* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Cardiovascular System
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
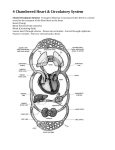
Provides oxygen and nutrients to tissues Removes wastes FYI Pumps 7,000 liter per day Beats 2.5 Billion times in your lifetime Hollow, cone-shaped Lies within thoracic cavity Rests on diaphragm Average Size 14cm long and 9cm wide Enclosed by layered pericardium Visceral – inner layer Parietal – outer layer Pericardial Cavity Space between the parietal and visceral layers of the pericardium Pericarditis Inflammation of pericardium Adhesions cause layers of pericardium to attach to each other Very painful Interferes with heart movements Epicardium Outer layer Visceral pericardium Protects heart reduces friction Myocardium Middle layer Pumps blood out of heart chambers Endocardium Inner layer Two atria Upper chambers Receive blood returning to heart Two ventricles Lower chambers Receive blood from atria Contract to force blood out of heart Right atrium receives blood from inferior vena cava, superior vena cava and coronary sinus Tricuspid valve Separates right atrium from right ventricle Prevents back flow when ventricle contracts Chordae Tendineae Right Ventricle Pumps blood to lungs Thin walls Pulmonary Valve Sends blood through pulmonary arteries to lungs Left Atrium Receives blood from lungs Arrives through pulmonary veins Mitral Valve Biscuspid valve Left Ventricle Aorta Aortic valve Fibrous rings enclose base of pulmonary artery and aorta Attachments for heart valves and muscle fibers Prevent chambers from dilating during contraction Blood Supply Coronary arteries First two branches of aorta Supply blood to myocardium Returns through cardiac veins and coronary sinus Mitral Valve Prolapse Blood gets back into atrium during ventricular contraction Chest pain, palpitations, fatigue and anxiety Often caused by Streptococcus bacteria Angina Pectoris Narrowing of coronary arteries Deprives heart cells of oxygen Heavy pressure, tightening or squeezing of chest Myocardial Infarction Heart attack Blood clot obstructs artery and kills part of heart Cardiac Cycle Atria contract (systole) while ventricles relax (diastole) Ventricles contract while atria relax Both relax for brief interval Due to vibrations the valve movements produce Lubb-Dubb Lubb Ventricular contractions A-V valves closing Dubb Ventricular Relaxation Pulmonary and Aortic valves closing Edges of valves erode away and don’t close completely Blood leaks back through the valve Can be caused by endocarditis (inflammation of endocardium) Repaired through open heart surgery Functional Syncytium Mass of merging cells that function as a unit We have atrial syncytium and ventricular syncytium If any part of the syncytium is stimulated, the whole structure contracts as a unit Initiates and conducts impulses throughout the myocardium Begins in Sinoatrial Node (S-A Node) Located under right atrium Fibers continuous with atrial syncytium Cells reach threshold on their own Membranes contract Rhythmic 70-80 times/minute Pacemaker Impulse travels from S-A Node to atrial syncytium Right and left atria contract Impulse goes to Atrioventricular Node (A-V Node) by way of junctional fibers Impulse enters A-V bundle This bundle gives way to Purkinje Fibers Gives way to twisting contraction of ventricles Records electrical changes in myocardium during a cardiac cycle Body fluids conduct electrical currents P wave Atrial depolarization QRS Complex Ventricular depolarization T wave Ventricular repolarization Parasympathetic Fibers Braking Action Nerve impulse reach fiber endings and secrete acteylcholine Decreases S-A and A-V node activity Increase in impulses – decreased heartrate Decrease in impulses – increased heartrate Sympathetic Fibers Secrete norepinephrine Increases rate and force of myocardial contractions Cardiac Center Located in Medulla Oblongata Keeps balance between sympathetic and parasympathetic impulses Baroreceptors control blood pressure – rising pressure lowers heart rate – lowers blood pressure Fainting – decreases heart rate Anxiety – increases heart rate Temperature – increase in temp increases heart rate Potassium – too much decreases rate and force of contractions Calcium – too much increases heart actions Closed circuit of tubes that carry blood from heart to cells and back Include arteries, arterioles, capillaries, venules and veins Human body has 62,000 miles Can circle globe 2 ½ times Arteries Strong, elastic vessels Adapted to carry blood at high pressure Branch and subdivide into arterioles Made of 3 layers Tunica interna Tunica media Tunica externa Vasoconstriction – arteries contract – get smaller Vasodilation – arteries relax – get larger These two functions influence blood flow and blood pressure Connect arterioles and venules Wall is single layer of cells that forms a semipermeable membrane Gas, nutrient and waste exchange occurs here Openings in walls vary from tissue to tissue Smaller in muscles Larger in endocrine glands, kidneys and small intestines Density varies with cellular needs Muscle and nerves have high need for nutrients – so they have many capillaries Cartilage, epidermis and cornea – no need – no capillaries Precapillary Sphincters Regulate blood flow During exercise muscle cells have most need so they get the most blood- digestive system capillaries close because they aren’t really working at that time Capillary blood and tissue fluid exchange gases, nutrients, and metabolic by-products Diffusion provides the most important means of transport Filtration, which is due to hydrostatic pressure of blood, causes a net outward movement of fluid at the arteriorlar end of a capillary Osmosis due to colloid osmotic pressure causes a net inward movement of fluid at the venular end Venules Microscopic vessels that continue from capillary and merge to form veins Veins Carry blood back to heart Made of three layers but middle layer is weak Don’t have to be as strong because blood pressure is lower Have valves to keep blood moving in right direction Serve as reservoirs Up to 25% of blood here Blood pressure is the force blood exerts against the insides of blood vessels Rises and falls with phases of cardiac cycle Systolic pressure Ventricle contracts Top number – should be <120 Diastolic pressure Ventricle relaxes Bottom number – should be <80 Heart Action Stroke volume – amount discharged with each contraction – 70ml for average male at rest Cardiac Output – volume discharged per minute If these number go up – so does blood pressure Blood Volume Approximately 5 liters (8% of body weight) More blood – higher blood pressure Peripheral Resistance Friction between blood and walls of blood vessels More friction – higher blood pressure Plaque build-up in arteries Blood Viscosity Thicker blood – higher blood pressure Controlled by the mechanisms that regulate cardiac output and peripheral resistance More blood enters heart stronger contraction greater stroke volume and greater cardiac output Little pressure left after blood moves through arteries, arterioles and capillaries Depends on Skeletal muscle contractions – when muscles contract blood in veins gets pushed from one valve reservoir to the next Respiratory movements – when rib cage expands applies pressure on abdominal veins and blood gets pushed from abdominal veins into thoracic veins Venoconstriction – if blood is lost veins contract, empty reservoirs and push blood back to heart. Pulmonary Circuit Consists of vessels that carry blood from the right ventricle to the lungs and back to the left atrium Systemic Circuit Consists of vessels that lead from the heart to the body cells (including the heart itself) and back to the heart Includes the aorta and its branches