* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 6. Heart failure
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Rheumatic fever wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Heart failure wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
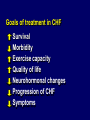
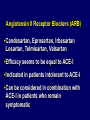
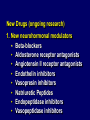
CHRONIC HEART FAILURE Heart Failure • What is Heart Failure? Basic Definition • Heart failure is a medical term that describes an inability of the heart to keep up its work load of pumping blood to the lungs and to the rest of the body. http://danilhammoudimd_1.tripod.com/cardio1/id57.htm Statistic • It is estimated that as many as two million Americans suffer from congestive heart failure and that up to 29, 000 die annually from this chronic disorder. » Cannobio, Mary. Cardiovascular Disorders. Missouri: C.V. Mosby Company, 1990. Symptoms (involving gravity/exhaustion of heart • Swelling of the ankles, legs, and hands • Orthopnea, or the shortness of breath when lying flat • Shortness of breath during exertion Symptoms (involving circulation) • Cyanosis, or a bluish color that is seen in the lips and fingernails from a lack of oxygen • Fatigue or weakness • Rapid or irregular heart beat • Changes of behavior such as restlessness, confusion, and decreased attention span Symptoms (involving congestion) • • • • • Unexplained or unintentional weight gain Chronic cough Increased urination Distended neck veins Loss of appetite or indigestion Congestive heart failure is a syndrome that can be caused by multiple underlying diseases such as: • Congenital heart disease • Atherosclerosis • Rheumatic fever • Cardiomyopathy • Valve disorders • Ventricular failure • Left or right-sided failure • Hypertension • Prolonged alcohol or drug addiction • Previous heart attack • Diabetes • Chronic rapid heartbeats Congenital Heart Disease • CHD affects one out of every one thousand babies. In these babies the marvelously intricate combination of chambers, valves, and vessels making up the heart and circulatory systems fails to form properly before birth. Septal, atrial, and ventricular defects are the most common. “Heart.” The World Book Encyclopedia. 1996 ed. Rheumatic Fever • Strep throat from the streptococcal infection begins a disease process where the heart valves are damaged. This condition is called rheumatic fever and it affects the connective tissues of the body. Cardiomyopathy • Cardiomyopathy is the stretching and enlarging of the heart cavity that occurs making the heart weak so it does not pump correctly Ventricular Failure • Ventricular failure occurs when there are weak spots in the ventricular walls causing a bulge, or an aneurysm. Atherosclerosis • Atherosclerosis is the gradual clogging of the arteries by fatty, fibrous deposits. A tiny lump of fibrous tissue grows as the artery tries to repair the damage. Cholesterol accumulates and more tissue builds up. The arteries are thickened and hardened making a loss of elasticity causing congestion. http://danilhammoudimd_1.tripod.com/cardio1/id57.htm c1183higgin05[1]video2.mpeg KEY ISSUES IN CHRONIC HEART FAILURE • Common 1-3 % of the population, rising to 6-10 % of people aged >65 years Incidence x2 in the last 10 years Dangerous – high mortality (>50% over 5 yrs, 50% of these deaths occur suddenly) Disabling – high morbidity (on average, 1 in 5 patients is readmitted within 12 months) Costly – 1.5-2.5% of health care budget Contributors to Increased Incidence - Improvements in: - Survival post-MI - Technologies (i.e.. Laser, stents etc.) - Medical Treatments for ischemic heart disease - Overall survival DEFINITION OF HEART FAILURE Clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood AHA / ACC HF guidelines 2001 Clinical symptoms / signs secondary to abnormal ventricular function ESC HF guidelines 2001 DEFINITION OF HEART FAILURE I. Symptoms of heart failure, typically breathlessness or fatigue, either at rest or during exercise, or ankle swelling II. Objective evidence (preferably by echocardiography) of cardiac dysfunction (systolic and/or diastolic) at rest III. Response to treatment directed towards heart failure Criteria I. and II. should be fulfilled in all cases ESC HF guidelines 2005 Q’s to be answered while facing a patient with suspected heart failure 1. Are the patient’s symptoms cardiac in origin? 