* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download pacemakercomp
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
Electrocardiography wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
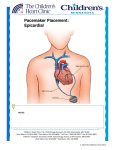
BMT414 Introduction to Biomedical Instrumentation (Part-1) Dr. Ali Saad, Department of Biomedical Technology College of Applied medical Sciences King Saud University. Contents Ch1- Defibrilators and cardioverters Ch2- Pacemakers- multivibrators Ch3- Electrosurgical unit and ablation Cardiac Pacemaker The contractions of the heart are controlled by electrical impulses, these fire at a rate which controls the beat of the heart. The cells that create these rhythmical impulses are called pacemaker cells, and they directly control the heart rate. Artificial devices also called pacemakers can be used after damage to the body's intrinsic conduction system to produce these impulses synthetically. SA NODE The sinoatrial node (abbreviated SA node or SAN, also called the sinus node) is the impulse generating (pacemaker) tissue located in the right atrium of the heart. Although all of the heart's cells possess the ability to generate the electrical impulses (or action potentials) that trigger cardiac contraction, the sinoatrial node is what normally initiates it, simply because it generates impulses slightly faster than the other areas with pacemaker potential. Because cardiac myocytes, like all muscle cells, have refractory periods following contraction during which additional contractions cannot be triggered, their pacemaker potential is overridden by the sinoatrial node. The sinoatrial node (SA node) is a group of cells positioned on the wall of the right atrium, near the entrance of the superior vena cava. These cells are modified cardiac myocytes. They possess some contractile filaments, though they do not contract. Cells in the SA node will naturally discharge (create action potentials) at about 70-80 times/minute. Because the sinoatrial node is responsible for the rest of the heart's electrical activity, it is sometimes called the primary pacemaker. If the SA node doesn't function, or the impulse generated in the SA node is blocked before it travels down the electrical conduction system, a group of cells further down the heart will become the heart's pacemaker. These cells form the atrioventricular node (AV node), which is an area between the atria and ventricles, within the atrial septum. The SA node is richly innervated by vagal and sympathetic fibers. This makes the SA node susceptible to autonomic influences. Stimulation of the vagus nerve causes decrease in the SA node rate (thereby causing decrease in the heart rate). Stimulation via sympathetic fibers causes increase in the SA node rate (thereby increasing the heart rate). In the majority of patients, the SA node receives blood from the right coronary artery, meaning that a myocardial infarction occluding it will cause ischaemia in the SA node unless there is a sufficiently good anastomosis from the left coronary artery. If not, death of the affected cells will stop the SA node from triggering the heartbeat. An action potential is a wave of electrical discharge that travels along the membrane of a cell. Action potentials are an essential feature of animal life, rapidly carrying information within and between tissues. They are also exhibited by some plants. Action potentials can be created by many types of cells, but are used most extensively by the nervous system for communication between neurons and to transmit information from neurons to other body tissues such as muscles and glands. pacemaker potential In realiIn the heart, the pacemaker potential is the voltage created by impulses from an artificial electronic pacemaker or the SA node which drives the rhythmic firing of the heart. The pacemaker potential brings the membrane potential to the threshold potential and initiates an action potential. ty, the heart has several pacemakers known as autonomic foci, each which fires at its own intrinsic rate: SA node 80 - 100 bpm Atrial foci 60 - 80 bpm Junctional foci 40 - 60 bpm Ventrical foci 20 - 40 bpm The potentials will normally travel in order SA node -> atrial foci -> junctional foci -> ventricular foci Pacemaker potentials are fired not only by SA node, but the other foci. However, the other firing frequencies are slower than the one of the AV node (as seen above). Normally, all the foci will end up firing at the SA node rate, not their intrinsic rate. The other foci attempt to fire at their intrinsic rate, but they are activated by the SA node before they can fire. This rapid firing causes all the foci to fire faster than their intrinsic rates, a phenomenon known as overdrive-suppression. Thus, in the normal, healthy heart, only the SA node intrinsic rate is observable. However, in pathological conditions, the intrinsic rate becomes apparent. Consider a heart attack which damages the region of the heart between the SA node and the atrial foci. SA node -> |block| atrial foci -> junctional foci -> ventricular foci The other foci will not see the SA node firing; however, they will see the atrial foci. The heart will now beat at the intrinsic rate of the atrial foci. The firing of the pacemaker cells is induced, as the firing of action potentials in any human action-potential rising cell (like nerve cells), electrically, by the reaching of the threshold potential of the cell membrane. It is reached by the constant increase of membrane potential (induced by the special "funny channel", which by its Na+-channel activity giving rise to a current, the "funny current"). Upon the reaching of the threshold potential, the action potential is fired, and then reset. Myocyte A muscle fiber (AE) or muscle fibre (BE) (also technically known as a myocyte) is a single cell of a muscle. Muscle fibers contain many myofibrils, the contractile unit of muscles. Muscle fibers are very long; a single fiber can reach a length of 30cm. Muscle fibres can be grouped according to what kind of tissue they are found in -skeletal muscle, cardiac muscle, and smooth muscle. Skeletal muscle fibers can be further divided into two basic types, type I (slow-twitch fibers) and type II (fast-twitch fibers). The muscle cells of heart muscle tissue are called cardiomyocytes. Atrioventricular node-- AV node The atrioventricular node (abbreviated AV node) is the tissue between the atria and the ventricles of the heart, which conducts the normal electrical impulse from the atria to the ventricles. The AV node receives two inputs from the atria: posteriorly via the crista terminalis, and anteriorly via the interatrial septum.