonic acid (Sigma Chemical), which is a potent inhibitor of Ca2⫹ATPase (3). Statistical analysis. Unpaired comparisons were performed using Student’s t-test, and when multiple comparisons were made, we used ANOVA with the Scheffé’s test for subgroup analysis. Data are expressed as means ⫾ SD. H837 H838 ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE Table 1. Heart and body weights, systolic and diastolic pressures, peak positive and negative dP/dt, coronary flow and myocardial oxygen consumption in all hearts from wild-type and transgenic mice Perfusate Calcium, mM WT (n ⫽ 32) TG (n ⫽ 30) 2.5 Body weight, g Heart weight, g Heart-to-body weight ratio Systolic pressure, mmHg Diastolic pressure, mmHg ⫹dP/dt, mmHg/s ⫺dP/dt, mmHg/s Coronary flow, ml/min MV̇O2, mol 䡠 min⫺1 䡠 g dry wt⫺1 Developed pressure/MV̇O2 58 ⫾ 6 4⫾3 2,296 ⫾ 280 1,600 ⫾ 306 2.2 ⫾ 0.2 42.2 ⫾ 4.3† 1.27 ⫾ 0.13 3.5 30.7 ⫾ 3.2 0.161 ⫾ 0.020 0.0049 ⫾ 0.0003 66 ⫾ 7 3⫾3 2,764 ⫾ 315 1,836 ⫾ 403 2.2 ⫾ 0.4 48.9 ⫾ 6.1† 1.28 ⫾ 0.11 2.5 3.5 31.7 ⫾ 3.1 0.156 ⫾ 0.017 0.0050 ⫾ 0.0003 58 ⫾ 6 69 ⫾ 7 4⫾4 4⫾3 2,322 ⫾ 287 2,879 ⫾ 234 1,609 ⫾ 154 1,905 ⫾ 191 2.3 ⫾ 0.4 2.2 ⫾ 0.5 38.4 ⫾ 3.6† 44.1 ⫾ 4.4† 1.41 ⫾ 0.14 1.47 ⫾ 0.15* transient and altered pressure-calcium relationship (Table 2, Fig. 4). Myocardial oxygen consumption. Myocardial oxygen consumption was measured as a decrease in calcium Fig. 3. Histology (hematoxylin and eosin) of WT (A) and TG (B) at ⫻40 magnification. Normal histology is seen in the TG mice. cycling that may result in a decrease in myocardial oxygen consumption. There was a significant reduction in myocardial oxygen consumption in transgenic mice compared with wild-type mice (ANOVA, P ⬍ 0.01; Table 1). Developed pressures were not significantly different between the two groups, though the ratio of developed pressure to myocardial oxygen consumption [in mmHg/(mol 䡠 min⫺1 䡠 g dry wt⫺1)], an index of energetic efficiency, was significantly higher in the transgenic mice at perfusate calcium of 3.5 mM (P ⬍ 0.05). Ischemia and reperfusion. Figure 5A shows representative Western immunoblots with translocation of PKC-⑀ to the particulate fraction after 15 min of ischemia in both wild-type and transgenic mice, and Fig. 5B demonstrates the laser densitometry quantification of PKC-⑀ content in fractionated tissue with significant (P ⬍ 0.05, n ⫽ 6 measurements per group) increase in the particulate fraction after 15 min of ischemia in both wild-type and transgenic mice. Examples of pressure tracings during the development of ischemic contracture are shown in Fig. 6, and mean values are shown in Fig. 7 (perfusate calcium 2.5 mM) and Fig. 8 (perfusate calcium 3.5 mM), which demonstrate the more marked development of ischemic contracture in the transgenic mice and elevation of diastolic pressures in the early reperfusion period. In addition to the data presented in Figs. 7 and 8, at perfusate calcium of 2.5 mM the time to development of ischemic contracture (increase in diastolic pressure 5 mmHg over baseline) was not significantly different between the two groups (wild type, 603 ⫾ 200 vs. transgenic, 491 ⫾ 137 s; P ⫽ not significant, NS), though at perfusate calcium 3.5 mM ischemic contracture pressure developed earlier (wild-type, 635 ⫾ 86 vs. transgenic, 425 ⫾ 84 s; P ⬍ 0.005) in the transgenic mice. During reperfusion at perfusate calcium 2.5 mM, diastolic pressures rose to a maximum of 30 ⫾ 13 mmHg at 308 ⫾ 92 s postreperfusion in transgenic mice compared with 14 ⫾ 7 mmHg (P ⬍ 0.001) at 271 ⫾ Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 Values are means ⫾ SD; n ⫽ no. of hearts. MV̇O2, myocardial oxygen consumption; WT, wild type; TG, transgenic. Heart and body weight ratios were not obtained in the fluorescence experiments because the tetanization procedure distorts heart weight, and the first derivative of pressure (dP/dt) was determined in a subgroup of 10 WT and 8 TG perfused hearts. MV̇O2 was determined in a subgroup of WT (n ⫽ 9) and TG (n ⫽ 9) hearts. Functional data were obtained at perfusate calcium 2.5 and 3.5 mM. * P ⬍ 0.05 