* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Signaling Proteins Regulated by Suppressor of Cytokine Immune
Drosophila melanogaster wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Innate immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
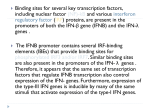
This information is current as of June 12, 2017. IFN-α-Induced Signal Transduction, Gene Expression, and Antitumor Activity of Immune Effector Cells Are Negatively Regulated by Suppressor of Cytokine Signaling Proteins Jason M. Zimmerer, Gregory B. Lesinski, Sri Vidya Kondadasula, Volodymyr I. Karpa, Amy Lehman, Abhik RayChaudhury, Brian Becknell and William E. Carson III References Subscription Permissions Email Alerts This article cites 65 articles, 30 of which you can access for free at: http://www.jimmunol.org/content/178/8/4832.full#ref-list-1 Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 J Immunol 2007; 178:4832-4845; ; doi: 10.4049/jimmunol.178.8.4832 http://www.jimmunol.org/content/178/8/4832 The Journal of Immunology IFN-␣-Induced Signal Transduction, Gene Expression, and Antitumor Activity of Immune Effector Cells Are Negatively Regulated by Suppressor of Cytokine Signaling Proteins1 Jason M. Zimmerer,*† Gregory B. Lesinski,† Sri Vidya Kondadasula,† Volodymyr I. Karpa,† Amy Lehman,‡ Abhik RayChaudhury,§ Brian Becknell,† and William E. Carson III2†¶ R ecombinant IFN-␣ is used to treat patients with metastatic malignant melanoma and is associated with an overall response rate of 10 –15% (1–3). High-dose IFN-␣ is also used as an adjuvant in patients who have undergone resection of high-risk lesions (nodal disease or primary tumors of Breslow thickness ⬎4 mm) (1, 3– 6). However, it has been difficult to determine the optimal dose of IFN-␣ for melanoma patients or devise strategies to enhance the antitumor effects of IFN-␣ because its cellular targets and mechanism of action are largely unknown. Although exogenous administration of IFN-␣ can act directly on melanoma cells to inhibit proliferation and up-regulate the expression of MHC class I Ags, its stimulatory properties on effector cells of the immune system are thought to be critical for its antitumor activity (7–10). Dunn et al. (11) have also shown that endogenously produced IFN-␣ is required for the prevention of carcinogen-induced tumors and that host immune effector cells are critical targets of IFN-␣ during the development of protective antitumor responses. *Integrated Biomedical Sciences Graduate Program, †Human Cancer Genetics Program, Department of Molecular Virology, Immunology, and Medical Genetics, ‡Center for Biostatistics, §Department of Pathology, ¶Department of Surgery, The Ohio State University, Columbus, OH 43210 Received for publication August 31, 2006. Accepted for publication January 30, 2007. The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. 1 This work was supported by a seed grant from the Immunology Program of The Ohio State University-Comprehensive Cancer Center and the Harry J. Lloyd Charitable Trust (to G.B.L.) and National Institutes of Health Grants P01 CA95426, K24 CA93670 (to W.E.C.), and P30 CA16058. 2 Address correspondence and reprint requests to Dr. William E. Carson III, Department of Surgery, The Ohio State University, N924 Doan Hall, 410 West 10th Avenue, Columbus, OH 43210. E-mail address: [email protected] www.jimmunol.org The receptor for IFN-␣ is widely expressed on both tumor cells and immune effector cells (8, 12). Binding of IFN-␣ to its receptor activates Jak1 and tyrosine kinase 2, which in turn phosphorylate tyrosine residues within the cytoplasmic region of the receptor. These phosphotyrosine residues provide docking sites for STAT1 and STAT2, latent cytoplasmic transcription factors that are phosphorylated by the Jaks (13). The prototypical IFN-␣-signaling reaction results in the formation of IFN-stimulated gene factor 3, a DNA-binding complex that consists of STAT1␣ (or STAT1), STAT2, and IFN regulatory factor 9 (14). IFN-stimulated gene factor 3 subsequently translocates to the nucleus and binds to IFNstimulated response elements located in the promoter regions of IFN-responsive genes (15). These signaling events induce the expression of a variety of immunoregulatory genes and largely determine the pattern of immune cell activation following exposure to IFN-␣ (9, 16 –19). We have previously demonstrated a high degree of variability in the formation of phosphorylated STAT1 (P-STAT1)3 in patient immune effector cells following IFN-␣-2b immunotherapy and have shown that Jak-STAT signal transduction is down-regulated at higher dose levels of IFN-␣ (20). These data suggested that negative regulatory pathways might influence signal transduction and gene expression in human immune cells following exposure to IFN-␣. Investigators have identified a family of proteins termed suppressors of cytokine signaling (SOCS) that negatively regulate 3 Abbreviations used in this paper: P-STAT1, phosphorylated STAT1; SOCS, suppressor of cytokine signaling; SH2, Src homology 2; CIS, cytokine-inducible SH2containing protein; ISG, IFN-stimulated gene; siRNA, small inhibitory RNA; hu, human; EGFP, enhanced GFP; DC, dendritic cell; GH, growth hormone; MU, million units. Copyright © 2007 by The American Association of Immunologists, Inc. 0022-1767/07/$2.00 Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 Proteins belonging to the suppressors of cytokine signaling (SOCS) family have been shown to regulate cytokine signal transduction in various cell types but their role in modulating the response of immune cells to IFN-␣ has not been fully explored. We hypothesized that SOCS proteins would inhibit the antitumor activity of IFN-␣-stimulated immune cells. Transcripts for SOCS1, SOCS2, SOCS3, and cytokine-inducible Src homology 2-containing protein were identified in total human PBMC (PBMCs, NK cells, and T cells) within 1–2 h of stimulation with IFN-␣ (103–105 U/ml). Immunoblot analysis confirmed the expression of these factors at the protein level. Transcripts for SOCS proteins were rapidly but variably induced in PBMCs from patients with metastatic melanoma following the i.v. administration of IFN-␣-2b (20 million units/m2). Overexpression of SOCS1 and SOCS3, but not SOCS2, in the Jurkat T cell line inhibited IFN-␣-induced phosphorylated STAT1 and the transcription of IFN-stimulated genes. Conversely, small inhibitory RNA-mediated down-regulation of SOCS1 and SOCS3 in Jurkat cells and normal T cells enhanced the transcriptional response to IFN-␣. Loss of SOCS1 or SOCS3 in murine immune effectors was associated with enhanced IFN-induced phosphorylated STAT1, transcription of IFN-stimulated genes, and antitumor activity. Of note, IFN-␣ treatment eliminated melanoma tumors in 70% of SOCS1-deficient mice, whereas IFN-treated SOCS-competent mice all died. The antitumor effects of IFN-␣ in tumor-bearing SOCS1-deficient mice were markedly inhibited following depletion of CD8ⴙ T cells. These results indicate that the antitumor response of immune effector cells to exogenous IFN-␣ is regulated by SOCS proteins. The Journal of Immunology, 2007, 178: 4832– 4845. The Journal of Immunology 4833 Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 FIGURE 1. SOCS transcripts are rapidly induced in PBMCs following IFN-␣ stimulation. PBMCs from normal donors were treated with IFN-␣ (103–105 U/ml) or PBS and SOCS mRNA levels were measured by real-time PCR at four time points (0.5, 1, 2, 4 h) using primers specific for (A) SOCS1, (B) SOCS2, (C) SOCS3, or (D) CIS. Data were expressed as the mean fold increase relative to baseline levels (PBS treatment). All real-time PCR data were normalized to the level of -actin mRNA (housekeeping gene). E, Phosphorylation of STAT1 at Tyr701 was measured in parallel by flow cytometry. Mean-specific fluorescence (Fsp) is illustrated on the y-axis. Appropriate isotype control Abs were used to determine background staining. All flow cytometric data were derived from at least 10,000 events gated on the lymphocyte populations