* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 5. KB_7.6 Physiology..
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Rheumatic fever wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Artificial heart valve wikipedia , lookup
Myocardial infarction wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart arrhythmia wikipedia , lookup
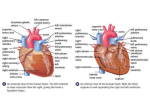
Dextro-Transposition of the great arteries wikipedia , lookup
Anatomy of the Heart KayOnda Bayo 1 2 2 Circuits Pulmonary •Heart lungs heart Systemic •Heart body heart 3 The heart=a muscular double pump with 2 functions 4 Overview The right side receives oxygen-poor blood from the body and tissues and then pumps it to the lungs to pick up oxygen and dispel carbon dioxide Its left side receives oxygenated blood returning from the lungs and pumps this blood throughout the body to supply oxygen and nutrients to the body tissues 5 Arteries • Carry blood away from heart • Except pulmonary arteries (carries deoxygenated blood) Veins • Carry blood to heart • Except pulmonary veins (carries oxygenated blood) 6 simplified… Cone shaped muscle Four chambers Two atria, two ventricles Double pump – the ventricles Two circulations Systemic circuit: blood vessels that transport blood to and from all the body tissues Pulmonary circuit: blood vessels that carry blood to and from the lungs 7 Heart’s position in thorax Heart’s position in thorax In mediastinum – behind sternum and pointing left, lying on the diaphragm It weighs 250-350 gm (about 1 pound) Feel your heart beat at apex (this is of a person lying down) 8 9 Coverings of the Heart Fibrous Pericardium Visceral Layer Parietal Layer 10 Layers of the Heart Pericardium Myocardium Endocardium 11 Pericardium (double-walled sac) Protects against infection Provides lubrication to the heart Fixes the heat to the mediastinum Myocardium Middle layer Contains many capillaries & nerve endings Has cardiac muscle forming the bulk of the heart – thickest layer Layer that contracts Endocardium Has an endothelial layer that lines the heart chambers Contains Perkinje fibers (specialized nerve fibers used during the heart beat) How Pericardium is Formed Around the Heart 12 Pericardial Cavity Between the parietal and visceral layer of the serous pericardium Contains serous fluid lubricates membranes to reduce friction *Pericarditis: inflammation of the pericardium that roughens the serous membrane surface 13 14 The Heart is enclosed within a double-walled sac called the pericardium. Consists of 2 layers Fibrous pericardium Serous pericardium Fibrous pericardium: Composed of dense connective tissue (protects the heart) Anchors to surrounding walls Prevents the heart from overfilling with blood Serous pericardium Located deep to fibrous pericardium Contains 2 layers function to lubricate the heart to prevent friction during activity 15 Heart Chambers There are 4 chambers in the heart 2 superior ventricles 2 inferior atria Atriums known as the receiving chamber Ventricles known as the discharging chambers 16 Chambers of the heart sides are labeled in reference to the patient facing you Two atria Right atrium Left atrium -------------------------------------------------------------------------------- Two ventricles Right ventricle Left ventricle Chambers of the heart divided by septae: Two atria-divided by interatrial septum Right atrium Left atrium Two ventricles-divided by interrventricular septum Right ventricle Left ventricle 17 Relative thickness of muscular walls 18 LV thicker than RV because it forces blood out against more resistance; the systemic circulation is much longer than the pulmonary circulation Atria are thin because ventricular filling is done by gravity, requiring little atrial effort 19 Pectinate muscles Auricle Atria +Fossa ovalis +Foramen ovale 20 The Fossa Ovalis is an embryonic remnant of the foramen ovale, which normally closes after birth. Following birth, the foramen ovale is covered by a fibrous sheet. Failure of the foramen ovale to close results in a disorder called patent foramen ovale. 