vs. WT; † P ⬍ 0.01 ANOVA: WT vs. TG combining perfusate 2.5 and 3.5 mM data. H839 ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE Table 2. Developed pressure, intracellular calcium, calcium transient duration, and calcium-pressure relations at perfusate calcium 2.5 and 3.5 mM from wild type and transgenic mice Perfusate Calcium, mM WT Developed pressure, mmHg Peak [Ca2⫹]i, nM Diastolic [Ca2⫹]i, nM ⌬[Ca2⫹]i, nM t90%, ms Pressure at peak [Ca2⫹]i, mmHg [Ca2⫹]i decay/pressure slope, nM/mmHg TG 2.5 (n ⫽ 5) 3.5 (n ⫽ 4) 2.5 (n ⫽ 5) 3.5 (n ⫽ 5) 56 ⫾ 8 800 ⫾ 97 508 ⫾ 49 292 ⫾ 71 65 ⫾ 10d 9 ⫾ 2d ⫺5.0 ⫾ 1.7 62 ⫾ 7 1,155 ⫾ 274 634 ⫾ 111 521 ⫾ 177 70 ⫾ 10d 10 ⫾ 4d ⫺6.6 ⫾ 1.4 53 ⫾ 3 610 ⫾ 85 391 ⫾ 36 218 ⫾ 58 85 ⫾ 15d 15 ⫾ 3d ⫺3.1 ⫾ 1.0 60 ⫾ 5 749 ⫾ 106a 427 ⫾ 64b 321 ⫾ 56c 80 ⫾ 5d 17 ⫾ 5d ⫺4.0 ⫾ 0.4e 71 s (P ⫽ NS) in controls. At perfusate calcium of 3.5 mM there was marked elevation of diastolic pressures in both wild-type and transgenic mice at 5 of min postreperfusion, although this was not significantly different between wild-type and transgenic mice. DISCUSSION In transgenic mice that express mutant TnI lacking functional PKC phosphorylation sites, there is a marked reduction in both systolic and diastolic levels of intracellular calcium at similar developed pressures indicating an altered pressure-calcium relation in the transgenic hearts. There is also significant prolongation of the duration of the calcium transient. These transgenic mice are susceptible to global ischemia with more rapid and extensive development of ischemic contracture and postischemic dysfunction, most likely because of the inability of PKC to phosphorylate TnI and decrease the force-calcium relation. Finally, these mice have a significantly elevated ratio of developed pressure to myocardial oxygen consumption at high-perfusate calcium, which may signify an energetic benefit of decreased calcium cycling. These findings are from perfused hearts at high-perfusate calcium (3.5 mM) (17) or during global ischemia (1), which have been used to activate PKC. We have previously demonstrated in this perfused mouse heart model that the selective PKC antagonist chelerythrine can inhibit calcium-induced inotropy, suggesting that PKC is activated by high-perfusate calcium (15). Altered pressure-calcium relationship in the perfused mouse heart. On the basis of in vitro studies demonstrating a reduction in maximal calcium-stimulated ATPase activity produced by PKC phosphorylation of TnI (19), an alteration in the pressure-calcium relationship is predicted in these mice. Though this prediction is clearly demonstrated, the surprising finding is that developed pressure is not increased but normal in Fig. 4. Intracellular calcium and calcium-pressure relations from WT (A and B) and TG (C and D) mice. Reduced levels of intracellular calcium at perfusate calcium 3.5 mM and prolonged calcium transients are seen in the TG mice. Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 Values are means ⫾ SD; n, no. of mice in each group. ⌬[Ca2⫹]i, change in intracellular Ca2⫹ concentration. t90%, duration of Ca2⫹ transient (measured from initial increase in intracellular Ca2⫹ to 90% return to baseline. a P ⬍ 0.01 vs. WT 3.5 mM; b P ⬍ 0.005 vs. WT 3.5 mM; c P ⫽ 0.05 vs. WT 3.5 mM; d P ⬍ 0.01 ANOVA: WT vs. TG combining perfusate 2.5 and 3.5 mM data, and e P ⬍ 0.05 vs. WT 3.5 mM. H840 ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE Fig. 5. A: representative Western immunoblots demonstrating translocation of protein kinase C (PKC-⑀) to the particulate fraction during 15-min ischemia in WT and TnI mutant mice. B: laser densitometry quantification of PKC-⑀ content in fractionated tissue samples. Bars represent means ⫾ SD of 6 measurements per group. Solid bars, WT mice. Open bars, TnI mutant mice. *P ⬍ 0.05 vs. no ischemia. these mice. The markedly reduced intracellular calcium levels indicate that the transgenic heart has adapted to the increased calcium sensitivity by decreasing the calcium transient, suggesting there is direct feedback from the myofilament