* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download No Slide Title
DNA vaccination wikipedia , lookup
Inflammation wikipedia , lookup
Immune system wikipedia , lookup
Acute pancreatitis wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adaptive immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Hepatitis B wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
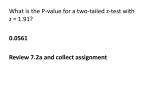
X-linked severe combined immunodeficiency wikipedia , lookup
Introduction and Approach to Transplantation Pathology Disclosures • Omnyx – Clinical development team and potential for eventual equity shares • Wyeth - Consultant • Bristol-Myers Squibb - Consultant • DCL/Novartis - Consultant Transplant Pathology General Considerations • Allograft pathology (and reporting) is the same as native organ pathology, except for syndromes unique to the allograft: – – – – – Preservation/reperfusion injury Rejection Opportunistic viruses Malignancies GVHD • Final diagnosis is based on extensive clinicopathologic diagnosis • More than one insult can contribute to the injury and diagnostic hierarchy should be assigned, if possible. • Pathophysiologic approach usually trumps morphological approach, but combination is best Rejection is a Process not a specific type of immune response! • Immune system redundancy and complexity enables many different pathways for organ damage/destruction • Similarities among individuals enables gross classification into T-cell mediated and AMR • Various immunologic effector mechanisms are more or less accentuated in individual patients • Changes in immunosuppressive therapy: – Affect the timing, severity, or histopathologic quality of rejection – Newer “biologically-based” IS agents are creating unique immunologic conditions and deficiencies (unusual infections at unusual sites). Leukocyte Migration Peripheral and Central Recognition (Demetris et al Early events in liver allograft rejection: Am J Pathol 1991; 138: 609) – Donor leukocytes travel to recipient lymphoid tissues • Immunologic “imprint” varies with organ – Recipient leukocytes infiltrate organ – Genetic non-identity triggers proliferation and apoptosis • Leads to: – Acute rejection – Regulatory responses • Treg, apoptosis, etc. Adaptive Immunity and T Lymphocytes • Naïve T lymphocytes (CD45RA) – Longer response time, might require central lymphoid tissue, less potent effector functions • Memory T lymphocytes (CD45RO) – Shorter response time, activated in organs, more potent effector functions – Generated by: • Previous exposure to alloantigen – Blood transfusion or other tissue tx; pregnancy • Infection/molecular mimicry – Pathogen-specific T cells cross-react with alloantigens • Homeostatic Proliferation – Natural or iatrogenic lymphopenia induces proliferation of residual cells, many of which have Tm phenotype Immunosuppression Strategies Steroid bolus P.R.N. Prednisone Tacrolimus Ab-depletion Rx Immune Responses Irreversible Rejection More Agspecific clonal deletion Pretreatment Tx Epitope spreading Homeostatic proliferation Classification of Rejection • Antibody-mediated Rejection (AMR) – Early after Tx can be catastrophic (hyperacute) – Later onset usually associated with activation of development of memory cells, poorer response to therapy and diminished survival – Major contributor to chronic rejection • Acute or T Cell-Mediated – Most episodes occur within 6 months; later in inadequately immunosuppressed patients. – Sub-classified by severity and whether there is overlap with antibody-mediated rejection • Chronic Rejection – Usually occurs more than 6 months after Tx; except for liver – Generally irreversible except for liver – Staging is important to help approach further therapy Antibody-Mediated Rejection • Antibodies may be preformed or develop after transplantation – Anti-endothelial cells most deleterious (ABO, lymphocytotoxic) – Susceptibility = kidney > heart > intestine > lung > liver – Increased risk in multiparous women, previous blood, or tissue exposure • Recognized histopathologically as microvascular endothelial “activation”, leukocyte margination, injury and congestion, lymphocytic and necrotizing arteritis • Definitive diagnosis usually requires clinical dysfunction, typical histopathologic changes and evidence of antibody-mediate injury and circulating anti-donor antibodies. Acute “Cellular” or T Cell Mediated Rejection • Mediated primarily by inflammatory cells – T lymphocytes, macrophages, B cells, eosinophils, and neutrophils • Most active period is during the first 6 months after Tx unless Ab-depletion therapy used – Later episodes: • inadequate immunosuppression • Immune reconstitution • Grading Used to Help Guide Therapeutic Intervention – Indeterminate/minimal/borderline, mild, moderate, and severe Basis for Histopathologic Grading of Acute Rejection • Severity and Distribution of Inflammation – Localized or diffuse – Estimate of amount of tissue injury • Direct or Indirect Evidence of Microvascular or Arterial Injury and Ischemia – Inflammatory or necrotizing arteritis – Interstitial hemorrhage w/o necrosis – Confluent necrosis Chronic Rejection Risk Factors • Immune Factors – Primary – Number and severity of acute cellular and AMR episodes – Matching • MHC, Sex, Race – Infections • CMV, Polyoma virus, bronchiolitis • “Non-immune” - Secondary – older donors, cold ischemia, donor atherosclerosis, inadequate functional capacity Major Problem in Transplantation Immune graft damage Fibrosis Chronic Rejection DM, ↑BP, Renal failure Opport. Infections Tumors CPC Conferences Keep Amplitude of Drift Low Rejection Rejection Infection Infection Special Procedures Needed • Specialized stains used for native kidney, liver, lung, pancreas, and small intestinal biopsies • IPEX or IF staining for IgGs and C (esp. C4d) • IPEX staining and/or ISH for viruses that commonly affect allograft recipients: – BK/Polyoma, EBV, CMV, HSV, VZ, Adenovirus, HHV-6, HBV, • Genetic analysis for origin of tissue: – XY ISH, specific anti MHC Abs, genetic identity testing • Electron Microscopy: F/U of renal allograft biopsies Use of Gene Arrays in Transplantation Purvesh Khatria and Minnie M. Sarwal Current Opinion in Organ Transplantation 2009, 14:34–39 • The current standard in allograft dysfunction diagnosis is histopathology, which is subjective, non-quantitative, and does not offer any insights into rejection mechanisms. On the contrary, gene expression profiling using microarray can provide objective, quantitative gene expression, which in turn can provide mechanistic insights into pathogenesis of transplant rejection. Limitations of Microarrays • Loss of spatial and temporal relationships • Deconvoluting gene signatures – Effects of multiple conflicting factors • Age, sex, medications, circumstances of biopsy • Expensive and requires time to complete • Post translational events not included • Multiple gene assays limits dynamic range of MA compared to real time PCR • Overwhelming amount of data generated on infinite variations Reporting on Allograft Biopsies • Final diagnosis should be based on extensive clinicopathologic correlation • More than one insult can contribute to the injury and diagnostic hierarchy should be assigned, if possible. • Provide Value in Your Report! • Liver Allograft, Needle Biopsy: – Negative for acute cellular and chronic rejection (RAI = 0/9). – Chronic hepatitis, recurrent HCV, mildly active (mHAI = 6/18). – Mild to moderate portal/periportal fibrosis (Fibrosis stage = 2/6). – Compared to the previous biopsy of 01/01/2009 the current biopsy shows increased fibrosis and architectural distortion. Conclusions • Antigen migration/lymphoid trafficking early after transplantation important concept • Working knowledge of immunologic events and mechanisms greatly assists clinical practice and research • Final interpretation should be based on complete clinicopathologic correlation • Specialized staining procedures needed for complete specimen evaluation • Reporting should be complete, hierarchical, if needed, and answer clinical questions/concerns