[1] An important property that is unique to the AV node is decremental conduction. This is the property of the AV node that prevents rapid conduction to the ventricle in cases of rapid atrial rhythms, such as atrial fibrillation or atrial flutter. The atrioventricular node delays impulses for 0.1 second before spreading to the ventricle walls. The reason it is so important to delay the cardiac impulse is to ensure that the atria are empty completely before the ventricles contract (Campbell et al, 2002). The blood supply of the AV node is from a branch of the right coronary artery in 85% to 90% of individuals, and from a branch of the left circumflex artery in 10% to 15% of individuals. In certain types of supraventricular tachycardia, a person could have two AV Nodes; this will cause a loop in electrical current and uncontrollably-rapid heart beat. When this electricity catches up with itself, it will dissipate and return to normal heart-beat speed Artificial pacemaker History of the implantable pacemaker The first external pacemaker was designed and built by the Canadian electrical engineer John Hopps in 1950. A substantial external device, it was somewhat crude and painful to the patient in use. A number of inventors, including Paul Zoll, made smaller but still bulky external devices in the following years. The pacemakers built in the late 1950s were bulky, relied on external electrodes, and had to be plugged into a wall outlet. External electric shocks were frequently too traumatic for young heart block patients, and the AC-operated pacemaker could fail during a power blackout. The first implantation into a human was made in 1958 by a Swedish team using a pacemaker designed by Rune Elmqvist and Åke Senning. The device failed after three hours. A second device was then implanted which lasted for two days. The world's first implantable pacemaker patient, Arne Larsson, survived the first tests and died in 2001 after having received 22 different pacemakers during his lifetime. In February 1960, an improved model relying on better materials was implanted in Montevideo, Uruguay. That device lasted until the patient died of other ailments, 9 months later. The early Swedishdesigned devices used rechargeable batteries, which were charged by an induction coil from the outside. Devices constructed by the American Wilson Greatbatch entered use in humans from April 1960 following extensive animal testing. The first patient lived for a further 18 months. The early devices suffered from battery problems - every patient required an additional operation every 24 months to replace the batteries. Others who contributed significantly to the technological development of the pacemaker in the pioneering years were Bob Anderson of Medtronic Minneapolis, Geoffrey Davies of Devices Ltd in England, Barouh Berkovits and Sheldon Thaler of American Optical, Geoffrey Wickham of Telectronics Australia, Walter Keller of Cordis Corp. of Miami, Hans Thorander who joined previously mentioned Rune Elmquist of Elema-Schonander in Sweden, Janwillem van den Berg of Holland and Manuel A. Villafaña of Cardiac Pacemakers Inc. Pacemakers require wires (called leads) to both send the pacing pulses to the heart and sense the intrinsic rhythm of the heart. The first pacemakers required these leads to be placed surgically on the outer surface of the heart. In the mid 1960s, the first transvenous leads were placed. This allowed the placement of pacemakers without opening the thoracic cavity and therefore without the use of general anesthesia. The first American-made nuclear-powered pacemaker was developed and implanted by Victor Parsonnet at Newark Beth Israel Medical Center in Newark, New Jersey. The first pacemaker implanted into an infant was July 26, 1974 to Jason A. Haines when he was 16 hours old. [edit] Applications Artificial pacemakers can be used in order to help with and/or treat these conditions: Arrhythmias - an abnormal heartbeat Sick sinus syndrome - when the sinoatrial node does not fire properly to contract the heart Methods of pacing External pacing External pacemakers can be used for initial stabilization of a patient, but implantation of a permanent internal pacemaker is usually required for most conditions. External cardiac pacing is typically performed by placing two pacing pads on the chest wall. Usually one pad is placed on the upper portion of the sternum, while the other is placed along the left axilla, near the bottom of the rib cage. When an electrical impulse goes from one pad to the other, it will travel through the tissues between them and stimulate the muscles between them, including the cardiac muscle and the muscles of the chest wall. Electrically stimulating any muscle, including the heart muscle, will make it contract. The stimulation of the muscles of the chest wall will frequently make those muscles twitch at the same rate as the pacemaker is set. It was first invented by Canadian doctor John Hopps in 1950. He studied as an electrical engineer at the University of Manitoba. Pacing the heart via external pacing pads should not be relied upon for an extended period of time. If the person is conscious, he or she may feel discomfort due to the frequent stimulation of the muscles of the chest wall. Also, stimulation of the chest wall muscles does not necessarily mean that the heart is being stimulated as well. Temporary internal pacing An alternative to external pacing is the temporary internal pacing wire. This is a wire that is placed under sterile conditions via a central venous catheter. The distal tip of the wire is placed into