to the processes controlling calcium homeostasis. This is further suggested by the prolongation of the calcium transient duration, which is seen at both levels of perfusate calcium. A precedent for such an effect may be seen in congestive heart failure. It has been well described that in heart muscle from patients with congestive heart failure there are alterations in calcium handling, with prolongation in calcium transients and increased diastolic levels of intracellular calcium with higher levels of perfusate calcium (11). However, Perez et al. (20) have recently studied the role of calcium cycling versus myofilament dysfunction in the spontaneous hypertension and heart failure rat model. They also demonstrated slowing of calcium cycling, but a much greater reduction in maximal calcium activated force. Their analysis revealed that the slowing of calcium cycling prolonged the time available for calcium to activate the contractile apparatus, as a compensatory response to reduced myofilament function. Thus myofilament function may be able to effect calcium cycling, a possible explanation for the reduced calcium levels and prolonged transients seen in the present study. The mechanism for the feedback from myofilament dysfunction to altered calcium cycling is not known. Minamisawa et al. (18) have recently shown that phospholamban ablation reverses the dilated cardiomyopathy phenotype of the mouse deficient in the Lin-11, Isl-1, and Mec-3 (LIM) cytoskeletal protein. It would be Fig. 7. Systolic and diastolic pressures at baseline, ischemia, and during reperfusion for WT and TG mice at perfusate calcium 2.5 mM. WT, n ⫽ 7; TG, n ⫽ 8; *P ⬍ 0.05 WT vs. TG. Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 Fig. 6. Examples of pressure tracings (slow time based) during development of ischemic contracture in WT (A) and TG (B) mice; perfusate calcium 3.5 mM. Arrows indicate time to development of ischemic contracture, an increase in diastolic pressure of 5 mmHg above baseline, which was earlier in TG mice at perfusate calcium 3.5 mM. In the early reperfusion period, diastolic pressures increase to a greater extent in the TG mice. ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE interesting to study sarcoplasmic reticulum regulatory proteins in these transgenic mice. An alternative explanation may relate to levels of intracellular calcium during altered calcium sensitivity. The magnitude of the measured calcium transient is dependent on the amount of calcium released and taken up from the sarcoplasmic reticulum and the amount of calcium that binds to cytosolic proteins, including troponin C. An increase in the calcium sensitivity of troponin C to calcium would decrease the amount of calcium available for binding to the calciumsensitive probe rhod 2, resulting in a reduced calcium transient. This assumes that troponin C is the only major calcium sequestering site in the myocyte. Such effects have been demonstrated in experiments studying the effects of muscle length, which alters the binding constant for troponin C for calcium (2, 13). Whether this applies to alterations in maximal actomyosin ATPase activity is unclear, and furthermore a reduction in diastolic values as seen in the present study may not be consistent with this effect. Ischemia-reperfusion. Ischemia is associated with a progressive rise in intracellular calcium (25) and activation of PKC (1), which we have confirmed in this perfused mouse heart model. The resulting phosphorylation of PKC sites on TnI is expected to reduce maximal ATPase activity, which may protect against the development of ischemic contracture. Thus we predicted that these transgenic mice would be susceptible to development of ischemic contracture, and that this effect would be greater with higher levels of perfusate calcium. The effects of PKC on actomyosin ATPase activity are greater during acidosis (as is expected in global ischemia), and this may explain why marked differences were seen at 2.5 mM perfusate calcium in the ischemia experiments, though differences were less