* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
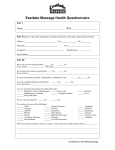
Survey
Document related concepts
Transcript
THE FOLLOWING LECTURE HAS BEEN APPROVED FOR ALL STUDENTS BY BIRMINGHAM CITY UNIVERSITY This lecture may contain information, ideas, concepts and discursive anecdotes that may be thought provoking and challenging Any issues raised in the lecture may require the viewer to engage in further thought, insight, reflection or critical evaluation health.bcu.ac.uk/craigjackson Psychosocial Aspects of Whiplash Injury Craig Jackson Prof. of Occupational Psychology Head of Division of Psychology BCU Whiplash Harold Crowe in 1928, first used term to describe movement of neck in accident Acceleration then Deceleration Now describes “injuries” induced by this motion Arthur E Davis in Erie, Penn. first used term in 1945 “Most patients recovered well” Used in 1953 in relation to auto-accidents (Gay & Abbott) Used the term “psychoneurotic reaction” to explain delayed recovery RTA Figures RTA Figures Kills: Injured: 1,200,000 per year 10,000,000 per year RTA most common cause of Head Injury Most Head Injuries are mild Many left with long-lasting problems Young males at biggest risk – alcohol often implied Data suggests female drinking habits catching up with males Implications for Female RTAs? RTA Figures 80% of serious RTA injury is to head 1 concussion every 15 seconds in USA Head Injury major cause of death and injury in RTAs 15,000,000 Brain Injuries per year in USA RTAs Playgrounds Sports 1990 - 5,563,000 intra-cranial injuries worldwide from RTA Murray et.al 1996 Psychological de-briefing after RTAs may help Hobbs et.al 1996 RTA Figures Mechanics of Occupant RTAs Hazards: Steering wheel / column Instrument panel Seatbelt Windscreens RTA Brain injuries Contre-Coup Concussion Intracranial Haematoma – Epidural, Intracerebral, Subdural Diffuse axonal injury How are Brain Injuries Assessed? PAA Post Accident Amnesia – memory problems when regaining consciousness • Minor Brain Injury Unconscious for < 15 mins • Moderate Brain Injury Unconscious > 15 mins but < 6 hrs + PTA < 24 hrs • Severe Brain Injury Unconscious > 6 hrs OR PTA > 24 hrs • Very Severe Brain Injury Unconscious > 48 hrs OR PTA > 7 days Mechanics of Whiplash Hyperextension HyperFlexion Majority of cases, no injury can be identified Symptoms attributed to musculo-ligamental sprain Mechanics of Whiplash Accelerating Phase Duration Acceleration Head-Neck Movement Phase 1 0-60 msec. 0g Rest State Phase 2 60-120 msec. 0.3 g Head rise, neck flexion and backbone extension Phase 3 120-200 msec. 4.3 g Neck extension Phase 4 200-300 msec. 2.8 g Head and neck hyperextension Phase 5 300-400 msec. 1.0 g Head forwards with neck flexion (whiplash) Phase 6 starting + de 400 msec. 0.8 g Little flexion, back to position Whiplash Associated Disorder Transfer of energy into the neck May result from rear-end or side impact collision Can occur with other accidents Impact of injury can occur on soft tissue and bone in the neck Can lead to a variety of clinical presentations known as WAD Whiplash injury feasible at 5 MPH 85% of UK RTA injury insurance claims Whiplash Statistics USA 1995: 5.5 million people involved in traffic accidents 53% of them suffered whiplash injury Germany 1992: 395,462 traffic accidents 197,731 (49%) suffered whiplash injury Whiplash as a “Pseudo Psychiatric” Condition? American Psychological “dissimulating” disorders Association recognises 1. Malingering 2. Somatoform disorders 3. Factitious disorders Doctors, alternative practitioners, scientists, lawyers, and patients have colluded in promoting a disorder that now afflicts millions and costs billions While patients who sustain serious neck injuries have a good prognosis minor collisions producing no demonstrable tissue damage now result in lifelong disability in around 10% of cases 3 types Whiplash as a “Pseudo Psychiatric” Condition? One of a family of fashionable conditions, including: Fibromyalgia Repetitive strain injury Chronic fatigue syndrome Occupational back pain Chronic pain syndrome Are these diagnoses are offered to patients who are either consciously or unconsciously seeking an escape from the pressures of modern life into the roles of sickness and victimhood? Do these conditions risk degrading medicine and bankrupting health services? Worst of all, they condemn patients to disorders from which there is little hope of recovery Malleson 2002 Prevention is OK Lots of research in area of whiplash injury prevention Cars better at preventing injury than ever before Not much known about prevention of chronic pain after incident Some treatment may foster chronic pain Quebec Task Force on Whiplash Extensive literature review of work from 1980 – 1993 10,382 papers examined Only 62 (0.6%) were relevant and scientifically good Papers before 1980 generally of little clinical / scientific value Pathophysiology – a Sprain Majority of whiplash injuries arise in soft tissue injury to neck involving ligaments, joints, joint capsules, muscles and tendons Type 1: Injury at microscopic level without altering structure Type 2: Partial tear at macroscopic level no separation Type 3: Severe stretching and tearing with separation of tissues