determined by light scatter properties (forward scatter vs side scatter). Error bars denote the 95% confidence interval of triplicate experiments (three donors). ⴱ, Statistically significant results vs PBS treatment. PBMCs were isolated from normal donors, stimulated with IFN-␣ (104 U/ml), and harvested at various times (1, 3, 5, 7, 24 h). Following immunoprecipitation, SOCS protein levels were measured by immunoprecipitation and subsequent immunoblot analysis using Abs directed against (F) SOCS1, SOCS2, SOCS3, or CIS. Lysates from a SOCS-overexpressing human melanoma cell line (HT144) were used as positive controls. Due to the immunoprecipitation protocol, levels of -actin were measured separately to control for loading. Densitometric data (fold induction) for each condition is shown at the bottom of each lane. Blots shown are representative of separate experiments using PBMCs from three normal donors. Jak-STAT signal transduction (21). The SOCS family of proteins consists of eight members, including SOCS1-SOCS7 and cytokine-inducible Src homology 2 (SH2)-containing protein (CIS). All SOCS proteins have a central SH2 domain that allows them to bind to phosphotyrosine residues in cytokine receptors or Jaks (22–27) and a C-terminal SOCS box domain that may function to target SOCS-bound proteins for proteasomal degradation (28, 29). SOCS1 and SOCS3 also contain a kinase inhibitory region that is IFN-␣ ANTITUMOR RESPONSE IS NEGATIVELY REGULATED BY SOCS 4834 We now demonstrate that SOCS1–3 and CIS are rapidly induced in whole PBMCs, T cells, and NK cells at the transcript and protein level following treatment with IFN-␣. The IFN-␣-induced activation of STAT1 and the subsequent regulation of IFN-stimulated genes (ISGs) was significantly reduced in SOCS1- and SOCS3-overexpressing lymphoid cell lines, whereas inhibition of SOCS1 and SOCS3 activity by small inhibitory (siRNA) knockdown led to an enhanced response. Furthermore, IFN-␣-induced signal transduction, gene regulation, and antitumor activity were enhanced in SOCS1- and SOCS3-deficient mice. These results demonstrate that SOCS proteins are critical negative regulators of the immune response to exogenous IFN-␣. Materials and Methods Reagents and cell lines 0 Ab for depletion of CD8⫹ T cells Rat anti-mouse CD8 Ab (clone 2.43) was purchased from the National Cell Culture Center (NCCC; Minneapolis, MN). For depletion of CD8⫹ T cells, 100 g of Ab was injected i.p. on days ⫺3, ⫺1, ⫹1, ⫹3, and every 4 days thereafter in relation to the tumor challenge. Rat IgG was used as a control. CD8 depletion was confirmed by flow cytometric analysis of PBMCs obtained from venous blood. Animals FIGURE 1. (continued) SOCS1-deficient mice die of overwhelming inflammation unless the endogenous release of IFN-␥ is eliminated (37). SOCS3⫺/⫺ is an embryonic lethal mutation (38). Therefore, SOCS1⫹/⫺ IFN-␥⫺/⫺ and SOCS3⫹/⫺ mouse breeding pairs (C57BL/6, Sv129 background) were obtained from Dr. J. Ihle (St. Jude Children’s Research Institute, Memphis, TN) and bred to produce their SOCS competent (SOCS1⫹/⫹IFN-␥⫺/⫺ and SOCS3⫹/⫹) and SOCS-deficient (SOCS1⫹/⫺IFN-␥⫺/⫺, SOCS1⫺/⫺IFN-␥⫺/⫺, and SOCS3⫹/⫺) counterparts. Genotyping of the SOCS1 and SOCS3 mice and confirmation of SOCS1 and SOCS3 protein deficiencies was performed as previously described (Refs. 37 and 38 and data not shown). Mice of 5– 6 wk of age were used in all experiments. Spleens from male and female mice of each genotype were removed aseptically and mechanically dispersed through 70 M cell strainers. Splenocytes were washed with PBS and 5% FBS, pelleted by centrifugation and resuspended in RPMI 1640 and 10% FBS. All experiments were performed in compliance with the guidelines of the Institutional Laboratory Animal Care and Use Committee of The Ohio State University (Protocol 2004A0151). Murine tumor models able to inhibit Jak activity (26, 27, 30). The expression of SOCS1 and SOCS3 has been shown to mediate potent inhibitory effects on IFN-␣-stimulated signal transduction and gene regulation in several experimental systems (31–34), however, the effect of exogenous IFN-␣ on SOCS expression in resting immune cell subsets has yet to be defined in the context of cancer immunotherapy. We hypothesized that SOCS proteins exert a negative effect on IFN␣-induced immune activity. An i.p. model of murine malignant melanoma was used to test the antitumor effects of IFN-A/D in SOCS-deficient mice (36). Mice were injected i.p. with 106 JB/MS melanoma tumor cells and randomly selected to receive either PBS or IFN-A/D (2 ⫻ 104 U/day, i.p.). Mice were examined daily, and those exhibiting signs of progressive disease were euthanized via CO2 inhalation. Survival experiments used at least six mice per group. Because IFN-A/D treatment was effective at protecting against lethal tumor challenge in SOCS1⫹/⫺ and SOCS1⫺/⫺ mice, this model was modified to permit the outgrowth of tumors for immunohistochemical analysis. For these studies, mice were injected i.p. on day 0 with 106 JB/MS melanoma cells. Beginning on day 7, mice were treated i.p. for 3 days with IFN-␣ Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 Recombinant human (hu) IFN-␣-2b (specific activity of 2 ⫻ 108 IU/mg) was purchased from Schering-Plough. Human growth hormone was purchased from Apollo Cytokine Research. IFN-A/D (sp. act. 1.1 ⫻ 108 U/mg; PBL Biomedical) was used in all murine tumor challenge experiments and was administered via the i.p. route at a dose of 2 ⫻ 104 U/day. IFN-A/D, or universal type I IFN, is a human hybrid recombinant type I IFN constructed from recombinant hu-IFN-␣ A and hu-IFN-␣ D. It is active on a wide variety of mammalian cells (PBL Biomedical). The human melanoma cell lines were gifts from Dr. S. Ferrone (Roswell Park Cancer Institute, Buffalo, NY) and were cultured in RPMI 1640 with 10% FBS and antibiotics (35). The Jurkat T cell lymphoma cell line (clone E6-1) was obtained from the American Type Culture Collection. The murine melanoma cell line JB/MS was obtained from V. Hearing (National Cancer Institute, Bethesda, MD) and grown as an adherent monolayer in DMEM supplemented with 10% FBS, sodium bicarbonate, 4 mM L-glutamine, 1% vitamins, 1% sodium pyruvate, 1% nonessential amino acids, and antibiotics (36). The Journal of Immunology 4835 Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 FIGURE 2. SOCS transcripts are differentially induced in NK cells and T cells following IFN-␣ stimulation. NK cells (CD56⫹) and T cells (CD3⫹) were isolated from normal donors (n ⫽ 3) and treated with 104 U/ml IFN-␣ or PBS. Cells were harvested at four time points (1, 2, 4, 6 h) for real-time PCR analyses of (A) SOCS1, (B) SOCS2, (C) SOCS3, and (D) CIS transcript levels. Data were expressed as the mean fold increase relative to baseline levels (PBS treatment). 4836 IFN-␣ ANTITUMOR RESPONSE IS NEGATIVELY REGULATED BY SOCS Quantitation kit (Molecular Probes), and reverse transcribed as previously described (39). The resulting cDNA was used as a template to measure gene expression by real-time PCR using predesigned primer/probe sets (Assays On Demand; Applied Biosystems) and 2⫻ TaqMan Universal PCR Master Mix according to the manufacturer’s recommendations as previously described (40). Predesigned primer/probe sets for human -actin were used as an internal control in each reaction well (Applied Biosystems). Real-time PCR data was analyzed using the Sequence Detector software version 1.6. Flow cytometric analysis of P-STAT1 Phosphorylation of STAT1 at Tyr701 was measured using an intracellular flow cytometric assay as previously described, with modifications (20, 41). A rabbit anti-P-STAT1 (Tyr701) primary Ab (Cell Signaling Technology) was used in combination with a goat anti-rabbit Alexa Fluor 488-conjugated secondary Ab (Molecular Probes). For assays involving enhanced GFP (EGFP)-positive cells, a goat anti-rabbit allophycocyanin-conjugated secondary Ab was used (Santa Cruz Biotechnology). Immunoprecipitation and immunoblot analysis Design of SOCS constructs FIGURE 3. Differential SOCS expression