marked in the intracellular calcium or myocardial oxygen consumption experiments at the same perfusate calcium. Importantly, this effect is not a nonspecific effect of overexpression of TnI, because total TnI levels in wild-type and transgenic mice are similar. Whereas the experiments studying intracellular calcium levels were performed during normoxia, the altered pressurecalcium relationship is a plausible explanation of the predisposition to ischemic contracture. The resulting profound postischemic dysfunction in the transgenic mice is partly related to the preceding ischemic contracture, so the contribution of the mutant protein to the postischemic dysfunction is not clear. Also, ischemia-reperfusion injury may result in TnI degradation (9, 16), although it is not known if there is increased selective breakdown of the mutant TnI that might also predispose the transgenic mice to reperfusion injury. Energetic effects of mutant TnI. Recent studies have demonstrated that calcium cycling may account for a significant proportion of the energy consumption (thus oxygen consumption) of the heart. For instance, in the perfused rat heart, Grandis et al. (10) have compared the inotropic and energetic effects of the calcium-sensitizing agent EMD-57033, and the -adrenergic agonist dobutamine. Whereas dobutamine produces a positive inotropic effect by increasing the amplitude of the calcium transient (22), EMD-57033 does not increase calcium cycling (24). At doses chosen to result in equal increases in developed pressure, there was a marked increase in myocardial oxygen consumption with dobutamine, though only a small increase in myocardial oxygen consumption with EMD-57033, not significantly different from control. Similar results have also been obtained in isolated myocyte studies (21). Thus we predicted that in these transgenic mice with reduced calcium cycling that myocardial oxygen consumption would be also reduced. Consistent with this, the reduced calcium transient and energetic advantage (developed pressure/myocardial oxygen consumption, Table 1) are both seen only with high-perfusate calcium. Recently, Brandes and Bers (4) have analyzed the contribution of mechanical work and calcium cycling to total mitochondrial ATP hydrolysis as measured by NADH levels by using fluorescent spectroscopy of rat cardiac trabeculas. They concluded that there was an equal contribution of mechanical work and calcium cycling to total ATP hydrolysis. Thus, given a 35% reduction in peak systolic calcium in the present study of transgenic mice, a 17.5% reduction in ATP hydrolysis would be expected, which compares favorably to the measured 15% reduction in the ratio of developed pressure to myocardial oxygen consumption. Limitations. We do not know the wild-type-to-mutant protein ratio in transgenic mice because the TnI antibodies did not selectively recognize mutant protein. This uncertainty makes it difficult to assess whether the phenotype demonstrated is a result of the mutant protein, or whether it is also an effect of the mutant protein on wild-type protein function. However, we do know that in two of the three transgenic lines used in these experiments that the ratio of mutant to wild-type mRNA is ⬃50:50. Nevertheless, Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 Fig. 8. Systolic and diastolic pressures at baseline, ischemia, and during reperfusion for WT and TG mice at perfusate calcium 3.5 mM. WT, n ⫽ 6; TG, n ⫽ 6; **P ⬍ 0.01 WT vs. TG. H841 H842 ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE This work was supported by American Heart Association (Pennsylvania Affiliate) Grant-in-Aid Beginning (B98452P) and National Heart, Lung, and Blood Institute Grants HL-03826 (to G. A. MacGowan), HL-40354 (to A. P. Koretsky), HL-46207 (to P. J. del Nido), HL-52589 (to F. X. McGowan), and R37 HL-22231 (to R. J. Solaro). The Pittsburgh NMR Center for Biomedical Research was awarded National Institutes of Health Grant RR-03631. REFERENCES 1. Albert CJ and Ford DA. Protein kinase C translocation and PKC-dependent protein phosphorylation during myocardial ischemia. Am J Physiol Heart Circ Physiol 276: H642–H650, 1999. 