* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Moderate depressive episode
Narcissistic personality disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Bipolar disorder wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Parkinson's disease wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
History of psychiatry wikipedia , lookup
Child psychopathology wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
History of mental disorders wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Conversion disorder wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
Mental status examination wikipedia , lookup
Postpartum depression wikipedia , lookup
Biology of depression wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Behavioral theories of depression wikipedia , lookup
Evolutionary approaches to depression wikipedia , lookup
Abnormal psychology wikipedia , lookup
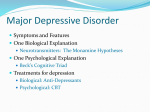
Malaysian CPG on the Management of Major Depressive Disorder Major depressive disorder: prevalence Lifetime prevalence from community surveys: 5% to 17% (Kessler 1994, AHCPR 1993) Six- to 12-month prevalence estimates: 2-11%, weighted mean 6% (Andrade et al. 2003; Robins and Regier 1991) Burden of disease By year 2020 major depression projected to be 2nd largest contributor to global burden of disease, after heart disease (Murray & Lopez, 1997) By 2030, the leading cause of DALYs worldwide is projected to be unipolar depressive disorders, followed by ischaemic heart disease and road traffic accidents (WHO 2008) Risk for suicide associated with depressive disorders elevated 12- to 20-fold compared to general population (Harris & Barraclough 1997) Malaysian Burden of Disease and Injury Study 2004: – Mental disorders contributed 8.6% of total DALYs, ranking as the 4th leading cause of disease burden – Unipolar major depression accounted for 45% of total burden due to mental disorders Causes of DALYs, Malaysia 2000 (Malaysian Burden of Disease & Injury Study 2004) Males: unipolar major depression was 9th leading cause (3% of 111 diseases) Females: unipolar major depression was 3rd leading cause (5% of 111 diseases) Leading causes of YLDs in 2004 (WHO 2008) Unipolar depressive disorder ranked first, for both males and females – Males: 8.3% of total YLDs – Females: 13.4% of total YLDs NB: YLD = years lived with disability Hidden morbidity Patients often delay seeking professional treatment for depression (Olfson et al 1998) Surveys in 6 Western European countries found that only 36.6% of those with active depression in the last 1 year received any professional treatment during the subsequent year (ESEMeD/MHEDEA 2000 Investigators 2004) Roles of healthcare providers Level People responsible Level 1 Primary care Assistant medical officer Nurses Medical Officer Level 2 Primary Care Family Medicine Specialist Medical Officer Level 3 Primary Care Family Medicine Specialist Focus of Disease Action Recognition Screening Mild Depressive Episode Psychological Intervention(counselling , problem solving and supportive psychotherapy) ± Medication Moderate Depressive Episode Medication Psychological Intervention Referral to secondary care if indicated including for cognitive behaviour therapy (CBT) Level People responsible Level 4 Secondary Care Outpatient psychiatric services Level 5 Secondary Care In-patient setting Focus of Disease Action Moderate to Severe Episode Medication Psychological intervention including CBT Risk to self/others Severe self neglect Psychotic symptoms Lack of impulse control Medication Psychological intervention including CBT ECT Assessment & Diagnosis Screening for depression Two-question Case Finding Instrument Evaluate for depression if “Yes” to either question Sensitivity 96%, specificity 57% PPV 33%, NPV 98% (at prevalence of 18%) (Whooley et al 1997) At estimated local prevalence of 5.6% PPV = 12% NPV = 99.6% ICD-10 criteria Typical symptoms of depressive episodes Depressed mood Loss of interest & enjoyment Reduced energy ICD-10 criteria Common symptoms of depressive episodes Reduced concentration & attention Reduced self-esteem & self – confidence Ideas of guilt & unworthiness Bleak & pessimistic views of the future Ideas or acts of self-harm or suicide Disturbed sleep Diminished appetite ICD-10 criteria contd.. Mild Depressive Episode At least 2 typical symptoms + 2 common symptoms No symptom should be present to an intense degree Minimum duration of whole episode is at least 2 weeks The person has some difficulty in continuing ordinary work & activities ICD-10 criteria contd.. Moderate depressive episode At least 2 typical symptoms + 3 common symptoms Some symptoms may be present to a marked degree Minimum duration of whole episode is at least 2 weeks The person has considerable difficulty in continuing social, work or domestic activities ICD-10 contd..episode Severecriteria depressive without psychotic symptoms All 3 typical symptoms + at least 4 common symptoms Some of the symptoms are of severe intensity Minimum duration of whole episode is at least 2 weeks ( may be <2 weeks if symptoms are very severe & of very rapid onset. The person is very unlikely to continue with social, work or domestic activities ICD-10 criteria contd.. Severe depressive episode with psychotic symptoms A severe depressive episode Delusions, hallucinations or depressive stupor are present Referral to Psychiatric Services Unsure of diagnosis Attempted suicide Active suicidal ideas/plans Failure to respond to treatment Advice on further treatment Clinical deterioration Recurrent episode within 1 year Psychotic symptoms Severe agitation Self neglect Common criteria for psychiatric admission include: Risk of harm to self Psychotic symptoms Inability to care for self Lack of impulse control Danger to others Psychological interventions Counselling A systematic process which gives individuals an opportunity to explore, discover and clarify ways of living more resourcefully, with a greater sense of well-being. (British Association for Counselling and Psychotherapy) Concerned with addressing and resolving specific problems, making decisions, coping with crises, working through conflict or improving