and STAT1 activation in melanoma patients undergoing IFN-␣ immunotherapy. PBMCs from (A) five melanoma patients were obtained immediately before and 1 h following administration of high-dose IFN-␣ (20 MU/m2 i.v.) and analyzed for SOCS1–3 and CIS mRNA levels by real-time PCR. In addition, freshly isolated PBMCs from (B) normal human donors (n ⫽ 5) were treated in vitro with IFN-␣-2b (104 U/ml) and tested for the induction of SOCS transcripts by real-time PCR. Data were expressed as the mean fold increase relative to baseline levels. All real-time PCR data were normalized to the level of -actin mRNA. (2 ⫻ 104 U) or PBS. Tumors were harvested on day 10, formalin fixed, embedded in paraffin, and sectioned. Isolation of immune subsets PBMC were isolated from source leukocytes of healthy adult donors (American Red Cross) or from the peripheral blood of patients receiving high-dose IFN-␣-2b (Ohio State University Institutional Review Board-approved protocol 99H0348) via density gradient centrifugation with Ficoll-Paque Plus (Amersham Biosciences). Lymphocyte subsets were enriched for individual cell populations (CD3⫹/CD56⫺ T cells and CD56⫹/CD3⫺ NK cells) by negative selection with the appropriate Rosette Sep reagents (Stem Cell Technologies) per the manufacturer’s recommendations. Enriched cell populations were cultured in RPMI 1640 medium supplemented with 10% human AB serum (Pel-Freez Clinical Systems). Cell purity was routinely ⬎95% as determined by flow cytometry. Real-time PCR Following TRIzol extraction (Invitrogen Life Technologies) and RNeasy purification (Qiagen), total RNA was quantitated via the RiboGreen RNA Overexpression of SOCS1, SOCS2, and SOCS3 proteins was achieved using the PINCO retroviral vector as previously described (43). Briefly, PBMCs from a normal healthy donor were stimulated with IFN-␣ and RNA was isolated and converted to cDNA for use as a template in a PCR to isolate the human SOCS1, SOCS2, and SOCS3 genes. Primers were designed to incorporate 1) AT overhangs; 2) 5⬘ BamHI and 3⬘ EcoRI restriction sites; 3) A C-terminal myc tag; and 4) a Kozak sequence before the initiation codon. SOCS transcripts were amplified using PCR according to the following schema: 94°C for 5 min; 30 cycles of 94°C for 30 s, 55°C for 30 s, 72°C for 1 min, followed by a final extension at 72°C for 7 min. PCR products were gel purified (Qiagen Gel Extraction kit) and ligated into the PCR2.1 vector by TA cloning according to the manufacturer’s recommendations (Invitrogen Life Technologies). Following sequence verification, plasmids were digested with BamHI and EcoRI to remove SOCS-encoding dsDNA and these inserts were then ligated into the BamHI EcoRI-digested PINCO expression plasmid. Ligation reactions were transformed into top 10 Escherichia coli and plasmid DNA was sequenced with the following primers (PINCO forward, 5⬘-ACCTTACACAGTCCTGCTGA-3⬘; PINCO reverse, 5⬘-TGAACTAATGACCCCGTAATT-3⬘) to verify each SOCSexpressing construct. Following sequence confirmation, each construct was prepared for virus production by endotoxin-free Maxiprep (Qiagen). Generation of SOCS-expressing retroviral constructs and transduction of Jurkat cells SOCS-overexpressing PINCO retroviral constructs were generated by transient transfection of the Phoenix-Ampho packaging cell line as previously described (43). The Jurkat cell line was transduced with SOCS-overexpressing retroviral constructs as previously described by Becknell et al. (43). Infection efficiency was determined by flow cytometry for EGFP expression. Cells were sorted based on EGFP positivity and used as described. SOCS down-regulation by RNA interference High-purity siRNA oligonucleotides that target SOCS1 (5⬘-CTGGTT GTTGTAGCAGCTTAA-3⬘) and SOCS3 (5⬘-TCGGGAGTTCCTGGAC CAGTA-3⬘) sequences were purchased from Qiagen. An oligonucleotide that does not match any human genome sequence was used as a control siRNA (5⬘-AACACAGTGGAGCGAATTCCT-3⬘; Qiagen). Jurkat cells and normal T cells were transfected with siRNA (2 g) via electroporation using the Nucelofector Amaxa device and cell-specific nucleofector reagent according to the manufacturer’s recommendations. All real-time PCR data were normalized to the level of -actin mRNA. E, Flow cytometric analysis of P-STAT1 levels in purified NK and T cell subsets was performed in parallel. Error bars denote the 95% confidence interval of triplicate experiments (three donors). ⴱ, Statistically significant results vs PBS treatment. ‡, Significant differences between T cells and NK cells. Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 Following treatment, cells were harvested and lysed in TN1 lysis buffer (125 mM NaCl, 50 mM Tris (pH 8), 10 mM EDTA, 10 mM Na4P2O7 䡠 10 H2O, 10 mM NaF, 1% Triton X-100, 3 mM Na3VO4, 5 g of aprotinin and leupeptin), and centrifuged at 10,000 rpm. For immunoprecipitation experiments, supernatants were collected and treated with 5 g of the appropriate Ab, processed per manufacturer’s recommendations (Abcam), and then subjected to immunoblot analysis as previously described (42). The Journal of Immunology 4837 Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 FIGURE 4. Overexpression of SOCS1 and SOCS3 protein in Jurkat cells inhibits the response to IFN-␣. The Jurkat T cell lymphoma cell line was transduced with PINCO retroviral constructs encoding SOCS1, SOCS2, or SOCS3 protein. Cells transduced with the empty PINCO vector served as a negative control. Cell populations were routinely ⬎95% pure post-FACS for GFP. A, Transcript levels of SOCS1, SOCS2, and SOCS3 in transduced cells as measured by real-time PCR. Data are expressed as the mean fold increase relative to baseline levels. All real-time PCR data were normalized to the level of -actin mRNA in duplicate experiments. B, Protein levels of SOCS1, SOCS2, and SOCS3 as measured by immunoblot analysis of whole cell lysates. These results are representative of duplicate experiments. C, Flow cytometric analysis of P-STAT1 formation in transduced cells following stimulation with 4838 IFN-␣ ANTITUMOR RESPONSE IS NEGATIVELY REGULATED BY SOCS Statistical analysis To estimate the changes in SOCS1–3, CIS, and P-STAT1 over time, linear mixed effects models were applied to the data (see Figs. 1 and 2). For each model, the presence of a significant quadratic trend was assessed, as the changes over time appeared to be nonlinear. Based on the models, point estimates of fold increases were calculated with 95% confidence intervals. Statistical analyses for Figs. 3–7 were assessed by ANOVA; pairwise comparisons were performed using a two-sided ␣ ⫽ 0.05 level of significance. Kaplan-Meier estimates of the survival function were calculated for the different mouse groups, and log-rank tests were used to assess group differences in survival. For all analyses, an ␣ ⫽ 0.05 level of significance was used. All analyses were performed using SAS version 9.1 (SAS Institute). Results SOCS1, 2, 3, and CIS are rapidly induced in human PBMCs following in vitro stimulation with IFN-␣ SOCS1, 2, 3, and CIS are differentially induced in human T cells and NK cells following in vitro stimulation with IFN-␣ To characterize the induction of negative regulators in the immune cell compartments thought to be responsible for mediating the an- Expression of SOCS transcripts in patient PBMCs post-IFN therapy To characterize the expression of SOCS transcripts in response to exogenous IFN-␣, peripheral venous blood was obtained from patients with metastatic melanoma (n ⫽ 5) immediately before and 1 h following the first dose of IFN-␣-2b (20 million units (MU)/m2 i.v.). PCR analysis revealed that SOCS1, SOCS2, SOCS3, and CIS transcripts were all expressed at the one hour time point following IFN-␣ therapy (Fig. 3A). Of note, there was considerable interpatient variation with respect to the induction of SOCS1 (range ⫽ 8.6- to 171.0-fold increase compared with baseline levels), SOCS2 (range ⫽ 3.0- to 9.6-fold increase), SOCS3 (range ⫽ 1.1- to 4.6fold increase), and CIS (range ⫽ 1.2- to 11.5-fold increase). In addition, freshly