* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download heart
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Artificial heart valve wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
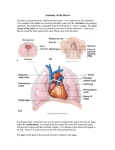
Lec1: Dr.Saba kh. The Cardiovascular System The cardiovascular system Responsible for transporting oxygen, nutrients, hormones, and cellular waste products throughout the body, cardiovascular system consists of the heart, blood vessels, and the approximately 5 liters of blood that the blood vessels transport. the The heart is a muscular organ in humans and other animals, The heart is located in the middle compartment of the chest. about the size of a closed fist is situated in the middle mediastinum, at the level of thoracic vertebrae T5-T8. A double-membraned sac called the pericardium a protective sac, the pericardium, which also contains a small amount of fluid. the heart and attaches to the mediastinum. The back surface of the heart lies near the vertebral column, and the front surface sits behind to the sternum and rib cartilages.[ heart which pumps blood through the blood vessels of the circulatory system Blood provides the body with oxygen and nutrients, as well as assists in the removal of metabolic wastes. Heart Anatomy Chapter 18, Cardiovascular System 8 18.1 Figure In humans, other mammals, and birds, the heart is divided into four chambers: upper left and right atria; and lower left and right ventricles. Commonly the right atrium (A-tre-a; singular, atrium;“chamber”) and ventricle are referred together as the right heart and their left counterparts as the left heart. In a healthy .heart blood flows one way through the heart due to heart valves, which prevent backflow. • Tricuspid valve controls blood flow between the right atrium and ventricle • Mitral valve controls blood movement between the left atrium and ventricle • Pulmonary valve controls blood movement from right ventricle into pulmonary artery . The aortic valve controls blood flow from the left ventricle to the aorta. Pulmonary circulation Blood enters the right atrium from the veins vena cava. There are two vena cava. The inferior vena cava takes blood from the lower part of the body to the right side of the heart. The superior vena cava takes blood from the upper part of the body to the heart and passes through the tricuspid valve into the right ventricle, the pulmonic valve closes to prevent regurgitation of blood back into the right ventricle.. The right ventricle contracts, expelling blood through the pulmonic valve into the pulmonary artery on its way to the lungs. As the right ventricle contracts, the tricuspid valve closes, preventing regurgitation of blood into the right atrium. Know the basic sequence of how the blood flows The double pump Systemic circulation Following right ventricular contraction Reoxygenated blood returns from the lungs by way of the pulmonic veins and enters the left atrium. Blood flows through the open mitral valve into the left ventricle. After the left ventricle fills, it contracts sending blood through the aortic valve into the aorta and the rest of the body. As the left ventricle contracts, the mitral valve closes to prevent regurgitation into the left atrium. After left ventricular contraction, the aortic valve closes to prevent regurgitation of blood from the aorta back into the left ventricle • Aorta: The main trunk of the systemic arteries, carrying blood from the left side of the heart to the arteries of all limbs and organs. • Pulmonary Artery carries blood to lungs Aorta pulmonary artery Left Atrium Right Atrium Right Ventricle Left Ventricle • Functional Parts of the Circulation The function of the arteries is to transport blood under high pressure to the tissues .for this reason the arteries have strong vascular walls ,and blood flows at a high velocity in the arteries the arterioles are the last small branches of the arterial system ;they act as control conduits through which blood is released into the capillaries. The function of the capillaries is to exchange fluid ,nutrients ,electrolytes, hormones, and other substances between the blood and the interstitial fluid .To serve this role ,the capillary walls are very thin ,and have numerous minute capillary pores permeable to water and other small molecular substances . The venules collect blood from the capillaries,and they gradually coalesce into progressively larger veins.The veins function as conduits for transport of blood from the venules back to the heart ;they serve as a major reservoir of extra blood .because the pressure in the venous system is very low, the venous walls are thin. Structure of the Heart Wall A section through the wall of the heart reveals three distinct layers: (1) an outer epicardium (visceral pericardium), (2) a middle myocardium, and (3) an inner endocardium. 1. The epicardium is the visceral pericardium; it forms the external surface of the heart. The epicardium is a serous membrane consisting of a mesothelium covering a supporting layer of areolar connective tissue. The pericardium is the serous membrane lining the pericardial cavity. 