relationships with others. Problem solving therapy • • Time-limited, structured intervention that focuses on learning to cope with specific problem areas. Therapist and patient work collaboratively. Supportive therapy Any form of treatment intended to relieve symptoms or help the patient live with them rather than attempt changes character structure. Components of supportive therapy Reassurance Explanation Guidance Suggestion Encouragement Effecting changes in patient’s environment Allowing catharsis Cognitive Behaviour Therapy Basic idea is that it is not events that distress us, but what we think about them CBT helps patients become aware of their own thoughts and replace them with more realistic thoughts Computerised cognitivebehaviour therapy (CCBT) • The delivering of CBT via an interactive computer interface. It may be used for mild to moderate depression. • Examples of programmes available over the internet: – – – – Moodgym Beating the Blues (BtB) COPE Overcoming depression Psychodynamic psychotherapy Patient explores feelings, and conscious and unconscious conflicts originating in the past, and gains insight. Should be reserved for selected patients, e.g. those with complex comorbidities, personality problems, traumatized persons and those with comorbid anxiety disorders. Interpersonal therapy A time-limited , structured psychological intervention that focuses on interpersonal issues. Therapist and patient work to identify the effects of problems related to: – interpersonal conflicts – role transitions – grief and loss – social skills PHARMACOTHERAPY Phases of pharmacotherapy Acute Phase A period where remission is achieved. Continuation Phase A period after sustained and complete remission from the acute phase. Usually a period of 6-9 months. Maintenance Phase A period to prevent recurrence (a new episode of depression) and to prevent the development of chronicity. Acute phase pharmacotherapy Mild depressive episode May exercise the option of treating by non-pharmacological means alone, viz. problem-solving, counselling, and supportive therapy, and exercise as an adjunct. Close follow-up appointment (within 2 weeks) so that patient’s condition can be monitored closely. Consider antidepressant medication: If depression persists or worsens If patient had a past history of moderate to severe depression, and now presents with a mild depressive episode When the patient is experiencing ongoing stressors that may perpetuate or worsen the depression Moderate-severe depressive episode Offer antidepressants Drug of first choice is an SSRI – Fluoxetine – Fluvoxamine – Sertraline – Escitalopram – Paroxetine – Citalopram Role of benzodiazepines Failed response to initial treatment Patients who have not responded after 4 weeks of antidepressant therapy at an adequate dose are acute phase nonresponders. Apparent non-response This may be due to: – incorrect diagnosis – psychotic depression – organic conditions – co-morbid psychiatric disorder – adverse psychosocial factors – non/poor compliance Apparent non-response If these other causes of apparent nonresponse have been ruled out, the further strategies to follow are: – Optimisation – Switching Optimisation If there are no significant side effects, increase the dose of medication gradually until – response is achieved – or to the maximum dose that can be tolerated – or until the maximum allowable dose is achieved Switching This refers to a change of antidepressant. You may switch within the same class of antidepressant (i.e. SSRI) or to another class. Reduce the dose of the first antidepressant gradually and slowly titrate upwards the dose of the new antidepressant. Treatment-resistant depression Depression that has failed to respond to two or more antidepressants given sequentially at an adequate dose for an adequate duration of time. Adequate dose is at least 150 mg/day imipramine equivalent Adequate duration refers to at least 4 weeks. Continuation phase pharmacotherapy After remission is achieved, continue antidepressants for another 6-9 months Use the same dose as for the acute phase Maintenance phase pharmacotherapy Not all patients will need to go on to the maintenance phase pharmacotherapy Maintenance phase treatment should be considered for the following: – 3 or more episodes of depression – 2 episodes with severe functional impairment Maintenance phase pharmacotherapy contd... – 2 episodes of depression, plus one or more of the following: –family history of bipolar disorder –history of recurrence within 1 year after discontinuation of medication –family history of recurrent major depression –early onset (< age 20) of first depressive episode Maintenance phase pharmacotherapy contd... –depressive episodes were severe, sudden, or life threatening within the past 3 years – Residual symptoms – Co-morbid dysthymic disorder, substance abuse or anxiety disorders (Bauer et al 2002, AHCPR 1993) Discontinuation of medication Drug therapy should not be terminated abruptly The medication should be tapered down gradually over weeks and sometimes even months Electroconvulsive therapy Effective and rapid form of somatic treatment for major depressive disorder Indications: – High degree of symptom severity and functional impairment – Psychotic symptoms – Catatonic features – Urgent response needed/life-threatening condition OTHER THERAPIES Exercise Therapy Structured and supervised exercise activity 40-60 minutes per session, up to 3 times per week and prescribed for 10-12 weeks has been shown to be effective. For practical purposes at least 30 minutes of daily moderate aerobic exercise is recommended. Social rhythm/ lifestyle Rhythm and regularity of activities are important for mental health Interaction with significant others reduces isolation Schedule activities (rest and recreation) that involve others Proper diet and exercise are helpful Maintain regular sleeping hours Guideline implementation priorities Training module – Manual – PowerPoint presentations – Video vignettes Quick reference for healthcare providers Patient information leaflet Note: these slides are a distillation of the information contained in the CPG, with some additional material on burden of disease.