isolated PBMCs from normal human donors (n ⫽ 5) were treated in vitro with IFN-␣-2b (104 U/ml) and tested for the induction of SOCS transcripts by real-time PCR (Fig. 3B). The induction of SOCS1 in normal donors following in vitro IFN-␣ stimulation was also variable. Interestingly, there appeared to be greater induction of SOCS species in PBMCs following in vivo administration of IFN-␣. Overexpression of SOCS proteins in the Jurkat cell line inhibits the response to IFN-␣ The Jurkat T cell lymphoma cell line was transduced with retroviral constructs expressing SOCS1, 2, or 3 to further evaluate the role of SOCS in IFN-␣-mediated signal transduction and gene expression. As a control, Jurkat cells were also transduced in parallel with the unmanipulated vector (PINCO-EGFP). Cells were then harvested from culture, enriched for EGFP expression by FACS sorting (⬎95% pure) and tested for their responsiveness to IFN-␣. Increased expression of these SOCS species was confirmed by real-time PCR and immunoblot analysis (Fig. 4, A and B). Cells were treated with various concentrations of IFN-␣ (102–104 U/ml) or PBS for 30 min and then analyzed for the level of P-STAT1 by flow cytometry and downstream ISG transcripts by real-time PCR (18 h time point). Phosphorylation of STAT1 was not appreciably IFN-␣ (102–104 U/ml) or PBS for 30 min. D, Analysis of 2⬘-5⬘-oligoadenylate synthetase 1 (OAS1), IFN-stimulated gene 20 (ISG20), and IFN-induced protein with tetratricopeptide repeats 2 (IFIT2) transcript levels in transduced cells following stimulation with IFN-␣ (104 U/ml) or PBS for 18 h. Error bars denote the 95% confidence interval of duplicate experiments. ⴱ, Statistically significant results. E, The 1106 MEL melanoma cell line was transduced with a PINCO retroviral construct encoding the SOCS2 protein. Cells transduced with the empty PINCO vector served as a negative control. Cells were treated with PBS or human GH (huGH; 100 ng/ml) for 15 min. Levels of P-STAT5 were measured by immunoblot analysis. -actin was used as a loading control. SOCS2 overexpression was also confirmed by immunoprecipitation and subsequent immunoblot analysis. Nonspecific bands (NSB) represent the L chain of the rabbit anti-SOCS2 Ab used in the immunoprecipitation. Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 Freshly isolated PBMCs from normal human donors (n ⫽ 3) were treated in vitro with varying concentrations of IFN-␣-2b (101–105 U/ml) and tested for the induction of SOCS transcripts by real-time PCR (Fig. 1, A–D, represent the combined results of these normal donors). SOCS1–3 and CIS were rapidly induced (1 h or less) in normal PBMCs following in vitro stimulation with IFN-␣ (Fig. 1, A–D, and data not shown). Significant induction of these genes as compared with PBS-treated cells was observed following treatment with doses of IFN-␣ as low as 103 U/ml ( p ⬍ 0.0001), however, maximal expression occurred in response to 104 or 105 U/ml IFN-␣ ( p ⬍ 0.0001). For example, PBMCs treated for 2 h with 104 U/ml IFN-␣ expressed high levels of SOCS1 (10.32 ⫾ 2.19-fold induction), SOCS2 (13.10 ⫾ 3.46), SOCS3 (2.79 ⫾ 0.87), and CIS (5.98 ⫾ 2.97) as compared with PBS-treated cells. SOCS transcripts were also reproducibly induced at lower doses of IFN-␣ (101–102 U/ml; data not shown) but to a lesser extent. SOCS4 –7 and protein inhibitor of activated STAT1 (PIAS1) transcripts were not induced even when high doses of IFN-␣ were used (data not shown). IFN-␣-induced expression of SOCS transcripts by PBMCs was transient in nature as levels of SOCS1–3 and CIS reverted to baseline within 2– 4 h of stimulation. PBMCs from these same donors were simultaneously tested for activation of STAT1 using a flow cytometric assay that employs an Ab specific for P-STAT1. Robust phosphorylation of STAT1 was observed within 30 min of IFN-␣ treatment ( p ⬍ 0.001 vs PBS-treated PBMCs), however, levels of P-STAT1 had returned to baseline within 2 h of stimulation (Fig. 1E), a finding that was consistent with the expression of multiple SOCS species at this time point. The enhanced expression of SOCS species was confirmed at the protein level by immunoblot analysis. These studies revealed that SOCS1, SOCS2, SOCS3, and CIS were rapidly induced in PBMCs following exposure to IFN-␣ (Fig. 1F). In each case, there was increased expression of SOCS protein at the 1 h time point. Maximal induction of SOCS3 and CIS occurred 3 h posttreatment, whereas SOCS1 and SOCS2 expression peaked at 5 and 1 h, respectively. titumor effects of IFN-␣ (44 – 46), NK cells, and T cells were isolated from fresh PBMCs (n ⫽ 3 donors), treated in vitro with 104 U/ml IFN-␣ for varying periods of time (1, 2, 4, 6 h), and analyzed for SOCS transcripts by real-time PCR. SOCS1–3 and CIS transcripts were significantly up-regulated in T cells following incubation with IFN-␣ as compared with PBS-stimulated cells ( p ⬍ 0.001; Fig. 2, A–D). In contrast, only SOCS1 ( p ⫽ 0.0263), SOCS2 ( p ⫽ 0.0688), and SOCS3 ( p ⫽ 0.0031) were up-regulated over baseline in NK cells. Significantly greater induction of SOCS1 ( p ⫽ 0.0106), SOCS2 ( p ⬍ 0.0001), and CIS ( p ⬍ 0.0001) were observed in the T cell compartment as compared with the NK compartment at the 2-h time point. SOCS3 transcripts were up-regulated to a similar degree within T cells and NK cells in response to IFN-␣ ( p ⫽ 0.1521). T cells and NK cells were simultaneously evaluated for levels of P-STAT1 by flow cytometry (Fig. 2E). This analysis revealed a significantly greater induction of P-STAT1 in T cells as compared with NK cells at each time point and a more rapid return to baseline in T cells beginning at 2 h ( p ⬍ 0.0001). 4839 The Journal of Immunology Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 4840 IFN-␣ ANTITUMOR RESPONSE IS NEGATIVELY REGULATED BY SOCS Splenocytes from SOCS-deficient mice exhibit increased responsiveness to IFN-␣ The genotype of SOCS1- and SOCS3-deficient mice was confirmed by PCR and altered expression of SOCS protein was confirmed by immunoblot analysis (data not shown). Splenocytes from SOCS1⫹/⫹IFN-␥⫺/⫺, SOCS1⫹/⫺IFN-␥⫺/⫺, and SOCS1⫺/⫺ IFN-␥⫺/⫺ mice were examined for the ability to respond to IFN-␣ with activation of STAT1 and the transcription of IFN-␣-regulated genes. As seen in Fig. 5A, the generation of P-STAT1 in response to IFN-␣ was markedly increased in SOCS1⫺/⫺ splenocytes as compared with SOCS1⫹/⫺ splenocytes ( p ⫽ 0.002) and SOCS1⫹/⫹ splenocytes ( p ⫽ 0.004), while SOCS1⫹/⫺ splenocytes did not show enhanced activation of STAT1 ( p ⫽ 0.154 vs SOCS1⫹/⫹ splenocytes). The transcription of downstream IFNstimulated genes (Gzmb, Ifit2, Mx2) was also significantly enhanced in SOCS1⫺/⫺ splenocytes as compared with splenocytes from SOCS1⫹/⫺ and SOCS1⫹/⫹ mice ( p ⬍ 0.05 for all genes; Fig. 5C). Of note, splenocytes from SOCS1-deficient and SOCS1-com- petent mice expressed identical baseline levels of STAT1 and IFN-␣R (data not shown). Similar studies were conducted with SOCS3⫹/⫹ and SOCS3⫹/⫺ splenocytes and revealed increased activation of STAT1 ( p ⫽ 0.0002, Fig. 5B) and enhanced transcription of ISGs in response to IFN-␣ as compared with SOCS3⫹/⫹ splenocytes ( p ⬍ 0.0001 for all genes; Fig. 5D). siRNA-mediated down-regulation of SOCS1 and SOCS3 in Jurkat cells and normal T cells enhances the response to IFN-␣ The Jurkat cell line was transfected with siRNA oligonucleotides targeting SOCS1 or SOCS3 and placed in culture for 16 h before analysis. Control conditions included cells transfected with a control siRNA sequence as well as mock-transfected cells. The siRNA constructs inhibited the expression of SOCS1 and SOCS3 in Jurkat cells at the transcript and protein level (Fig. 6, A and B). Cells were then stimulated with IFN-␣ (104 U/ml) and analyzed for levels of the IFN-stimulated genes G1P2, OAS1, and IFIT2 at the 18 h time point. As seen in Fig. 6C, knockdown of SOCS1 and SOCS3 led to a significant increase in the transcription of the indicated genes ( p ⬍ 0.05 for all genes) as compared with the control conditions. Similar results were obtained following