* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CALCIUM AND PHOSPHATE METABOLISM
Resting potential wikipedia , lookup
Membrane potential wikipedia , lookup
Pre-Bötzinger complex wikipedia , lookup
Countercurrent exchange wikipedia , lookup
G protein-gated ion channel wikipedia , lookup
End-plate potential wikipedia , lookup
Neuromuscular junction wikipedia , lookup
Cardiac action potential wikipedia , lookup
Mineralized tissues wikipedia , lookup
Long-term depression wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
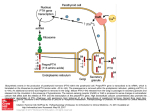
KSU CALCIUM AND PHOSPHATE METABOLISM Dr.Aida Abdelhamid Korish Assistant Prof.Physiology Dept. [PHYSIOLOGY DEPT.KSU] CALCIUM AND PHOSPHATE METABOLISM Three hormones are primary concerned with the regulation of calcium metabolism: -1,25-dihydroxycholecalciferol (a steroid hormone formed from vitamin D) -parathyroid hormone (secreted from the parathyroid gland) -cacitonin (secreted from perifollicular cells of the thyoid glands). All the three hormones probably operate to maintain the constancy of the calcium level in the body fluids. Glucocorticoid,growth hormone,oestrogen and various other hormones also affect calcium metabolism. Absorption of calcium and phosphate: Calcium is actively absorbed in the upper small intestine,facilitated by 1,25-dihydroxycholecalciferol. Calcium absorption is adjusted to body needs, absorption is increased in the presence of calcium deficiency and decreased in the presence of calcium excess. calcium absorption is : facilitated by lactose and protein, inhibited by phosphate and oxalate because these form insoluble salts with calcium in the intestine. Phosphate is absorbed in the duodenum and small intestine by both active transport and passive diffusion. when excess calcium is in the deit , the calcium tends to form insoluble calcium phosphate compounds that fail to be absorbed. Function of the calcium in the body: 1.it enter in the structure of bones,teeth,connective tissue elements and cellular cement substance. 2.ionized calcium is necessary for blood coagulation,muscle contraction,and nerve conduction. Function of phosphate: It enter in the formation of many compounds as ATPand C-AMP. Vitamin D and its role in calcium and phosphate absorption: Vitamin D has a potent effect on increasing calcium absorption from the intestinal tract,it also has important effect on bone deposition. vitamin D is not the active substance,it must first be converted in the liver and kidneys to the final active product 1,25 dihydroxycholecalciferol in multiple steps as the following: 1.vitamin D3(cholecalciferol) is formed in the skin as a result of irradiation of steroid(7dehydrocholesterol) by ultraviolet rays. exposure to the sun prevents vitamin D deficiency. 2. cholecalciferol is converted to 25hydroxychlecalciferol in the liver which has a feedback inhibitory effect on the conversion reactions. Feedback mechanism regulates the concentration of 25-hydroxychlecalciferol in the plasma and conserves the vitamin D for future use because once converted,it persists in the body for short time but vitamin D can be stored in the liver for several months. 3.in the kidneys, 25-hydroxychloecalciferol is converted to 1,25 dihydroxycolecalciferol which is the active form of vitamin D,this conversionrequires parathyroid hormone.parathyroid hormone exerts a potent effect in determining the functional effect of vitamin D in the body. 4. 1,25-dihydroxycholecalciferol causes formation of calcium binding protein in the intestinal epithelial cells.the rate of calcium absorption is proportional to the quantity of calcium binding protein.it remain in the intestine for several weeks after disappearance of 1,25dihydroxycholecalciferol. 5.when the plasma calcium concentration is increased,it inhibits parathyroid hormone secretion which lead to decrease formation of 1,25- dihydroxycholecalciferol. .lack of this in turn decreases the absorption of calcium from the intestines,from the renal tubules,thus causing the calcium ion concentration to fall back tward its normal level. 