2. If so, what kind of cardiac disease is producing these symptoms HEART FAILURE should never be the only diagnosis ! Etiology of Chronic Heart Failure Coronary artery disease accounts for about 65% Non-ischemic Cardiomyopathy: Hypertension Valvular Heart Disease Idiopathic Thyroid Toxic or drug-induced SYMPTOMS I. There is a poor relationship between symptoms and the severity of cardiac dysfunction. Mild symptoms should not be equated with minor cardiac dysfunction II. Symptoms may be related to prognosis particularly if persisting after therapy III. Once a diagnosis of heart failure has been established, symptoms may be used to classify the severity of heart failure and should be used to monitor the effects of therapy Electrocardiogram • A normal electrocardiogram (ECG) suggests that the diagnosis of CHF should be carefully reviewed • The presence of pathological Q-waves may suggest myocardial infarction as the cause of cardiac dysfunction. • A QRS width >120 ms suggests that cardiac dyssynchrony may be present and a target for treatment Types of Rhythms Associated with CHF – Left Ventricular Failure with Pulmonary Edema • Aka—systolic heart failure – Right Ventricular Failure • Aka—diastolic heart failure The smooth, glistening pleural surface of a lung is shown here. This patient had marked pulmonary edema, which increased the fluid in the lymphatics that run between lung lobules. Thus, the lung lobules are outlined in white. – Occurs when the left ventricle fails as an effective forward pump – back pressure of blood into the pulmonary circulation – pulmonary edema – Cannot eject all of the blood delivered from the right heart. – Left atrial pressure rises increased pressure in the pulmonary veins and capillaries – When pressure becomes to high, the fluid portion of the blood is forced into the alveoli. – decreased oxygenation capacity of the lungs – AMI common with LVF, suspect – Severe resp. distress– • Evidenced by orthopnea, dyspnea • Hx of paroxysmal nocturnal dyspnea. – Severe apprehension, agitation, confusion— • Resulting from hypoxia • Feels like he/she is smothering – Diaphoresis— • Results from sympathetic stimulation – Pulmonary congestion • Often present • Rales—especially at the bases. • Rhonchi—associated with fluid in the larger airways indicative of severe failure • Wheezes—response to airway spasm – Jugular Venous Distention—not directly related to LVF. • Comes from back pressure building from right heart into venous circulation – Vital Signs— • Significant increase in sympathetic discharge to compensate. • BP—elevated • Pulse rate—elevated to compensate for decreased stroke volume. • Respirations—rapid and labored ECHOCARDIOGRAPHY • • Assessment of LV systolic function (EF) Assessment of LV diastolic function Natriuretic peptides • Plasma concentrations of BNP and NT-proBNP are helpful in the diagnosis in HF • A low-normal concentration in an untreated patient makes HF unlikely as the cause of symptoms • BNP and NT-proBNP have considerable prognostic potential. Their role in treatment monitoring remains to be determined The value of BNP in HF diagnosis A. Is well established in the general population B. Is well established in persons at risk of heart failure C. Is well established in patients with suggestive symptoms D. Has an overall accuracy of 100% E. Is based on a high negative predictive value The value of BNP in HF diagnosis A. Is well established in the general population B. Is well established in persons at risk of heart failure C. Is well established in patients with suggestive symptoms D. Has an overall accuracy of 100% E. Is based on a high negative predictive value NYHA classification of HF Class I No limitation: ordinary physical exercise does not cause undue fatigue, dyspnea, or palpitations Class II Slight limitation of physical activity: comfortable at rest but ordinary activity results in fatigue, palpitations, or dyspnea Class III Marked limitation of physical activity: comfortable at rest but less than ordinary activity results in symptoms Class IV Unable to carry out any physical activity without discomfort: symptoms of heart failure are present even at rest with increased discomfort with any physical activity Hypertension Diabetes, Hyperchol. Family Hx Cardiotoxins A Heart disease (any) B Stages in the Evolution of Heart Failure Clinical Characteristics Asymptomatic LV dysfunction Systolic / Diastolic C Dyspnea, Fatigue Reduced exercise tolerance D Marked symptoms at