transfection of primary T cells from normal human donors with siRNA targeting SOCS1 or SOCS3 (data not shown). SOCS deficiency augments the antitumor effects of IFN-␣ in vivo The antitumor effects of IFN-␣ in the setting of SOCS1 deficiency were studied in a murine model of malignant melanoma in which JB/MS cells (1 ⫻ 106) were injected i.p. into SOCS1⫹/⫺IFN-␥⫺/⫺ or SOCS1⫺/⫺IFN-␥⫺/⫺ mice (n ⫽ 7 mice/group) (38). One day after tumor challenge, mice received daily i.p. injections of IFN-A/D (2 ⫻ 104 U) or PBS. SOCS1⫹/⫹ IFN-␥⫺/⫺ mice and wild-type mice (SOCS1⫹/⫹ IFN-␥⫹/⫹) served as controls. As expected, treatment of both tumor-bearing IFN-␥⫺/⫺ and wild-type mice with IFN-A/D led to a significant improvement in survival as compared with treatment with PBS alone (Fig. 7A; p ⫽ 0.0027). The antitumor effects of IFNA/D therapy were significantly enhanced in SOCS1-deficient mice as 57–71% of these mice were cured of their tumors, whereas PBStreated mice all died at 10 –14 days (Fig. 7B, p ⫽ 0.0002 for SOCS1⫹/⫺ mice; Fig. 7C, p ⫽ 0.0002 for SOCS1⫺/⫺ mice). Of note, there was no evidence that mice with SOCS deficiencies experienced increased systemic toxicity in response to IFN-␣ treatments: these mice behaved normally and histochemical analysis of their visceral organs revealed no increase in tissue damage or inflammatory cell infiltrate (data not shown). Immunohistochemistry of treated tumors revealed increased infiltration of CD45⫹ immune cells with IFN-␣ treatment but there was no difference between SOCS-competent and SOCS-deficient mice. SOCS1-deficient mice that survived following IFN-A/D treatment were observed for a total of 90 days during which no recurrent tumors were identified. These mice were then rechallenged with 1 ⫻ 106 JB/MS cells and remained tumor free for 100 days in the absence of additional IFN-␣ treatments (identically treated tumor-naive WT mice rapidly developed lethal disease), suggesting that an adaptive immune response to the tumor had been induced. Similarly, SOCS3-deficient mice exhibited enhanced survival (median survival ⫽ 29 days) in response to IFN-A/D therapy compared with wild-type littermates (median survival ⫽ 21 FIGURE 5. SOCS1- and SOCS3-deficient mice exhibit an augmented response to IFN-␣. A and B, The formation of P-STAT1 in SOCS-competent and SOCS-deficient murine splenocytes was measured by flow cytometry following stimulation of with IFN-A/D (104 U/ml) or PBS for 30 min. C and D, Transcription of granzyme B (Gzmb), Ifit2, and myxovirus resistance 2 (Mx2) genes were measured in splenocytes from SOCS1- and SOCS3-deficient mice following an 18 h stimulation with IFN-A/D (104 U/ml) or PBS via real-time PCR. Data were expressed as the mean fold increase relative to baseline levels (PBS treatment). All real-time PCR data were normalized to the level of -actin mRNA. Error bars denote the 95% confidence interval of duplicate experiments. ⴱ, Statistically significant results. Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 affected by transduction of Jurkat cells with the empty PINCOEGFP vector, however, cells that overexpressed SOCS1 or SOCS3 showed significantly reduced levels of P-STAT1 in response to IFN-␣ treatment ( p ⬍ 0.0001; Fig. 4C). The induction of ISGs was also significantly inhibited in cells that overexpressed SOCS1 or SOCS3 ( p ⬍ 0.045 for all genes; Fig. 4D). For example, the induction of 2⬘-5⬘-oligoadenylate synthetase 1 (OAS1) was 2-fold less in SOCS1 overexpressing Jurkat cells and 4-fold less in SOCS3 overexpressing Jurkat cells as compared with PINCOtransduced control cell lines ( p ⫽ 0.0002 and p ⬍ 0.0001, respectively). In contrast, overexpression of SOCS2 did not have a significant effect on the activation of STAT1 or transcription of downstream ISGs. To demonstrate that the PINCO-SOCS2 construct was producing a functional SOCS2 protein, we evaluated the known effects of SOCS2 on growth hormone (GH)-induced STAT5 phosphorylation (47). The 1106 MEL melanoma cell line was used instead of the Jurkat cell line due to the fact that Jurkat cells have very low levels of STAT5 protein (Ref. 48 and data not shown). As shown in Fig. 4E, overexpression of SOCS2 resulted in a significant decrease in GH-induced STAT5 phosphorylation. These data confirmed that the SOCS2 vector produces a functional protein that is capable of inhibiting relevant signaling pathways. Further in vitro studies were also conducted to analyze the relationship between IFN-␣-induced SOCS transcripts and the transcription of IFN-␣-responsive genes. Because SOCS transcripts are rapidly induced, human PBMCs were analyzed for the expression of SOCS transcripts by real-time PCR 2 h following IFN-␣ stimulation (104 U/ml). Expression of G1P2 mRNA was evaluated in these same normal donors at the 4-h time point, which is when this transcript is maximally induced by IFN-␣. As expected, there was a strong inverse correlation between the expression of transcript for SOCS1 and SOCS3 and the induction of G1P2 mRNA (parametric Pearson correlation; p ⫽ 0.0200 and p ⫽ 0.0218, respectively; data not shown). SOCS2 and CIS mRNA expression did not correlate with G1P2 expression. These results indicate that the transcriptional response of lymphoid cell lines to IFN-␣ is negatively regulated by specific SOCS proteins. The Journal of Immunology 4841 Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 FIGURE 6. siRNA-mediated inhibition of SOCS1 and SOCS3 augments IFN-␣ responsiveness in vitro. Jurkat cells were transfected via electroporation with siRNA specific to SOCS1 and SOCS3. As a negative control, Jurkat cells were transfected in parallel with a control siRNA or no siRNA (mock transfection). A, Specific down-regulation of SOCS by siRNA was confirmed at the transcript level by real-time PCR and (B) at the protein level by immunoprecipitation and immunoblot analysis of SOCS1 and SOCS3. These results are representative of duplicate experiments. C, IFN-␣ responsiveness at the level of gene transcription was measured in siRNA-transfected cell lines via real-time PCR. Fold increase in ISGs were determined following an 18-h stimulation with IFN-␣ (104 U/ml) or PBS (IFN-␣-inducible protein (clone IFI-15K) (G1P2), 2⬘-5⬘-oligoadenylate synthetase 1 (OAS1), and IFN response factor 7 (IRF7)). Data were expressed as the mean fold increase relative to baseline levels (PBS treatment). All real-time PCR data were normalized to the level of -actin mRNA. Error bars denote the 95% confidence interval of duplicate experiments. ⴱ, Statistically significant results. days; Fig. 7D; p ⫽ 0.0091). However, all SOCS3-deficient mice treated with IFN-A/D eventually succumbed to their tumors. In vivo depletion of CD8⫹ T cells significantly inhibits the antitumor action of IFN-␣ of SOCS1-deficient mice We next examined the role of CD8⫹ T cells in mediating the antitumor effects of IFN-␣ in this murine model. SOCS1-compe- tent and SOCS1-deficient mice were depleted of CD8⫹ T cells via i.p. injection of an anti-CD8 Ab. Control mice were treated with the appropriate isotype control Ab. Mice were then challenged i.p. with tumor and received daily i.p. injections of IFN-A/D (or PBS) beginning the next day. Depletion of CD8⫹ T cells markedly inhibited the antitumor effects of IFN-A/D in SOCS1-deficient mice (Fig. 7E; p ⫽ 0.0002). In contrast, mice receiving the control Ab 4842 IFN-␣ ANTITUMOR RESPONSE IS NEGATIVELY REGULATED BY SOCS Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 FIGURE 7. SOCS deficiency enhances the antitumor effect of IFN-A/D in a murine model of malignant melanoma. A, SOCS1⫹/⫹ IFN-␥⫺/⫺, (B) SOCS1⫹/⫺ IFN-␥⫺/⫺, (C) SOCS1⫺/⫺ IFN-␥⫺/⫺, and (D) SOCS3⫹/⫺ mice were injected i.p. with 1 ⫻ 106 JB/MS cells on day 0. Wild-type mice served as controls. Beginning on day 1, mice received daily i.p. injections of PBS or 2 ⫻ 104 U of IFN-A/D. As expected, treatment of tumor-bearing SOCS1⫹/⫹ mice with IFN-␣ led to a significant improvement in survival as compared with treatment with PBS alone (p ⫽ 0.0002; A). The antitumor effects of IFN-␣ therapy were