1,25- dihydroxycholecalciferol itself functions as a hormone to promote intestinal absorption of calcium. Figure:activation of vitaminD3 to form 1,25dihydroxycholecalciferol, and the role of vitamin D in cotrolling the plasma calcium concentration The concentration of calcium in the plasma is 9.4 mg/dL,varying between 9.0 and 10.0 mg/dL. The calcium in the plasma is present in three different forms: 1.40% of the calcium is combined with the plasma proteins(is non-diffusible through the capillary membrane). 2.10% of the calcium is diffusible through the capillary membrane but is combined with other substances of the plasma and interstitial fluids in such a manner that it is not ionized. 3.The remaining 50% of the calcium in the plasma is both diffusible through the capillary membrane and ionized.this ionic calcium is important for most functions of calcium in the body,including the effect of calcium on the heart,on the nervous system, and on bone formation. Bone calcium and its relationships to extracellular calcium and phosphate Bone is composed of tough organic matrix that is greatly strengthened by deposits of calcium salts. the crystalline salts deposited in the organic matrix are composed principally of calcium and phosphate in the form of hydroxyappitite crystals. about 0.5-1% of the total bone calcium is in the form of readily metabolizable amorphous calcium phosphate known as exchangeable calium that is always in equilibrium with calcium ions in the extracellular fluids.it provides a rapid buffering mechanism to keep the calcium ion concentration of extracellular fluids from rising to excessive levels or falling to very low levels. In addition to the buffer function of bones,the mitochondria of many of the tissues of the body,especially of the liver and intestine,also contain a reasonable amount of exchangeable calcium that provide an additional,buffer system for helping to maintain constancy of extracellular fluid calcium ion concentration. Parathyroid gland There are four parathyroid glands in human being;located immediately behind the thyroid gland. the parathyroid gland of the adult human contains chief cells and oxyphil cells. the chief cells secrete most of the parathyroid hormone(parathormone). Action of parathyroid hormone: The effect of parathormone is elevation of calcium ion concentration in the extracellular fluid and depression of phosphate concentration.bone,kidney and GIT are the three organs affected by parathormone. A) effect on bone: parathyroid hormone has two separate effect on bone in causing absorption of calcium and phosphate. 1.a very rapid phase that takes place in minutes and results from activation of the already existing bone cells(osteoclast) to promote calcium and phosphate absorption. 2. a slower phase requiring days or even weeks to become fully developed results from proliferation of the osteoclast,followed by by greatly enhanced osteoclastic reabsorption of the bone itself. B)Effect on the kidneys: 1. Adminstration of parathyroid hormone causes immediate and rapid loss of phosphate in urine by diminished proximal tubular reabsorption of phosphate ions. 2. parathyroid hormone increases the absorption of calcium in the proximal tubules and collecting ducts. C)Effect on the intestine: It enhances both calcium and phosphate absorption from the intestine by increasing the formation of 1,25 dihydroxycholecalciferol from Vit.D. Control of parathyroid hormone secretion: 1.the slightest decrease in calcium ion concentration in the extracellular fluid causes the glands to increase the rate of secretion within minutes, and if the decreased calcium concentration persists ,the gland will hypertrophy. 2.Any condition that increases the calcium ion concentration causes decreased activity and reduced size of the parathyroid gland such as : a)Excessive amount of calcium in diet. b)Increased Vit.D in the diet. c)Bone absorption caused by factors other than parathyroid. Hyperparathyroidism When the parathyroid glands do not secrete sufficient hormone,the osteoclast of the bone become inactive.as a result,bone reabsorption decrease so the level of calcium in the body fluid decreases. When the parathyroid glands are suddenly removed, the calcium level in the blood falls from the normal of 9.4 to 6 mg/dL within two to three days (hypocalcemia which leads to tetany) Causes of tetany: When the extracellular fluid concentration of calcium ion falls below normal,the nervous system becomes more excitable because of increased neuronal