rest despite max. therapy Treat risk factors Avoid toxics ACE-i in selected p. A ACE-i blockers B Stages in the Evolution of Heart Failure Treatment In selected patients C ACE-i blockers Diuretics / Digitalis D Palliative therapy Mech. Assist device Heart Transplant Goals of treatment in CHF Survival Morbidity Exercise capacity Quality of life Neurohormonal changes Progression of CHF Symptoms Prolong survival •ACE inhibitors •Beta blockers •Spironolactone •Angiotensin receptor blockers •Implantable cardioverter-defibrillators Symptom reduction and improved activity tolerance •Exercise training •Diuretics •ACE inhibitors •Digoxin •Beta blockers Prevent progression (remodeling) •ACE inhibitors •Beta blockers •Spironolactone •Angiotensin receptor blockers •Cardiac resynchronization (biventricular pacing) Non-pharmacological management • Sodium and fluid restriction • Alcohol • Weight • Smoking • Rest and exercise Dietary advice • 2-2.5 g sodium restriction (about 5-6 g of salt) • Fluid restriction (in patients with refractory fluid retention, significant hyponatremia or severely impaired renal function • Low fat diet and caloric restriction when indicated • Abstention from alcohol or restriction to 1 drink per day Activity and exercise councelling • Encourage regular activity in all patients • Exercise training/cardiac rehabilitation in stable, motivated patients Activity and exercise councelling Symptomatic and psychologic benefits: • Aerobic training results in increased exercise capacity (peak oxygen consumption), improved quality of life (questionnaires), reduced sympathetic nervous system activity • Possible beneficial effect on prognosis Treatment Pharmacologic Therapy • Diuretics • ACE inhibitors • Beta Blockers • Digitalis • Spironolactone • Other Approach to the patient with HF Assess LV function (EF < 40%) Assess volume status Fluid retention? Yes No Diuretic ACE inhibitor Digoxin Beta-blocker Digitalis. Indications • When no adequate response to ACE-i + diuretics + beta-blockers AHA / ACC Guidelines 2001 • AF, to slow AV conduction Dose 0.125 to 0.250 mg / day Spironolactone. Indications • Recent or current symptoms despite ACE-i, diuretics, dig. and -blockers AHA / ACC HF guidelines 2001 • Recommended in advanced heart failure (III-IV), in addition to ACE-i and diuretics • Hypokalemia ESC HF guidelines 2001 Angiotensin II Receptor Blockers (ARB) • Candesartan, Eprosartan, Irbesartan Losartan, Telmisartan, Valsartan • Efficacy seems to be equal to ACE-I • Indicated in patients intolerant to ACE-I • Can be considered in combination with ACE-I in patients who remain symptomatic Nitrates. Clinical Use • CHF with myocardial ischemia • Orthopnea and paroxysmal nocturnal dyspnea • In acute CHF and pulmonary edema:NTG sl / iv • Nitrates + Hydralazine in intolerance to ACE-I (hypotension, renal insufficiency) Positive Inotropic Therapy •May increase mortality Exception: Digoxin, Levosimendan •Use only in refractory CHF •NOT for use as chronic therapy Drugs to Avoid (may increase symptoms, mortality) • Inotropes, long term / intermittent • Antiarrhythmics (except amiodarone) • Calcium antagonists (except amlodipine) • Non-steroidal antiinflammatory drugs (NSAIDS) • Tricyclic antidepressants • Corticosteroids • Lithium ESC HF guidelines 2001 New Drugs (ongoing research) 1. New neurohormonal modulators • Beta-blockers • Aldosterone receptor antagonists • Angiotensin II receptor antagonists • Endothelin inhibitors • Vasopresin inhibitors • Natriuretic Peptides • Endopeptidase inhibitors • Vasopeptidase inhibitors Diastolic Heart Failure • Treat as HF with low LVEF • Control: • Hypertension • Tachycardia • Fluid retention • Myocardial ischemia • Ongoing research ICD • Implantation of an ICD in combination with biventricular pacing may be considered in patients who remain symptomatic with severe heart failure NYHA class III-IV with LVEF≤35% and QRS duration ≥ 120 msec • ICD therapy is recommended to improve survival in patients after cardiac arrest or who have sustained ventricular tachycardia Heart Transplant. Indications • Refractory cardiogenic shock • Documented dependence on IV inotropic support to maintain adequate organ perfusion • Peak VO2 < 10 ml / kg / min • Severe symptoms of ischemia not amenable to revascularization • Recurrent symptomatic ventricular arrhythmias refractory to all therapeutic modalities Contraindications: age, severe comorbidity Thank you for attention!