significantly enhanced in SOCS1-deficient mice as 57–71% of these mice were cured of their tumors (B and C), whereas PBS-treated mice all died at 10 –14 days (p ⫽ 0.0002 for SOCS1⫹/⫺ mice; p ⫽ 0.0002 for SOCS1⫺/⫺ mice). Each group contained seven mice. The antitumor effects of IFN-␣ therapy were significantly enhanced in SOCS3-deficient mice vs SOCS3⫹/⫹ mice (p ⫽ 0.0091; D). Each group contained four mice. Before tumor inoculation, (E) SOCS1⫺/⫺IFN-␥⫺/⫺ and (F) SOCS1⫹/⫹IFN-␥⫺/⫺ mice were injected i.p. with 100 g of a rat anti-mouse CD8 Ab (clone 2.43) or rat IgG on days ⫺3, ⫺1, ⫹1, ⫹3, and every fourth day thereafter. CD8⫹ T cell depletion (defined as ⬍0.5% CD8⫹ cells in the peripheral blood) was confirmed by flow cytometry in all mice before tumor challenge. Mice were injected with 1 ⫻ 106 JB/MS cells on day 0. Beginning on day 1, mice received daily injections of PBS or 2 ⫻ 104 U of IFN-A/D. The antitumor effects of IFN-␣ therapy were significantly diminished in CD8-depleted mice as compared with CD8-competent mice, regardless of SOCS1 genotype (p ⬎ 0.0002). Each group contained seven mice. exhibited prolonged survival following therapy with IFN-A/D ( p ⫽ 0.0002) as observed previously. Depletion of CD8⫹ T cells also inhibited the effectiveness of IFN-A/D in IFN-␥⫺/⫺ mice (Fig. 7F; p ⫽ 0.0062). These data suggest that CD8⫹ T cells play a critical role in mediating the antitumor effects of IFN-␣ and that this effect is enhanced in SOCS1-deficient mice. The Journal of Immunology Discussion exert potent antitumor actions in response to IFN-␣ in the absence of SOCS1 activity. Importantly, dendritic cell (DC) function is also regulated by SOCS1. SOCS1⫺/⫺ mice have greater numbers of DCs. Also, these DCs respond more strongly to IL-4 and IFN-␥ and produce higher levels of B cell maturation/differentiation factors such as Baff/BLys (a member of the TNF ligand superfamily) as compared with normal mice (60). Shen et al. (61) subsequently demonstrated that down-regulation of SOCS1 in DCs using lentiviral-delivered siRNA led to enhanced production of TNF-␣, IL-6, and IL-2 in response to LPS and IFN-␥ treatments. In addition, coculture of SOCS1-deficient DCs with Ag-specific CD8⫹ T cells led to enhanced T cell proliferation and cytokine secretion as compared with wild-type DCs. Immunization with tyrosinase-related protein2-pulsed, SOCS1-silenced DCs abrogated the growth of a TRP2⫹ B16 melanoma in C57BL/6 mice (61). A similar study confirmed these results and identified several genes that were expressed to a greater degree in SOCS1-deficient DCs as compared with SOCS1⫹/⫹ DCs (62). Thus, SOCS1-deficiency appears to promote both the processing of tumor Ags by DCs and their recognition by effector T cells. Analysis of IFN-␣-induced DC activity in SOCSdeficient mice is therefore warranted. Reduced levels of SOCS1 in target cells appear to promote the therapeutic efficacy of IFN-␣ immunotherapy. Evidence in favor of this concept comes from a study by Roman-Gomez et al. (63) demonstrating that constitutive expression of SOCS1 in PBMCs obtained from chronic myeloid leukemia patients correlated with a significantly shorter progression-free survival and poor cytogenetic response to IFN-␣ therapy (63). Similarly, it has been shown by Imanaka et al. (57) that high-level expression of SOCS1 within hepatocytes from chronic hepatitis C patients correlated with a diminished antiviral response to IFN-␣. Also, Fenner et al. (64) recently demonstrated that, compared with wild-type mice, SOCS1-deficient mice are better able to use endogenous IFN-␣ to clear an otherwise lethal viral infection. These data are in agreement with our findings and point to a role for SOCS1 in regulating the antitumor effects of IFN-␣ therapy and the outcome of viral infections. Interestingly, selective down-regulation of SOCS1 within the T cell compartment does not lead to an overt inflammatory response, as occurs in SOCS1-deficient mice that possess a functioning IFN-␥ gene (65). Therefore, targeted down-regulation of SOCS proteins within specific cell types may help to avoid the toxicity associated with global down-regulation of SOCS1. The present study demonstrated that overexpression of SOCS1 and SOCS3 had negative effects on IFN-␣-induced Jak-STAT signal transduction and gene regulation, while experimental reductions in SOCS activity enhanced the response to IFN-␣. Reduced expression of SOCS1 or SOCS3 in tumor-bearing mice enhanced the antitumor activity of exogenous IFN-␣. These findings suggest that modulation of SOCS activity may have beneficial effects in the setting of cytokine-mediated immune phenomena. SOCS proteins may also play a role in mediating endogenous IFN activity which is known to be important in the immune surveillance for cancer cells (11). Acknowledgment We thank The Ohio State University Comprehensive Cancer Center RealTime Core Facility for assisting in the operation of the ABI PRISM 7900 Sequence Detection System. Disclosures The authors have no financial conflict of interest. Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 We have previously demonstrated that Jak-STAT signal transduction within host immune cells is critical to the antitumor effects of IFN-␣ in a murine model of malignant melanoma (9). This led us to examine the role of SOCS proteins in regulating the antitumor properties of IFN-␣-stimulated immune effector cells. The present study demonstrated that SOCS1, SOCS2, SOCS3, and CIS were rapidly induced in a dose-dependent manner by IFN-␣ in normal lymphocytes at the transcript and protein level. The inhibitory effects of SOCS proteins were highly specific, as overexpression of SOCS1 and SOCS3, but not SOCS2, in the Jurkat T cell lymphoma cell line inhibited IFN-␣-induced activation of STAT1 and the expression of IFN-stimulated genes. Conversely, siRNA-mediated down-regulation of SOCS1 and SOCS3 in Jurkat cells and T cells enhanced the transcriptional response to IFN-␣. The functional importance of SOCS proteins in regulating the actions of IFN-␣ was suggested by the improved ability of SOCS1- and SOCS3-deficient mice to eliminate melanoma tumor cells following treatment with IFN-␣. To date, there have been limited studies investigating the regulation of SOCS family protein expression in IFN-␣-stimulated immune effector cells. IFN-␣ has been shown to induce the expression of SOCS species in megakaryocytes, LPS-stimulated macrophages, in an IL-2-primed human T cell line, and a human chronic myelogenous leukemia cell line (32, 34, 49 –52). Overexpression of SOCS proteins has been shown to inhibit cytokine responses in hepatoma cells and activated T cells (33, 53–57). However, the effects of SOCS proteins on unmanipulated human lymphocytes have not been fully explored. We demonstrated that SOCS1, SOCS2, SOCS3, and CIS are differentially induced in both T cells and NK cells. The finding of variable SOCS induction in malignant melanoma patient PBMCs after the administration of high-dose IFN-␣-2b supports the clinical relevance of these findings and further suggests that the immune response to exogenous cytokines may be influenced by individual differences in the expression of SOCS proteins within lymphocyte populations. In the present report, inhibition of SOCS expression in T cells had marked effects on IFN-␣-induced gene expression. Furthermore, the antitumor effects of IFN-␣ were significantly enhanced in SOCS1-deficient mice: ⬃70% of mice achieved long-term resolution of their tumor-burden while no adverse side-effects were observed. SOCS1-deficient mice that were tumor free following IFN-␣ treatment survived a second challenge with JB/MS melanoma cells. SOCS3 deficiency also promoted the antitumor effects of IFN-␣. These enhanced antitumor effects of IFN-␣ were mediated, at least in part, by CD8⫹ T cells. Several lines of evidence point to SOCS1 as an important regulator of T cell development and function. Mice with a targeted deficiency of SOCS1 within the T cell compartment exhibit an increased ratio of CD8/CD4 mature thymic cells and a