2. Allen DG and Kurihara S. The effects of muscle length on intracellular calcium transients in mammalian cardiac muscle. J Physiol (Lond) 327: 79–94, 1982. 3. Backx PH, Gao WD, Azan-Backx M, and Marban E. The relationship between contractile force and intracellular [Ca2⫹] in intact rat cardiac trabeculae. J Gen Physiol 105: 1–19, 1998. 4. Brandes R and Bers DM. Analysis of mechanisms of mitochondrial NADH regulation in cardiac trabeculae. Biophys J 77: 1666–1682, 1999. 5. Brooks WW and Apstein CS. Effect of Treppe on isovolumic function in the isolated blood-perfused mouse heart. J Mol Cell Cardiol 28: 1817–1822, 1996. 6. Chomczynski P and Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem 162: 156–159, 1987. 7. Del Nido PJ, Glynn P, Buenaventura P, and Koretsky AP. Fluorescence measurement of calcium transients in perfused rabbit heart using rhod 2. Am J Physiol Heart Circ Physiol 274: H728–H741, 1998. 8. Du C, MacGowan GA, Farkas DL, and Koretsky AP. Quantitative measurement of calcium transients in perfused mouse hearts using rhod-2 fluorometry. Proc SPIE 3602: 214–219, 1999. 9. Gao WD, Atar D, Liu Y, Perez NG, Murphy AM, and Marban E. Role of troponin I proteolysis in the pathogenesis of stunned myocardium. Circ Res 80: 393–399, 1997. 10. Grandis DJ, del Nido PJ, and Koretsky AP. Functional and energetic effects of the inotropic agents EMD-57033 and BAPTA on the isolated rat heart. Am J Physiol Cell Physiol 269: C472– C479, 1995. 11. Gwathmey JK, Copelas L, MacKinnon R, Schoen FJ, Feldman MD, Grossman W, and Morgan JP. Abnormal intracellular calcium handling from patients with end-stage heart failure. Circ Res 61: 70–76, 1987. 12. Hogan B, Constantini F, and Lacy L. Manipulating The Mouse Embryo: A Laboratory Manual. Plainview, NY: Cold Spring Harbor Lab, 1986. 13. Lab MJ, Allen DG, and Orchard CH. The effects of shortening on myoplasmic calcium concentration and on the action potential in mammalian ventricular muscle. Circ Res 55: 825–829, 1984. 14. Light PE, Sabir AA, Allen BG, Walsh MP, and French RJ. Protein kinase C-induced changes in the stoichiometry of ATP binding activate cardiac ATP-sensitive K⫹ channels. Circ Res 79: 399–406, 1996. 15. MacGowan GA and Koretsky AP. Effects of protein kinase C inhibition during calcium induced inotropy in the isolated perfused mouse heart (Abstract). J Am Coll Cardiol 31: 288A, 1998. 16. McDonough JL, Arrell D, and Van Eyk JE. Troponin I degradation and covalent complex formation accompanies myocardial ischemia/reperfusion injury. Circ Res 84: 9–20, 1999. 17. Meldrum DR, Cleveland JC, Rowland RT, Banerjee A, and Harken AH. Calcium-induced inotropy is in part mediated by protein kinase C. J Surg Res 63: 400–405, 1996. 18. Minamisawa S, Hoshijima M, Chu G, Ward CA, Frank K, Gu Y, Martone ME, Wang Y, Ross J Jr, Kranias EG, Giles WR, and Chien KR. Chronic phospholamban-sarcoplasmic reticulum calcium ATPase interaction is the critical calcium cycling defect in dilated cardiomyopathy. Cell 99:313–322, 1999. 19. Noland TA, Guo X, Raynor RL, Jideama NM, AveryhartFullard V, Solaro RJ, and Kuo JF. Cardiac troponin I mutants. Phosphorylation by protein kinases C and A and regulation of Ca2⫹-stimulated MgATPase of reconstituted actomyosin S-1. J Biol Chem 270: 25445–25454, 1995. 20. Perez NG, Hashimoto K, McCune S, Altschuld RA, and Marban E. Origin of contractile dysfunction in heart failure. Calcium cycling versus myofilaments. Circulation 99: 1077– 1083, 1999. 21. Popping S, Fischer MY, Ionescu I, Kammermeier H, and Rose H. Economy of contraction of cardiomyocytes as influenced by different positive inotropic interventions. Am J Physiol Heart Circ Physiol 271: H357–H364, 1996. 22. Ruffolo RR. Dobutamine: review of pharmacology. Am J Med Sci 294: 244–248, 1987. 