Whiplash Associated Disorders (WAD) Classed by severity of signs and symptoms WAD 0 No complaints or physical signs WAD 1 Neck complaints but no physical signs WAD 2 Neck complaints and musculoskeletal signs WAD 3 Neck complaints and neurological signs WAD 4 Neck complaints and fracture / dislocation Most whiplash injury results from low impact collisions Prolonged and Escalated Symptoms Excess stress Psychosocial difficulties Anxiety (approx 40%) Depression (approx 40%) PTSD Poor sleep Ear pain Poor posture Dizziness Memory problems Concentration problems Headaches Movement difficulty 10% have WAD symptoms for > 2 years after accident: Caused by. . . Poor sleep Depression, Anxiety, Stress Psychosocial difficulties Pre-existing conditions Inappropriate therapeutics Prolongation of litigation Post Traumatic Fibromyalgia? Saskins & Moldofsky 1986 11 cases of PTFS Generalised pain on 11 of 18 designated tender points A happy marriage of Whiplash and Fibromyalgia? Post Traumatic Fibromyalgia abandoned in 1994 Wolfe 1996 Chronic Whiplash Complex interaction between many factors: Biological Psychosocial Economics Legal Beliefs / Attitudes Psychological factors are also hypothesized to influence the existence of whiplash-related cognitive impairments. Other Countries 1 Mills & Horne 1986 – New Zealand Very low incidence Significantly lower than Australia Difference in process of dealing with: insurance companies lawyers therapists Awerbuch 1992 - Australia WAD claims dropped from 6000 to 2000 / year in 1987 Legislative changes limited compensation and claim sizes Claimants had to: bear initial cost of claim report to police have minimum 30% disability Other Countries 2 Cassidy et.al 1995 – Canada 27% reduction in claims under a “no fault system” in courts Statute of limitations to 200 days after accident “No Crash No Cash” Obelieniene 1999 – Lithuania No notion of chronic pain resulting from rear end collision No fear of long term disability No involvement of lawyers Partheni et.al 1997 – Greece 91% of WAD victims recover in 4 weeks Treatments – Quebec Task Force (1995) Most studies show little or no efficacy of treatments Collar and NSAIDs on short term basis Avoid long term physiotherapy Mobilization by trained person & active exercise for grade 2 & 3 Drugs for insomnia or anxiety Early return to activities and promote mobility Myths about Whiplash 1. “Whiplash Personality” 2. Malingering (for monetary gain) is common 3. Illness & Disability are biological phenomena 4. Men are more vulnerable than women 5. Direct impact upon neck is necessary for WAD 6. X-ray shows nothing so no WAD 7. Complaints are psychosomatic 8. Rest, time, muscle relaxants and tranquillisers cure the distress 9. Seatbelts would prevent injury Case Summary of a Whiplash Patient Male, Age 34. Head Injury, Whiplash, Headaches, Sleep Disorder, Fatigue. Suffered a head injury during an auto accident in which he was rear-ended at 50mph. He described severe pain in his neck and back and headaches that originated at the base of his skull and spread to his left eye. His pain was so severe that it prevented him from sleeping, so he suffered from severe fatigue. To maintain some level of function during the day, he relied on multiple caffeinated beverages such as jolt or bull colas and/or coffee. At the time of his initial upper cervical chiropractic evaluation (14 months after the accident), he had been suffering with all of the above symptoms for over a year. He had sought help from numerous practitioners including physicians, neurologists, and therapists, to no avail. He reported receiving some temporary relief from Pilates. Case Summary of a Whiplash Patient Female, Age 56. Neck Pain, Headaches, Chronic Fatigue. Suffered from chronic neck pain, headaches, and fatigue for years. She thought the problems may have started sometime after an auto accident she experienced 14 years before. During the accident, she was hit head-on and totalled her car. The pain bothered her on and off for years-- sometimes on a daily basis and other times a month would go by without pain. She tried many practitioners such as massage therapists and chiropractors and received some relief but still the problem continued year after year. Finally, after struggling over a decade, she sought help from upper cervical chiropractic care. Case Summary of a Whiplash Patient Female. Age 52. Migraine Headaches, Neck Pain, Whiplash, Head Injury. Involved in two auto accidents three years apart. The first accident (she was rear-ended) caused migraines, neck pain, and head injury symptoms, including insomnia, depression, memory loss, and inability to multi-task. These symptoms were worsened after her second auto accident in which she was also rear-ended. She tried multiple therapies including physical therapy, chiropractic care, cranial sacral therapy, as well as medications from her neurologist but she could hardly function due to severity of her cognitive symptoms and pain. Case Summary of a Whiplash Patient Female, Age 49. Headaches, Neck Pain, Loss of Sense of Taste Involved in 6 different auto accidents during a 5-year period. After each accident, she suffered increased pain in her neck and head. Her third accident was most severe in that