significant increase in the prevalence of CD44highCD8 memory T cells within the periphery (58). Memory T cells from these mice displayed a 5-fold increased proliferative response to IL-2 and IL-15 as compared with wild-type mice. Similarly, the proliferation of T cells from SOCS1⫺/⫺IFN-␥⫺/⫺ mice in response to anti-CD3 Ab was markedly enhanced in the presence of IL-12, whereas this cytokine had minimal effects on activated T cells from normal mice (58, 59). Recently, Davey et al. (58) discovered that SOCS1-deficient CD8⫹ T cells proliferate when transplanted to normal mice and that this response is driven by IL-15 and self ligands that normally drive homeostatic proliferation in T cell-deficient mice. The ability of CD8 depletion to abrogate the prosurvival effects of IFN-␣ in tumor-bearing, SOCS1-deficient mice suggests that this immune compartment can 4843 4844 IFN-␣ ANTITUMOR RESPONSE IS NEGATIVELY REGULATED BY SOCS References 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. gene CIS encodes an SH2-containing protein that binds to tyrosine-phosphorylated interleukin 3 and erythropoietin receptors. EMBO J. 14: 2816 –2826. Nicholson, S. E., T. A. Willson, A. Farley, R. Starr, J. G. Zhang, M. Baca, W. S. Alexander, D. Metcalf, D. J. Hilton, and N. A. Nicola. 1999. Mutational analyses of the SOCS proteins suggest a dual domain requirement but distinct mechanisms for inhibition of LIF and IL-6 signal transduction. EMBO J. 18: 375–385. Sasaki, A., H. Yasukawa, A. Suzuki, S. Kamizono, T. Syoda, I. Kinjyo, M. Sasaki, J. A. Johnston, and A. Yoshimura. 1999. Cytokine-inducible SH2 protein-3 (CIS3/SOCS3) inhibits Janus tyrosine kinase by binding through the N-terminal kinase inhibitory region as well as SH2 domain. Genes Cells 4: 339 –351. Larsen, L., and C. Ropke. 2002. Suppressors of cytokine signalling: SOCS. APMIS 110: 833– 844. Wormald, S., and D. J. Hilton. 2004. Inhibitors of cytokine signal transduction. J. Biol. Chem. 279: 821– 824. Yasukawa, H., H. Misawa, H. Sakamoto, M. Masuhara, A. Sasaki, T. Wakioka, S. Ohtsuka, T. Imaizumi, T. Matsuda, J. N. Ihle, and A. Yoshimura. 1999. The JAK-binding protein JAB inhibits Janus tyrosine kinase activity through binding in the activation loop. EMBO J. 18: 1309 –1320. Brender, C., M. Nielsen, K. Kaltoft, G. Mikkelsen, Q. Zhang, M. Wasik, N. Billestrup, and N. Odum. 2001. STAT3-mediated constitutive expression of SOCS-3 in cutaneous T-cell lymphoma. Blood 97: 1056 –1062. Sakai, I., K. Takeuchi, H. Yamauchi, H. Narumi, and S. Fujita. 2002. Constitutive expression of SOCS3 confers resistance to IFN-␣ in chronic myelogenous leukemia cells. Blood 100: 2926 –2931. Song, M. M., and K. Shuai. 1998. The suppressor of cytokine signaling (SOCS) 1 and SOCS3 but not SOCS2 proteins inhibit interferon-mediated antiviral and antiproliferative activities. J. Biol. Chem. 273: 35056 –35062. Brender, C., M. Nielsen, C. Ropke, M. H. Nissen, A. Svejgaard, N. Billestrup, C. Geisler, and N. Odum. 2001. Interferon-␣ induces transient suppressors of cytokine signalling expression in human T cells. Exp. Clin. Immunogenet. 18: 80 – 85. Lesinski, G. B., B. Badgwell, J. Zimmerer, T. Crespin, Y. Hu, G. Abood, and W. E. Carson III. 2004. IL-12 pretreatments enhance IFN-␣-induced Janus kinase-STAT signaling and potentiate the antitumor effects of IFN-␣ in a murine model of malignant melanoma. J. Immunol. 172: 7368 –7376. Berkelhammer, J., R. W. Oxenhandler, R. R. Hook, Jr., and J. M. Hennessy. 1982. Development of a new melanoma model in C57BL/6 mice. Cancer Res. 42: 3157–3163. Marine, J. C., D. J. Topham, C. McKay, D. Wang, E. Parganas, D. Stravopodis, A. Yoshimura, and J. N. Ihle. 1999. SOCS1 deficiency causes a lymphocytedependent perinatal lethality. Cell 98: 609 – 616. Marine, J. C., C. McKay, D. Wang, D. J. Topham, E. Parganas, H. Nakajima, H. Pendeville, H. Yasukawa, A. Sasaki, A. Yoshimura, and J. N. Ihle. 1999. SOCS3 is essential in the regulation of fetal liver erythropoiesis. Cell 98: 617– 627. Lengyel, P. 1993. Tumor-suppressor genes: news about the interferon connection. Proc. Natl. Acad. Sci. USA 90: 5893–5895. Carr, D. J., J. Chodosh, J. Ash, and T. E. Lane. 2003. Effect of anti-CXCL10 monoclonal antibody on herpes simplex virus type 1 keratitis and retinal infection. J. Virol. 77: 10037–10046. Fleisher, T. A., S. E. Dorman, J. A. Anderson, M. Vail, M. R. Brown, and S. M. Holland. 1999. Detection of intracellular phosphorylated STAT-1 by flow cytometry. Clin. Immunol. 90: 425– 430. Gregorieff, A., S. Pyronnet, N. Sonenberg, and A. Veillette. 2000. Regulation of SOCS-1 expression by translational repression. J. Biol. Chem. 275: 21596 –21604. Becknell, B., R. Trotta, J. Yu, W. Ding, H. C. Mao, T. Hughes, T. Marburger, and M. A. Caligiuri. 2005. Efficient infection of human natural killer cells with an EBV/retroviral hybrid vector. J. Immunol. Methods 296: 115–123. Azogui, O., M. F. Avril, A. Margulis, M. Guillard, B. Caillou, and M. Prade. 1991. Tumor-infiltrating CD3⫺ NK cells are more effective than CD3⫹ T cells in killing autologous melanoma cells. J. Invest. Dermatol. 97: 425– 429. Xu, D., P. Gu, P. Y. Pan, Q. Li, A. I. Sato, and S. H. Chen. 2004. NK and CD8⫹ T cell-mediated eradication of poorly immunogenic B16-F10 melanoma by the combined action of IL-12 gene therapy and 4-1BB costimulation. Int. J. Cancer 109: 499 –506. Wargo, J. A., L. Y. Schumacher, B. Comin-Anduix, V. B. Dissette, J. A. Glaspy, W. H. McBride, L. H. Butterfield, J. S. Economou, and A. Ribas. 2005. Natural killer cells play a critical role in the immune response following immunization with melanoma-antigen-engineered dendritic cells. Cancer Gene Ther. 12: 516 –527. Horvat, S., and J. F. Medrano. 2001. Lack of Socs2 expression causes the highgrowth phenotype in mice. Genomics 72: 209 –212. Srahna, M., L. A. Van Grunsven, J. E. Remacle, and P. Vandenberghe. 2006. CTLA-4 interacts with STAT5 and inhibits STAT5-mediated transcription. Immunology 117: 396 – 401. Wang, Q., Y. Miyakawa, N. Fox, and K. Kaushansky. 2000. Interferon-␣ directly represses megakaryopoiesis by inhibiting thrombopoietin-induced signaling through induction of SOCS-1. Blood 96: 2093–2099. Ishida, N., K. Oritani, M. Shiraga, H. Yoshida, S. Kawamoto, H. Ujiie, H. Masaie, M. Ichii, Y. Tomiyama, and Y. Kanakura. 2005. Differential effects of a novel IFN-/limitin and IFN-␣ on signals for Daxx induction and Crk phosphorylation that couple with growth control of megakaryocytes. Exp. Hematol. 33: 495–503. Li, Z., D. Metze, D. Nashan, C. Muller-Tidow, H. L. Serve, C. Poremba, T. A. Luger, and M. Bohm. 2004. Expression of SOCS-1, suppressor of cytokine signalling-1, in human melanoma. J. Invest. Dermatol. 123: 737–745. Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 1. Lens, M. B., and M. Dawes. 2002. Interferon ␣ therapy for malignant melanoma: a systematic review of randomized controlled trials. J. Clin. Oncol. 20: 1818 – 1825. 2. Tsao, H., M. B. Atkins, and A. J. Sober. 2004. Management of cutaneous melanoma. N. Engl. J. Med. 351: 998 –1012. 3. Kirkwood, J. M., M. H. Strawderman, M. S. Ernstoff, T. J. Smith, E. C. Borden, and R. H. Blum. 1996. Interferon ␣-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J. Clin. Oncol. 14: 7–17. 4. Kirkwood, J. M., J. G. Ibrahim, V. K. Sondak, J. Richards, L. E. Flaherty, M. S. Ernstoff, T. J. Smith, U. Rao, M. Steele, and R. H. Blum. 2000. High- and low-dose interferon ␣-2b in high-risk melanoma: first analysis of intergroup trial E1690/S9111/C9190. J. Clin. Oncol. 18: 2444 –2458. 5. Creagan, E. T., R. J. Dalton, D. L. Ahmann, S. H. Jung, R. F. Morton, R. M. Langdon, Jr., J. Kugler, and L. J. Rodrigue. 1995. Randomized, surgical adjuvant clinical trial of recombinant interferon ␣-2a in selected patients with malignant melanoma. J. Clin. Oncol. 13: 2776 –2783. 6. Kirkwood, J. M., J. G. Ibrahim, J. A. Sosman, V. K. Sondak, S. S. Agarwala, M. S. Ernstoff, and U. Rao. 2001. High-dose interferon ␣-2b significantly prolongs relapse-free and overall survival compared with the GM2-KLH/QS-21 vaccine in patients with resected stage IIB-III melanoma: results of intergroup trial E1694/S9512/C509801. J. Clin. Oncol. 