2. The myocardium consists of multiple, interlocking layers of cardiac muscle tissue, with associated connective tissues, blood vessels, and nerves. The relatively thin atrial myocardium contains layers that form figure-eights as they pass from atrium to atrium. The ventricular myocardium is much thicker, and the muscle orientation changes from layer to layer. Superficial ventricular muscles wrap around both ventricles; deeper muscle layers spiral around and between the ventricles from the attached base toward the free tip, or apex, of the heart 3. The inner surfaces of the heart, including the valves, are covered by a simple squamous epithelium, known as the endocardium The endocardium is continuous with the endothelium of the attached blood vessels. Pericardial Layers of the Heart Chapter 18, Cardiovascular System 34 18.2 Figure Coronary Blood Vessels The heart works continuously, and cardiac muscle cells require reliable supplie of oxygen and nutrients. The coronary circulation supplies blood to the muscle tissue of the heart. During maximum exertion, the oxygen demand rises considerably, and the blood flow to the heart may increase to nine times that of resting levels. The coronary circulation .includes an extensive network of coronary blood vessels. The left and right coronary arteries originate at the base of the ascending aorta, within the aortic sinus, as the first branches of this vessel. Blood pressure here is the highest found anywhere in the systemic circuit, and this pressure ensures a continuous flow of blood to meet the demands of active cardiac muscle tissue The Conducting System of the Heart (a) The stimulus for contraction is generated by pacemaker cells at the SA sinoatrial node( pacemaker cells).From there, impulses follow three different paths through the atrial walls to reach the AV node. the impulse they produce will bring all other nodal cells to threshold. These rapidly depolarizing cells are found in the sinoatrial (si-no-A-tre-al) node (SA node), or cardiac pacemaker. The SA node is embedded in the posterior wall of the right atrium, near the entrance depolarize rapidly and spontaneously, generating 80–100 action potentials per minute. . The stimulus affects only the atria, because the fibrous skeleton electrically isolates the atrial myocardium from the ventricular myocardium. The AV node sits within the floor of the right atrium near the opening of the coronary sinus. Due to differences in the shape of the nodal cells, the impulse slows as it passes through the AV node. From there, the impulse travels to the ventricles. AV bundle, also known as the bundle of His (HISS). This rather massive bundle of conducting fibers travels along the interventricular septuma short distance before dividing into a right bundle branch and a left bundle branch that extend toward the apex and then radiate across the inner surfaces of both ventricles. At this point, Purkinje (pur-KIN-je) cells (Purkinje fibers) convey the impulses very rapidly to the contractile cells of the ventricular myocardium. The conducting fibers of the moderator band relay the stimulus to the papillary muscles, which tense the chordae tendineae before the ventricles contract. The stimulus for a contraction is generated at the SA node, and the anatomical relationships among the contracting cells, the nodal cells, and the conducting fibers distribute the impulse so that (1) the atria contract together, before the ventricles, and (2) the ventricles contract together in a wave that begins at the apex and spreads toward the base.When the ventricles contract in this way, blood is pushed toward the base of the heart and out into the aortic and pulmonary trunks. 39 A number of clinical problems are the result of abnormal pacemaker function. Bradycardia is the term used to indicate a heart rate that is slower than normal, whereas a faster-thannormal heart rate is termed tachycardia . Both terms are relative, and in clinical practice the definition varies depending on the normal resting heart rate and conditioning of the individual. The Electrocardiogram (ECG) The electrical events associated with the depolarization and repolarization of the heart are powerful enough to be detected by electrodes placed on the body surface. A recording of these electrical activities constitutes an electrocardiogram (e-lek-tro-KAR-de-o-gram), also called an ECG. During each cardiac cycle, a wave of depolarization radiates through the atria, reaches the AV node, travels down the interventricular septum to the apex, turns, and spreads through the ventricular myocardium toward the base. This electrical activity can be monitored from the body surface. By comparing the information obtained from electrodes placed at different locations, one can monitor the performance of specific nodal, conducting, and contractile components. For example, when a portion of the heart has been damaged, as after an MI, these cardiac muscle cells can no longer conduct action potentials, so an ECG will reveal an abnormal pattern of electrical conduction. The appearance of the ECG tracing varies, depending on the placement of the monitoring electrodes, or leads .shows the important features of a representative electrocardiogram. The P wave accompanies the depolarization of the atria. The QRS complex appears as the ventricles depolarize. This electrical signal is relatively strong because the mass of the ventricular muscle is much larger than that of the atria. The smaller T wave indicates ventricular repolarization.You do not see a deflection corresponding to atrial repolarization because it occurs while the ventricles are depolarizing, and the electrical events are masked by the QRS complex.