she suffered a head injury. After that accident, in addition to experiencing an increase in pain, she lost her sense of taste. Her neurologist told her the damage to the nerves controlling taste was most likely permanent and due to the head injury. She tried many forms of treatment over the years including pain pills, chiropractic care, and physical therapy. Sometimes she received benefit, sometimes not, but the results were never consistent or long lasting. After struggling for 8 years with headaches and neck pain and 6 years with loss of her sense of taste, she sought help from upper cervical chiropractic care. Chronic Patient’s Attributions of Ill-Health Work Environment Chemicals Stress Toxins Virus Allergies Anatomy / Ergonomic Traumatic injury Non-Traumatic injury Living in a litigious society “Victim” culture Living in a “risk-controlled” world Someone must therefore always be to blame Urgency of Treatment? Poor knowledge of management of acute whiplash symptoms Best early treatment involves: 1) Frequently repeated active sub-maximal movements 2) Mechanical diagnosis 3) Therapy More effective in reducing pain than standard program of: a) Initial rest b) Use of a soft collar c) Gradual self-mobilization This therapy could be performed as home exercises initiated and supported by a physiotherapist Rosenfeld et.al 2000 Treatment For Patients – Cochrane Review 2004 15 studies met the inclusion criteria – only 3 were good quality Overall a poor methodological quality Passive & Active interventions more effective than no treatment Found conflicting evidence about the effectiveness of active interventions compared to passive ones Data of the high quality studies were conflicting ‘Rest makes rusty', can no longer be justified There is a suggestion that active interventions are more effective than passive ones, but no clear conclusion about chronic WAD can be drawn. Predictors of Disability in Patients Reported frequencies of disability ranging from 0% to 50% in follow-up studies After 1 year, (7.8%) persons with whiplash injury had not returned to usual level of activity or work Initiation of lawsuit within first month after injury did not influence recovery The cervical range-of-motion test has a high sensitivity in prediction of handicap after acute whiplash injury Kasch et.al 2001 WAD patients' self-efficacy at an early stage after injury significantly predicts the development of pain intensity and disability. Patients' confidence in performing daily activities should be reinforced in order to optimize treatment after injury Kyhlback et.al 2002 Cognitive Dysfunction in Patients Bosma & Kessells 2002 WAD Patients often experience cognitive impairments Neuro(psycho)logical test results do not always support this WAD Patients performed similarly to neurology patients on the cognitive tasks and performed worse on memory and attention tasks compared with the control group WAD Patients had high scores on subscales measuring somatization and displayed a palliative coping style Somatization, in combination with inadequate coping, might play a role in the development, persistence, or aggravation of whiplash-related symptoms, such as pain or cognitive dysfunction. Prognostic Factors in Patients Malt & Sundet 2002 15% of WAD patients suffer long lasting health problems 5% do not return to work Psychosocial impairment following injury is influenced by: Symptom Formation Vulnerability Biomechanical Low mental ability Past mental illness Older age Female Narrow spinal canal Neural structures Joints Musculature Musculature Acute stress response Head position @ impact Manual work, expectation of disability and an ongoing compensation claim case seem to be important moderator variables affecting symptom formation Prognostic Factors in Patients Psychological factors more important than crash parameters (e.g. velocity) in predicting course of WAD at 6 months Greater initial pain or symptoms persisting for 28 days were associated with reduced QoL and PTSD symptoms Richter et.al 2004 Stress at time of accident predicted > symptoms at follow-up Long-lasting distress and poor outcome were more related to the occurrence of stressful life events than to clinical and paraclinical findings Karlsborg et.al 1997 Prognostic Factors in Patients WAD patients 2 times sensitive to cold in neck Overall elevated level of distress > in the WAD gp than controls Neither vibration or heat caused different responses Pain in response to non-noxious stimulation over presumably healthy tissues suggests that central mechanisms are responsible for ongoing pain in at least some whiplash patients Moog et.al 2002 WAD patients have lower pain thresholds for electrical stimulus Hypersensitivity to peripheral stimulation in WAD patients Curatolo et.al 2001 Hassles and Daily Problems in Patients “Everyday Problem Checklist” (EPCL) scores were higher in WAD patients than healthy controls Chronic WAD patients report a high stress load WAD patients (especially those with a low educational level) appear to be more vulnerable and react with more distress than healthy people to all kinds of stressors Stress responses probably play an important role in the maintenance or deterioration of whiplash-associated complaints