membrane permeability to sodium ions. this increase in excitability occurs both in CNS and in the peripheral nerves. The nerve fibres becomes so excitable that they begin to discharge spontaneously,initiating nerve impulses that pass to the peripheral skeletal muscles causing extensivespasm involving especially the muscles of the extremities and the larynx.laryngospasm becomes so severe that the airway is obstructed and fatal asphyxia is produced. Tetany in the hand occur before generalized tetany develop , this is called carpal spasm. Acute hypocalcemia in human being causes no other significant effects beside tetany,because tetany kills the patients before other effects can develop. Types of tetany: 1.manifest tetany: which shows itself without any stimulus to evoke it.the serum calcium is less than 7mg/dL. 2.latent tetany: the serum calcium ions is about 7mg/dL.this type of tetany needs certain tests to prove it. a)Chovostek,sign:quick contraction of theipsilateral facial muscles elicited by tapping over the fafacial nerve at the angle of the jew. b)Trousseau,sign: occlusion of the circulation with a blood pressure cuff causes a spasm of the muscles of the upper extremity which causes flexion of the wrist and thumb with extension of the fingers(carpal spasm). Because placing a tourniquet on the upper arm causes ischemia of the peripheral nerves and also increases the excitability of the nerves thus causing spasm of the muscles of the lower arm and hand. Hyperparathyroidism The cause of Hyperparathyroidism : IT IS THE TUMOUR OF ONE OF THE PARATHYROID GLANDS. In Hyperparathyroidism,extreme osteoclastic activity occurs in the bone and this elevated the calcium ion concentration in the extracellular fluid,which usually depressing the concentration of phosphate ions because of increased rate of excretion of phosphate. Bone disease in Hyperparathyroidism In severe hyperthyroidism, the osteoclastic absorption is severe,bone may be eaten away with development of large cavities filled with very large multinucleated osteoclast. radiographs of the bone show extensive decalcification. multiple fractures can result from slight trauma. Effect of hypercalcemia: in Hyperparathyroidism calium level increases which leads to: depression of the central and peripheral nervous system. muscular weakness. constipation,abdominal pain,peptic ulcer and loss of appetite because of depressed contractility of the muscle wall of the gastrointestinal tract. depressed relaxation of the heart during diastole. If the level of calcium in the body fluid rises to very high level, calcium,phosphate crystal may be deposited in: the alveoli of the lung. in the tubules of the kidneys. in the wall of the arteries. this effect can be fatal. Calcitonin This hormone reduces the blood calcium ion concentration.it is secreted in the human being by the thyroid gland from perifollicular cells. Calcitonin is a protein in nature. Functions of Calcitonin: Calcitonin Reduces plasma calcium concentration in three separate ways: 1.it reduces bone resorption by inhibiting osteoclast function.this result in a decrease in the concentration of both calcium and phosphate in serum. 2.it increases the urinary excretion of calcium ,phosphate,sodium,potassium,and magnesium. 3.the third and most prolonged effect of calcitonin is to decrease the formation of new osteoclast. Calcitonin has only a very weak effect on plasma calcium concentration in the adult human being. on the other hand,the effect in children is much more marked because bone remodeling occurs rapidly in children,with absorption and deposition of calcium. There are two major differences between the calcitonin and the parathyroid feedback system: 1.the Calcitonin mechanism operates more rapidly. 2.the Calcitonin mechanism acts mainly as a shortterm regulator of calium `ion concentration because it is very rapidly overridden by the much more powerful parathyroid control mechanism. Control of Calcitonin secretion: 1.increase in plasma calcium concentration of about 10%,causes an immediate three-to six fold increase in the rate of secretion of calcitonin. 2. dopamine and estrogens stimulates Calcitonin secretion. 3.gastrin.cck,glucagons and secretin stimulate Calcitonin secretion. ↑ Ca++ dopamine } estrogen } → ↓ Calcitonin → ↑ calcitonin