23. Shistik E, Ivanina T, Blumenstein Y, and Dascal N. Crucial role of N terminus in function of cardiac L-type Ca2⫹ channel Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017 transgenic techniques that change the endogenous gene would avoid this uncertainty relating to the efficiency of mutant protein production. Also, total TnI levels including mutant and wild-type proteins are similar in wild-type and transgenic mice, so the results presented are not the result of overexpression of TnI. All of the the experiments in the current study are performed in isolated isovolumically contracting hearts, and it must be recognized that this experimental preparation may produce different results to ejecting, or in vivo preparations. Nevertheless, in the present study, the data regarding developed pressure, myocardial oxygen consumption, and intracellular calcium are all derived from the same experimental methods, i.e., the perfused mouse heart, allowing correlations between these data. Also, we have used the physiological heart rate of 8 Hz. Because the mouse has a negative force-frequency relationship (5), higher pressures and altered calcium levels at lower stimulation rates may be expected. With respect to rhod 2 measurements of intracellular calcium, other investigators using myocyte studies and different loading procedures to those described in the present study have used rhod 2 as an indicator of mitochondrial calcium (28). Though we cannot exclude a small proportion of rhod 2 leaking into organelles, we have previously shown that there is predominant cytosolic localization of rhod 2 (7, and unpublished data by MacGowan and Koretsky). The differences in rhod 2 localization probably relate to different loading conditions used by different investigators. In conclusion, transgenic mice expressing mutant TnI lacking PKC phosphorylation sites have markedly diminished levels of intracellular calcium levels and prolonged calcium transients, but have normal developed pressures under conditions that activate PKC. This altered pressure-calcium relationship is associated with a predisposition to development of ischemic contracture, and a reduced energetic cost of calciuminduced inotropy. These studies demonstrate that in vivo phosphorylation of TnI by PKC can have marked effects on myocyte function and energetics during ischemia and normoxia. Furthermore, the presence of reduced intracellular calcium levels and prolonged calcium transients suggests a potent interaction between the myofilament and the processes that control calcium homeostasis. ISCHEMIC DYSFUNCTION IN TROPONIN I TRANSGENIC MICE and its modulation by protein kinase C. J Biol Chem 273: 17901–17909, 1998. 24. Solaro RJ, Gambassi G, Warshaw DM, Keller MR, Spurgeon HA, Beier N, and Lakatta EG. Stereoselective actions of thiadiazinones on canine cardiac myocytes and myofilaments. Circ Res 73: 981–990, 1993. 25. Steenbergen C, Murphy E, Watts JA, and London RE. Correlation between cytosolic free calcium, contracture, ATP, and irreversible ischemic injury in perfused rat heart. Circ Res 60: 135–146, 1990. 26. Subramaniam A, Jones WK, Gulick J, Wert S, Neumann J, and Robbins J. Tissue-specific regulation of the ␣-myosin heavy chain gene prometer in transgenic mice. J Biol Chem 266: 24613–24620, 1991. H843 27. Takeishi Y, Chu G, Kirkpatrick DM, Li Z, Wakasaki H, Kranias EG, King GL, and Walsh RA. In vivo phosphorylation of cardiac troponin I by protein kinase C2 decreases cardiomyocyte calcium responsiveness and contractility in transgenic mouse hearts. J Clin Invest 102: 72–78, 1998. 28. Trollinger DR, Cascio WE, and Lemasters JJ. Selective loading of rhod-2 into mitochondria shows Ca2⫹ transients during the contractile cycle in adult rabbit cardiac myocytes. Biochem Biophys Res Commun 236: 738–742, 1997. 29. Venema RC and Kuo JF. Protein kinase C-mediated phosphorylation of troponin I and C protein in isolated myocardial cells is associated with inhibition of myofibrillar actomyosin MgATPase. J Biol Chem 268: 2705–2711, 1993. Downloaded from http://ajpheart.physiology.org/ by 10.220.33.2 on June 12, 2017
















![Poster ECE`14 PsedohipoPTH [Modo de compatibilidad]](http://s1.studyres.com/store/data/007957322_1-13955f29e92676d795b568b8e6827da6-150x150.png)