21 Trabecular carneae Chordae tendineae Ventricles Papillary muscles 22 Heart Valves: Atrioventricular (AV) Valves Prevent backflow into the atria when the ventricles contract Both valves contains 3 cusps Tricuspid valve (right AV valve) has 3 flexible cusps Mitral valve (left AV valve) has 2 cusps a.k.a. “bicuspid valve” 23 Heart Valves: Semilunar (AV) Valves Prevent backflow into associated ventricles Aortic valve protects the orifice between the left ventricle and the aorta Pulmonary valve guards the orifice between the right ventricle and the pulmonary artery 24 Homeostatic Imbalance of Heart Valves Heart valves can function with “leaky” valves as long as the impairment is not too severe. Severe valve deformities can seriously hamper cardiac function. Problems with Valves: An incompetent valve forces the heart to pump the same blood over and over because the valve does not close properly. When stenosis occurs, the valve flaps become stiff and constrict the opening heart contracts more than normal In both conditions, the heart’s workload increases weakens the heart overtime Treatment: Heart valve is replaced with: • Mechanical Heart • Pig or cow valve (chemically treated to reduce rejection) 25 Blood Return to R-atrium Superior vena cava (SVC) Inferior vena cava (IVC) Coronary sinus (CS) Pathway of Blood Through the Heart 27 Pathway of Blood (cont.) Superior vena cava, Inferior vena cava, Coronary sinus Left Ventricle Right Atrium Mitral Valve Left Atrium Aortic Semilunar valve Aorta Rest of the Body Tricuspid valve Right Ventricl e 28 Pulmonary Semilunar valve 4 pulmonary veins Pulmonary Artery & Trunk Lungs Coronary Artery Circulation 29 Even though the heart is filled with blood, the blood provides little nourishment to the heart (the myocardium tissue is too thick). Blood is supplied to the heart via Coronary Circulation which is the shortest circulation in the body. Branching of Coronary Arteries Right Coronary Artery (RCA) Branches into: Right marginal artery Posterior descending artery Supplies: Right atrium Bottom portion of both ventricles and back of septum Together the RCA and its branches supply the R. Atrium and nearly all the ventricles. Left Coronary Artery (Left Main Trunk) Branches into: Circumflex artery Anterior interventricular artery Supplies: Circumflex Artery: left atrium, side and back of the left ventricle Anterior interventricular artery: front and bottom of the left ventricle and front of the septum 30 *What happens when a coronary artery is blocked? 31 Angina Pectoris Myocardial Infarction (MI) Homeostatic Imbalance of Coronary Blood Flow Partial blockade • Decreased blood flow ischemia angina • Treatment:???? Complete blockade • No blood flow myocardial infarction • Treatment: ????? 32 33 Cardiac Muscle Cell Characteristics Striated Involuntary control Short, fat branched, and interconnected One to two large, centrally located nuclei 34 Unique Characteristic of the Heart Some cardiac fibers are auto-rhythmic. These fibers have the ability to depolarize spontaneously and pace the heart. The bulk of the heart consists of contractile muscle cells that are responsible for the heart’s pumping activity. All cells of the heart MUST contract as a unit or the heart doesn’t contract at all. Gap junctions electrically tie all cardiac muscle together into a single contractile unit. Physiology of the Heart KayOnda Bayo 35 Contractile Cell Action Potential Four phases of action potential Resting membrane potential -90 mV Depolarization due to fast Na+ channels Plateau due to slow Ca2+ channels Repolarization due to K+ channels Action potential Plateau 20 2 0 Tension development (contraction) –20 –40 3 1 –60 Absolute refractory period –80 0 150(ms) Time 300 Tension (g) Membrane potential (mV) Contractile Cell A.P. 1 Depolarization is due to Na+ influx through fast voltage-gated Na+ channels. A positive feedback cycle rapidly opens many Na+ channels, reversing the membrane potential. Channel inactivation ends this phase. 2 Plateau phase is due to Ca2+ influx through slow Ca2+ channels. This keeps the cell depolarized because few K+ channels are open. 3 Repolarization is due to Ca2+ channels inactivating and K+ channels opening. This allows K+ efflux, which brings the membrane potential back to its resting voltage. © 2013 Pearson Education, Inc. Pacemaker Action Potential Present in SA & AV node Contains three phases Slow depolarization Unstable resting membrane potential Between -60 mV to -40 mV Pacemaker (Autorhythmic) Cells Unstable resting membrane potentials (pacemaker potentials) opening of slow Na+ channels Continuously depolarize At threshold, Ca2+ channels open Explosive Ca2+ influx rising phase of A.P. Repolarization inactivation of Ca2+ channels opening of voltage-gated K+ channels © 2013 Pearson Education, Inc. Pacemaker Action Potential Three phases of action potential: Pacemaker potential Repolarization closes K+ channels opens slow Na+ channels ion imbalance Depolarization Ca2+ channels open huge influx rising phase of A. P. Repolarization K+ channels open efflux of K+ © 2013 Pearson Education, Inc. Membrane potential (mV) Pacemaker Action Potential +10 0 –10 –20 –30 –40 –50 –60 –70 Action potential 2 Threshold 2 Depolarization The action potential begins when the pacemaker potential reaches threshold. Depolarization is due to Ca2+ influx through Ca2+ channels. 