19: 2370 –2380. 7. Nathan, P. D., and T. G. Eisen. 2002. The biological treatment of renal-cell carcinoma and melanoma. Lancet Oncol. 3: 89 –96. 8. von Stamm, U., E. B. Brocker, M. von Depka Prondzinski, D. J. Ruiter, P. Rumke, C. Broding, S. Carrel, and F. J. Lejeune. 1993. Effects of systemic interferon-␣ (IFN-␣) on the antigenic phenotype of melanoma metastases. EORTC Melanoma Group Cooperative Study No. 18852. Melonoma Res. 3: 173–180. 9. Lesinski, G. B., M. Anghelina, J. Zimmerer, T. Bakalakos, B. Badgwell, R. Parihar, Y. Hu, B. Becknell, G. Abood, A. R. Chaudhury, et al. 2003. The antitumor effects of IFN-␣ are abrogated in a STAT1-deficient mouse. J. Clin. Invest. 112: 170 –180. 10. Parangi, S., M. O’Reilly, G. Christofori, L. Holmgren, J. Grosfeld, J. Folkman, and D. Hanahan. 1996. Antiangiogenic therapy of transgenic mice impairs de novo tumor growth. Proc. Natl. Acad. Sci. USA 93: 2002–2007. 11. Dunn, G. P., A. T. Bruce, K. C. Sheehan, V. Shankaran, R. Uppaluri, J. D. Bui, M. S. Diamond, C. M. Koebel, C. Arthur, J. M. White, and R. D. Schreiber. 2005. A critical function for type I interferons in cancer immunoediting. Nat. Immunol. 6: 722–729. 12. Navarro, S., O. R. Colamonici, and A. Llombart-Bosch. 1996. Immunohistochemical detection of the type I interferon receptor in human fetal, adult, and neoplastic tissues. Mod. Pathol. 9: 150 –156. 13. Haque, S. J., and B. R. Williams. 1998. Signal transduction in the interferon system. Semin. Oncol. 25: 14 –22. 14. Darnell, J. E., Jr., I. M. Kerr, and G. R. Stark. 1994. Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science 264: 1415–1421. 15. Levy, D., N. Reich, D. Kessler, R. Pine, and J. E. Darnell, Jr. 1988. Transcriptional regulation of interferon-stimulated genes: a DNA response element and induced proteins that recognize it. Cold Spring Harb. Symp. Quant. Biol. 53(Pt. 2): 799 – 802. 16. Meraro, D., M. Gleit-Kielmanowicz, H. Hauser, and B. Z. Levi. 2002. IFNstimulated gene 15 is synergistically activated through interactions between the myelocyte/lymphocyte-specific transcription factors, PU.1, IFN regulatory factor-8/IFN consensus sequence binding protein, and IFN regulatory factor-4: characterization of a new subtype of IFN-stimulated response element. J. Immunol. 168: 6224 – 6231. 17. Hatina, V. J., J. Kralova, and P. Jansa. 1996. Identification of an intragenic interferon-stimulated response element sequence of the mouse class I major histocompatibility complex H-2Kb gene. Exp. Clin. Immunogenet. 13: 55– 60. 18. Ohmori, Y., and T. A. Hamilton. 1995. The interferon-stimulated response element and a B site mediate synergistic induction of murine IP-10 gene transcription by IFN-␥ and TNF-␣. J. Immunol. 154: 5235–5244. 19. Herberman, R. B. 1997. Effect of ␣-interferons on immune function. Semin. Oncol. 24: S9-78 –S79-80. 20. Lesinski, G. B., S. V. Kondadasula, T. Crespin, L. Shen, K. Kendra, M. Walker, and W. E. Carson III. 2004. Multiparametric flow cytometric analysis of interpatient variation in STAT1 phosphorylation following interferon ␣ immunotherapy. J. Natl. Cancer Inst. 96: 1331–1342. 21. Alexander, W. S. 2002. Suppressors of cytokine signalling (SOCS) in the immune system. Nat. Rev. Immunol. 2: 410 – 416. 22. Endo, T. A., M. Masuhara, M. Yokouchi, R. Suzuki, H. Sakamoto, K. Mitsui, A. Matsumoto, S. Tanimura, M. Ohtsubo, H. Misawa, et al. 1997. A new protein containing an SH2 domain that inhibits JAK kinases. Nature 387: 921-924. 23. Masuhara, M., H. Sakamoto, A. Matsumoto, R. Suzuki, H. Yasukawa, K. Mitsui, T. Wakioka, S. Tanimura, A. Sasaki, H. Misawa, et al. 1997. Cloning and characterization of novel CIS family genes. Biochem. Biophys. Res. Commun. 239: 439 – 446. 24. Narazaki, M., M. Fujimoto, T. Matsumoto, Y. Morita, H. Saito, T. Kajita, K. Yoshizaki, T. Naka, and T. Kishimoto. 1998. Three distinct domains of SSI1/SOCS-1/JAB protein are required for its suppression of interleukin 6 signaling. Proc. Natl. Acad. Sci. USA 95: 13130 –13134. 25. Yoshimura, A., T. Ohkubo, T. Kiguchi, N. A. Jenkins, D. J. Gilbert, N. G. Copeland, T. Hara, and A. Miyajima. 1995. A novel cytokine-inducible The Journal of Immunology 59. Eyles, J. L., D. Metcalf, M. J. Grusby, D. J. Hilton, and R. Starr. 2002. Negative regulation of interleukin-12 signaling by suppressor of cytokine signaling-1. J. Biol. Chem. 277: 43735– 43740. 60. Hanada, T., H. Yoshida, S. Kato, K. Tanaka, K. Masutani, J. Tsukada, Y. Nomura, H. Mimata, M. Kubo, and A. Yoshimura. 2003. Suppressor of cytokine signaling-1 is essential for suppressing dendritic cell activation and systemic autoimmunity. Immunity 19: 437– 450. 61. Shen, L., K. Evel-Kabler, R. Strube, and S. Y. Chen. 2004. Silencing of SOCS1 enhances antigen presentation by dendritic cells and antigen-specific anti-tumor immunity. Nat. Biotechnol. 22: 1546 –1553. 62. Hanada, T., K. Tanaka, Y. Matsumura, M. Yamauchi, H. Nishinakamura, H. Aburatani, R. Mashima, M. Kubo, T. Kobayashi, and A. Yoshimura. 2005. Induction of hyper Th1 cell-type immune responses by dendritic cells lacking the suppressor of cytokine signaling-1 gene. J. Immunol. 174: 4325– 4332. 63. Roman-Gomez, J., A. Jimenez-Velasco, J. A. Castillejo, F. Cervantes, M. Barrios, D. Colomer, A. Heiniger, and A. Torres. 2004. The suppressor of cytokine signaling-1 is constitutively expressed in chronic myeloid leukemia and correlates with poor cytogenetic response to interferon-␣. Haematologica 89: 42– 48. 64. Fenner, J. E., R. Starr, A. L. Cornish, J. G. Zhang, D. Metcalf, R. D. Schreiber, K. Sheehan, D. J. Hilton, W. S. Alexander, and P. J. Hertzog. 2006. Suppressor of cytokine signaling 1 regulates the immune response to infection by a unique inhibition of type I interferon activity. Nat. Immunol. 7: 33–39. 65. Chong, M. M., A. L. Cornish, R. Darwiche, E. G. Stanley, J. F. Purton, D. I. Godfrey, D. J. Hilton, R. Starr, W. S. Alexander, and T. W. Kay. 2003. Suppressor of cytokine signaling-1 is a critical regulator of interleukin-7-dependent CD8⫹ T cell differentiation. Immunity 18: 475– 487. Downloaded from http://www.jimmunol.org/ by guest on June 12, 2017 52. Crespo, A., M. B. Filla, S. W. Russell, and W. J. Murphy. 2000. Indirect induction of suppressor of cytokine signalling-1 in macrophages stimulated with bacterial lipopolysaccharide: partial role of autocrine/paracrine interferon-␣/. Biochem. J. 349: 99 –104. 53. Egwuagu, C. E., C. R. Yu, M. Zhang, R. M. Mahdi, S. J. Kim, and I. Gery. 2002. Suppressors of cytokine signaling proteins are differentially expressed in Th1 and Th2 cells: implications for Th cell lineage commitment and maintenance. J. Immunol. 168: 3181–3187. 54. Yu, C. R., R. M. Mahdi, S. Ebong, B. P. Vistica, I. Gery, and C. E. Egwuagu. 2003. Suppressor of cytokine signaling 3 regulates proliferation and activation of T-helper cells. J. Biol. Chem. 278: 29752–29759. 55. Vlotides, G., A. S. Sorensen, F. Kopp, K. Zitzmann, N. Cengic, S. Brand, R. Zachoval, and C. J. Auernhammer. 2004. SOCS-1 and SOCS-3 inhibit IFN␣-induced expression of the antiviral proteins 2,5-OAS and MxA. Biochem. Biophys. Res. Commun. 320: 1007–1014. 56. Brand, S., K. Zitzmann, J. Dambacher, F. Beigel, T. Olszak, G. Vlotides, S. T. Eichhorst, B. Goke, H. Diepolder, and C. J. Auernhammer. 2005. SOCS-1 inhibits expression of the antiviral proteins 2⬘,5⬘-OAS and MxA induced by the novel interferon- IL-28A and IL-29. Biochem. Biophys. Res. Commun. 331: 543–548. 57. Imanaka, K., S. Tamura, K. Fukui, N. Ito, S. Kiso, Y. Imai, T. Naka, T. Kishimoto, S. Kawata, and Y. Shinomura. 2005. Enhanced expression of suppressor of cytokine signalling-1 in the liver of chronic hepatitis C: possible involvement in resistance to interferon therapy. J. Viral Hepat. 12: 130 –138. 58. Davey, G. M., R. Starr, A. L. Cornish, J. T. Burghardt, W. S. Alexander, F. R. Carbone, C. D. Surh, and W. R. Heath. 2005. SOCS-1 regulates IL-15driven homeostatic proliferation of antigen-naive CD8 T cells, limiting their autoimmune potential. J. Exp. Med. 202: 1099 –1108. 4845