Blokhorst et.al 2002 Anxiety and Depression in Patients Depression & Anxiety 2 years before accident, significantly overlaps with WAD patients Wenzel et.al 2002 Depression & Anxiety greater in WAD patients than controls Those with longest history of pain gave highest ratings of pain Those with longest history of pain were most depressed Most of these patients were involved in litigation. Whiplash injury sufferers are anxious and depressed Their psychological distress could be aggravated by litigation Lee et.al 1993 Pre-injury Psychiatry in Patients Outcome measured for 33 WAD patients and correlated with a range of pre-accident variables No association between pre-accident psychiatric factors and overall outcome Older age and pre-accident history of MSD complaints correlated with physical and psychiatric outcomes Pre-accident psychiatric factors may have little bearing on longterm prognosis Outcome of late whiplash syndrome is probably worse in older individuals and in patients with a pre-accident history of MSD complaints Turner et.al 2003 Expectation of Problems in Patients Compared self-reported outcomes of physicians and nonphysicians Physicians Non-Physicians Recall being in RTA? 71% 60% Recall acute symptoms? 31% 46% 9% 32% Symptoms lasting > 1 year? Physicians symptoms were shorter than non-physicians Physicians appear, however, to be more resistant than nonphysicians to the progression from acute pain to chronic pain and disability. Virani et.al 2001 Cognitive Model of Physical Symptoms in WAD Preventing Chronicity of Pain Teach professionals Educate patients Avoid anxiety provoking terms e.g. “PTFS” or “disc bulge” Avoid excessive investigation & test – Iatrogenesis Be rational Avoid prolonged litigation involvement Make patient aware of lengthy outcomes of litigation Patient Education Explain benign nature of WAD Avoid confusing and conflicting info Watch for factors leading to pain chronicity Home / work programmes as effective as physiotherapy Teach relaxation and stress management Educate posture and neck care Ergonomics at home and work Home program of heat and cold & exercises Self Monitor stress, sleep and mood Headaches Avoid excessive investigation Acute Rational Care Take good history Physical examination X-ray of cervical spine Analgesics and muscle relaxants Use of local cold and heat Cervical collar for a few days NSAIDS for few weeks Gradual mobilization Correction of disturbed sleep Compensation Neurosis Pending litigation Treatment results often poor Some overt malingering Exaggerated illness due to: suggestion + somatization rationalization + distorted sense of justice victim status + entitlement beliefs Adverse legal / admin. systems Harden patient’s convictions With time, care-eliciting behaviour may remain permanent Bellamy, 1997 Compensation Neurosis Improvement in health..... ...may result in loss of status Patient compelled to guard against getting better Financial reward for illness is a powerful nocebo Exacerbates illness In a litigious society, will compensation neurosis become more widespread? Accident Neurosis Failure to improve with treatment until compensation issue settled Accident must occur in circumstances with potential for compensation payment Inverse relationship to severity of injury - Accident neurosis rare in cases of severe injury Low socio-economic status favors accident neurosis Complete recovery common compensation issue ? ? ? following settlement of Miller 1961 Abnormal Illness Behaviour after Compensable Injury Accident neurosis Aftermath neurosis Attitudinal pathosis Compensatory hysteria Compensation neurosis Functional overlay Greenback neurosis Justice neurosis Post accident anxiety syndrome Postaccident fibromyalgia Profit neurosis Railway spine Traumatic hysteria Traumatic neurasthenia Triggered neurosis Vertebral neurosis Whiplash neurosis Accident victim syndrome American disease Barristogenic illness Compensationitis Fright neurosis Greek disease Invalid syndrome Perceptual augmenter Pensionitis Post-traumatic syndrome Psychogenic invalidism Secondary gain neurosis Symptom magnification syndrome Traumatic neurosis Unconscious malingering Wharfie’s back Mendelson, 1984 Secondary Gain Pre-disposition Potential Claimants • Military patients nearing severance • Workers under retirement age • Workers soon to be made redundant •Low job satisfaction • Members of support groups Non-economic motivation Loneliness Depression Anxiety Difficulty expressing emotional pain Previous history of attention seeking when ill Summary of Whiplash Most common injury following RTA (Spitzer et al. 1995) Sufferers no more likely to be worriers or have psychiatric problems than non-suffers who had RTAs Sufferers more likely to find an accident frightening and be the innocent party than non-suffers who had RTAs 33% of sufferers have psychiatric complications at 1 year after accident No “psychology of whiplash” – many physical and psychological interactions combine together to produce a complicated clinical problem Finally. . . It’s a sexual thing – theory that anal retentive people (especially females) find being shunted / rear-ended to be distressing Is psychoanalytic theory any more unlikely than that of other whiplash theories ? ? ?