2 3 3 1 1 Pacemaker potential Time (ms) © 2013 Pearson Education, Inc. 1 Pacemaker potential This slow depolarization is due to both opening of Na+ channels and closing of K+ channels. Notice that the membrane potential is never a flat line. 3 Repolarization is due to Ca2+ channels inactivating and K+ channels opening. This allows K+ efflux, which brings the membrane potential back to its most negative voltage. Sequence of Excitation Cardiac pacemaker cells pass impulses, in order, across heart in ~220 ms Sinoatrial(SA) node Atrioventricular(AV) node Atrioventricular bundle Right and left bundle branches Subendocardial conducting network (Purkinje fibers) © 2013 Pearson Education, Inc. Heart Physiology: Sequence of Excitation Sinoatrial (SA) node Pacemaker of heart in right atrial wall Depolarizes faster than rest of myocardium Generates impulses 75X/minute (sinus rhythm) Inherent rate of 100X/minute Tempered by extrinsic factors Impulse spreads across atria, and to AV node © 2013 Pearson Education, Inc. Figure 18.15a Intrinsic cardiac conduction system and action potential succession during one heartbeat. Superior vena cava Right atrium 1 The sinoatrial (SA) node (pacemaker) generates impulses. Internodal pathway 2 The impulses pause (0.1 s) at the atrioventricular (AV) node. 3 The atrioventricular (AV) bundle connects the atria to the ventricles. 4 The bundle branches conduct the impulses through the interventricular septum. Left atrium Subendocardial conducting network (Purkinje fibers) Interventricular septum 5 The subendocardial conducting network depolarizes the contractile cells of both ventricles. Anatomy of the intrinsic conduction system showing the sequence of electrical excitation © 2013 Pearson Education, Inc. Heart Sounds Two sounds (lub-dup) associated with closing of heart valves First as AV valves close; beginning of systole ”lub” S1 Tricuspid & Bicuspid(Mitral) Valves Second as SL valves close; beginning of ventricular diastole “dup” S2 Aortic & PulmonaryValves Pause indicates heart relaxation Heart murmurs - abnormal heart sounds; usually indicate incompetent valves © 2013 Pearson Education, Inc. Figure 18.20 Areas of the thoracic surface where the sounds of individual valves can best be detected. Aortic valve sounds heard in 2nd intercostal space at right sternal margin. S2 Pulmonary valve sounds heard in 2nd intercostal space at left sternal margin. S2 Mitral valve sounds heard over heart apex (in 5th intercostal space) in line with middle of clavicle. S1 Tricuspid valve sounds typically heard in right sternal margin of 5th intercostal space. S1 © 2013 Pearson Education, Inc. Heart Sounds Two sounds associated with filling of ventricles(Inaudible) Rapid flow of blood from atria into ventricles S3 Normally heard in children Heard in adults associated with disease Inflow of blood into ventricles during atrial systole S4 Heard in disease state such as diastolic stiffness or high atrial pressure Cardiac Output (CO) Volume of blood pumped by each ventricle in one minute CO = heart rate (HR) × stroke volume (SV) HR = number of beats per minute SV = volume of blood pumped out by one ventricle with each beat Normal – 5.25 L/min © 2013 Pearson Education, Inc. Cardiac Output (CO) At rest CO (ml/min) = HR (75 beats/min) SV (70 ml/beat) = 5.25 L/min CO increases if either/both SV or HR increased Maximal CO is 4–5 times resting CO in nonathletic people Maximal CO may reach 35 L/min in trained athletes Cardiac reserve - difference between resting and maximal CO © 2013 Pearson Education, Inc. Regulation of Stroke Volume SV = EDV – ESV EDV affected by length of ventricular diastole and venous pressure ESV affected by arterial BP and force of ventricular contraction Three main factors affect SV: Preload Contractility Afterload © 2013 Pearson Education, Inc. Homeostatic Imbalance Hypocalcemia depresses heart Hypercalcemia increased HR and contractility Hyperkalemia alters electrical activity heart block and cardiac arrest Hypokalemia feeble heartbeat; arrhythmias © 2013 Pearson Education, Inc. Homeostatic Imbalances Tachycardia - abnormally fast heart rate (>100 beats/min) If persistent, may lead to fibrillation Bradycardia - heart rate slower than 60 beats/min May result in grossly inadequate blood circulation in nonathletes May be desirable result of endurance training © 2013 Pearson Education, Inc. Factors that Influence Heart Rate Age Fetus has fastest HR Gender Females faster than males Exercise Increases HR Body temperature Increases with increased temperature © 2013 Pearson Education, Inc. 54 QUESTIONS?