either the right atrium or right ventricle. The proximal tip of the wire is attached to the pacemaker generator, outside of the body. Temporary internal pacing is often used as a bridge to permanent pacemaker placement. Under certain conditions, a person may require temporary pacing but would not require permanent pacing. In this case, a temporary pacing wire may be the optimal treatment option. [edit] Permanent pacemaker placement Placement of a permanent pacemaker involves placement of one or more pacing wires within the chambers of the heart. One end of each wire is attached to the muscle of the heart. The other end is screwed into the pacemaker generator. The pacemaker generator is a hermetically sealed device containing a power source and the computer logic for the pacemaker. Most commonly, the generator is placed below the subcutaneous fat of the chest wall, above the muscles and bones of the chest. However, the placement may vary on a case by case basis. The outer casing of pacemakers is so designed that it will rarely be rejected by the body's immune system. It is usually made of titanium, which is very inert in the body. [edit] Basic pacemaker function Modern pacemakers all have two functions. They listen to the heart's native electrical rhythm, and if the device doesn't sense any electrical activity within a certain time period, the device will stimulate the heart with a set amount of energy, measured in joules. [edit] Pacemaker naming code The NASPE/BPEG generic (NPG) code is a pacemaker naming convention originally developed in 1974 that uses a 3-5 letter code to describe the main features of an artificial pacemaker. Each of the 5 positions signifies a particular aspect of pacemaker functionality. Using this scheme, a designation of VATOO would describe, for example, a pacemaker that sensed the atria and paced the ventricles in a triggered mode with no rate response or multisite pacing. Position I II III IV Response Chamber(s) Chamber(s) Rate Category to Paced Sensed Response Sensing Code O = none, A = atrium, V= ventricle and D = dual (A + V) O = none, A = atrium, V= ventricle and D = dual (A + V) O= none, T = O = none, triggered, R = rate I= modulation inhibited and D = dual (T + V Multisite Pacing O= none, A = S= S= Manufacturer's atrium, single single designation V= (A or (A or only ventricle V) V) and D = dual (A I) + V) Table I. The Revised NASPE/BPEG Generic Code for Antibradycardia Pacing [edit] Bi-Ventricular Pacing (BVP) A bi-ventricular pacemaker, also known as CRT (Cardiac Resynchronization Therapy) is a type of pacemaker that can pace both ventricles (right and left) of the heart. By pacing both sides of the heart, the pacemaker can resynchronize a heart that does not beat in synchrony, which is common in heart failure patients. CRT devices has three leads, one in the Atrium, one in the right ventricle, and the last one is inserted through the coronary sinus to pace the left ventricle. CRT devices are shown to reduce mortality and improve quality of life in groups of heart failure patients.2,3 [edit] Advancements in pacemaker function When first invented, pacemakers controlled only the rate at which the heart's two largest chambers, the ventricles, beat. Many advancements have been made to enhance the control of the pacemaker once implanted. Many of these enhancements have been made possible by the transition to microprocessor controlled pacemakers. Pacemakers that control not only the ventricles but the atria as well have become common. Pacemakers that control both the atria and ventricles are called dual-chamber pacemakers. Although these dual-chamber models are usually more expensive, timing the contractions of the atria to precede that of the ventricles improves the pumping efficiency of the heart and can be useful in congestive heart failure. Rate responsive pacing allows the device to sense the physical activity of the patient and respond appropriately by increasing or decreasing the base pacing rate via rate response algorithms. The DAVID trial4 have shown that unnecessary pacing of the right ventricle can lead to heart failure. New devices can keep the amount of right ventricle pacing to a minimum and thus prevent worsening of the heart disease. Another advancement in pacemaker technology is left ventricular pacing. A pacemaker wire is placed on the outer surface of the left ventricle, with the goal of more physiological pacing than what is available in standard pacemakers. This extra wire is implanted to improve symptoms in patients with severe heart failure. [edit] Devices with pacemaker function Sometimes devices resembling pacemakers, called ICDs (implantable cardioverterdefibrillators) are implanted. These devices are often used in the treatment of patients at risk for sudden cardiac death. An ICD has the ability to treat many types of heart rhythm disturbances by means of pacing, cardioversion,or defibrillation. Complementary informations catheter In medicine, a catheter is a tube that can be inserted into a body cavity duct or vessel. Catheters thereby allow drainage or injection of fluids or access by surgical instruments. The process of inserting a catheter is catheterization. In most uses a catheter is a thin, flexible tube: a Central venous catheter In medicine, a central venous catheter (CVC or central (venous) line) is a catheter placed into a large vein in the neck, chest, or groin. Most commonly used veins are the internal jugular vein, the subclavian vein and the femoral vein. This is in contrast to a peripheral line which is usually placed in the arms or hands. The Seldinger technique is generally employed to gain central venous access. A tine is a process of metal, or a prong, often used to spear, hook, or otherwise carry other objects. A fork may have two, three, or more tines. Typically, the tines on a fork intended for use as an eating utensil are rather blunt. However, on other objects that have tines, the tines may be quite sharp. Winding (to turns coil) suture (plural sutures) Singular suture Plural sutures 1. Seam formed by sewing two edges (esp. of skin) together. 2. Thread used to sew two edges