* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Evolution of ICD Therapy:
Survey
Document related concepts
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
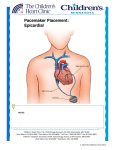
Single Chamber Temporary Pacing Operations & Troubleshooting Temporary Pacing Indications Sick Sinus Syndrome (Patient Must Be Symptomatic and Documented with ECG) Symptomatic sinus bradycardia Symptomatic sinus arrest Suppression of ventricular ectopy resulting from bradycardia Atrial fibrillation Bradycardia/Tachycardia syndrome Temporary Pacing Indications Heart Blocks Type I and Type II second degree AV block Acute bifascicular or trifascicular block Complete AV block Cardiac arrest with ventricular asystole Other Temporary Pacing Indications Drug-Refractory Dysrhythmia Overdrive ventricular pacing to suppress or prevent VEA (Ventricular Ectopic Activity) Overdrive atrial pacing to “break” SVT, atrial flutter Other Temporary Pacing Indications Cardiovascular Surgery Coverage for anesthesia and surgery in patients with positive cardiac history Treatment for CHB development during surgery Augment cardiac output post operatively Other Temporary Pacing Indications Diagnostic Uses SSS pacing studies to determine SA node recovery Stress testing for Coronary Artery Disease Electrophysiologic (EP) studies Insertion Sites Internal Jugular Vein External Jugular Vein Brachial Vein Femoral Vein Subclavian Vein Lead Types Lead Types Endocardial/Transvenous lead – Transvenous lead is introduced into a vein and advanced into the heart Epicardial/Myocardial lead – An epicardial lead attached to the outside of the heart is introduced through the chest wall Lead Types Bipolar lead system – The negative and positive electrodes are in contact with the heart Lead Types Unipolar lead system – The negative electrode is in contact with the heart and the positive (or ground) electrode is located elsewhere on the body Cable Connectors Connector pins on the lead(s) must be fully inserted in the patient connector block Observe polarity – Distal = negative – Proximal = positive Finger tighten only – no tools! Temporary Pacing Parameters Pacing rate (heart rate) Output/stimulation threshold Sensitivity Pacing Rate Paced Interval Paced Interval Output Output Pulse Output/Current (ma) Pulse Width (ms) The output dial regulates the current or movement of electrons Capture Depolarization of cardiac muscle following an electrical stimulus Stimulation Threshold The minimum output pulse needed to consistently capture the heart 3 mA 2 mA 1 mA Lead Maturation Threshold Amplitude x3 x2 Initial 1 2 3 4 5 10 Days Since Leads Applied 15 Sensitivity The degree that the pacing system “sees” or senses signals, controlled by the sensitivity setting which is graduated in millivolts (mV) Sensitivity (mV) 5 (mV) 2.5 (mV) 1.25 (mV) Sensitivity The lower the setting, the more sensitive the pacemaker is to intracardial signals NBG Codes 1st Letter 2nd Letter Chamber(s) Paced A = atrium V = ventricle D = dual (both atrium and ventricle) Chamber(s) Sensed A = atrium V = ventricle D = dual O = none 3rd Letter Response to Sensing I = inhibit (Demand mode) T = triggered D = dual O = none (Asynch) Chamber paced Chamber sensed Action or response to a sensed event V V I VVI Demand/Inhibited Pacemaker senses intrinsic depolarization Paces the heart when the patient’s own rate becomes slower than the pacemaker Ventricular Inhibited Mode (VVI) VOO Asynchronous (Fixed) Pacemaker will emit an output at a fixed rate regardless of intrinsic activity Ventricular Asynchronous Mode (VOO) Single Chamber Troubleshooting Process 1. Gather information 2. Identify the problem and possible cause 3. Identify the solution and carry out corrective procedures Information Gathered Patient data Pacemaker information Lead information Non-invasive tools Undersensing Failure of the pacemaker to sense intrinsic R-waves or intrinsic P-waves Undersensing Oversensing Inhibition of the pacemaker by events the pacemaker should ignore, e.g. EMI, T-waves, and myopotential Oversensing Loss of Capture Loss of Output Fusion/Pseudofusion Beats Intrinsic Beat Intrinsic Beat Fusion Beat Fusion Beat Paced Beat Paced Beat Pseudofusion Beat Pseudofusion Beat Electromagnetic Interference (EMI) Radiated or conducted energy – either electrical or magnetic – which can interfere with the function of the pacemaker in the Demand mode (EMI) Should have paced 2.5 mV 80 80