* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Basics of Pacing - St. Joseph Mercy Health System
Heart failure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
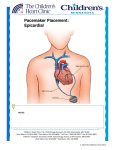
Basics of Pacing Ruth Hickling, RN-BSN Tasha Conley, RN-BSN The Cardiac Conduction System Cardiac Conduction System Review Normal Conduction Conduction QRS QRS Complex Complex RR PP ST ST segment segment PR PR segment segment PR Interval PR Interval Q Q ST interval ST interval SS QT Interval QT Interval TT Indications for Pacing Documented evidence of Arrhythmia and Symptoms Symptomatic Bradycardia Sick Sinus Syndrome (AKA tachy/brady) Sinus Arrest or Sinoatrial (SA) Exit Block Atrial Fibrillation with slow V response or s/p AVNA for AF with RVR • Atrioventricular Block • First Degree (symptomatic) • Second Degree, Mobitz I and II • Third Degree or Complete Heart Block • Carotid Sinus Hypersensitivity/Syncope • • • • Possible Symptoms Syncope Dizziness Confusion Fatigue Shortness of Breath Limited Exercise Tolerance Keeping it Simple If the Sinus Node Doesn’t Fire… … then we need to pace the atrium Keeping it Simple If the AV node does not appropriately conduct… ...then we need to pace the ventricle In a ‘Nut Shell’ Pacemakers 1. Keep the heart from going too slow 2. Provide AV Synchrony 3. Aid in Chronotropic response Indications for ICD Implantation Primary Prevention • Congenital Heart Disease • Long QT Syndrome • Cardiomyopathy that meets appropriate NYHE guidelines Ischemic Non-Ischemic Idiopathic Hypertrophic Secondary Prevention • Prior Cardiac Arrest • Ventricular Tachycardia • Ventricular Fibrillation What makes up a Pacemaker / AICD System? Basic Components of Pacing/AICD System • Pulse Generator • • • • Battery Circuitry Case Header • Lead(s) • Systems can have up to three leads depending on implant indication Pacemaker Components of a pacemaker pulse generator. Also called “the Can” “Brain” Single-Chamber System • The pacing lead is implanted in the atrium or ventricle, depending on the chamber to be paced and sensed Dual Chamber Systems Have Two Leads • One in the atrium • One in the ventricle Biventricular Pacing Systems Also called Cardiac Resynchronization Therapy (CRT) pacemakers have a Right ventricular lead and a left ventricular lead. These leads force the ventricles to contract at the same time for “resynchronization” May not have atrial lead with history of chronic atrial fibrillation Implantable Cardiac Device Function and Programming Sensing What the device “sees” • Monitor the hearts intrinsic electrical activity Think of a fence… “Can’t see the hearts activity?!?”, (Undersensing) “Sees too much!” (Oversensing) EMI, Myopotential “Ahhh, Just Right!” (Appropriate sensing) Pacing The delivery of an electrical impulse to elicit contraction of the heart muscle. CAPTURE THRESHOLD – minimum amount of energy needed to elicit contraction of the heart. • Amplitude – How much energy (measured in Voltage) • Pulse Width – Over what time period (measured in ms) Voltages are set to 2 times the amplitude of capture threshold to ensure safety Pacing Parameters Lower Rate Limit (LRL): Nominal - 60bpm Rest rate – 50bpm Pts with AF s/p AVNA 80bpm for 6 weeks PVCs Upper Rate Limit (URL): How fast device will pace Patient can have OWN intrinsic rates higher that programmed URL Sensors – Rate Response (Not to be confused with “sensing”) Provide appropriate increase in heart rate with activity for the those patients who have chronotropic incompetence “Accelerometer” • Spring board system • Measures heal strike “Physiologic” • Only available in pacemakers • CLS (closed loop system) • Minute Ventilation – not appropriate for patient’s on a ventilator Magnet Response Pacemakers • “Shuts the eyes of the pacemaker” (Sensing) • Force A/V pacing at a specific rate, which is dependent on the pacemaker manufacturer (Ranging between 85-100bpm) ICDs • Temporarily deactivates ICD therapies Basic Differences between Pacemakers and Defibrillators Pacemakers Maintain HR, CO and AV synchrony Pace at a specified rate when magnet is applied Are not defibrillators They do not stop fast heart rates Defibrillators All have pacemaker component, but may not be utilized if no pacing indication Treat sustained VT/VF with pacing (ATP) and or shocks Magnet application suspends detection for VT/VF and prevents treatment. It does not affect Pacing rates. Keeping it Simple • ICDs are intended to treat potentially life threatening arrhythmias. • ICDs can function as a Pacemaker when pacing is indicated. NBG Code NASPE/BPEG Generic I II III IV V Chamber(s) Paced Chamber(s) Sensed Mode(s) of Response Programmable Functions Antitachycardia Functions A = Atrium A = Atrium T = Triggered R = Rate Modulated P = Paced V = Ventricle V = Ventricle I = Inhibited C= Communicating S = Shocks D = Dual (A&V) D = Dual (A&V) D = Dual M= D = Dual (P&S) O= None O = None O = None Multiprogrammable P = Simple Programmable O = None O = None Common Pacing Modes Single Chamber • VVI • VVIR • AAI • AAIR Dual Chamber • DDD • DDDR • DDI • DDIR VVIR V: ventricle is paced V: ventricle is sensed I: pacing is inhibited in response to a sensed event R: rate responsive This is a ventricular demand mode with artificial rate response D D DR D: both chambers are paced D: both chambers are sensed D: pacemaker will either inhibit or trigger in response to a sensed event R: rate responsive This is a dual chamber “universal” mode with artificial rate response Four Faces of DDD Pacing Atrial pace - Ventricular pace Atrial pace - Ventricular sense Atrial sense - Ventricular sense Atrial sense - Ventricular pace DDD Pacing Example Atrial Pace – Ventricular Pace DDD Pacing Example Atrial sense - Ventricular pace “Atrial tracking” DDD Pacing Example Atrial Pace – Ventricular Sense Could this be normal DDD Pacemaker Function? Normal sinus rhythm with no pacing YES! What About This? Atrial Flutter with Variable V rate Absolutely! Identifying Pacemaker/ICD Related Issues What do you see? Capture Loss ofOf Capture Loss Capture What do you see? Loss Of Capture Undersensed QRS Undersensing More Undersensing undersensing Typical Paced Beat Normal and Psuedofusion look the same Pseudofusion Fusion beats can have several different looks Helpful steps to take when calling for trouble shooting assistance • Make sure the telemetry monitor is not undersensing beats such as a PVC. • Make sure the “pacing spikes” are not artifact • Please save copies or telemetry strips for questionable rhythms. • Often we can determine if device functionality is an issue just by looking at these. • Whenever possible, make sure to save 2 ECG channels. New Advancements in the World of Cardiac Devices Implantable Loop Recorders Implantable Loop Recorder A Smaller version The Evolution of Pacemakers Then Now Leadless Pacemakers Progression of ICDs Subcutaneous ICD It is always a good idea to have device settings posted above the head of the bed. • Device settings can be obtained from the cardiac rounding nurse • Signs for posting should be located at central stations on your unit • Essential information lower and upper rate limits for pacing Intervention rates for VT and VF Need Help? Questions or Concerns? Page the Pacemaker Nurse (734) 670-1825 Available M-F 8am to 5pm After hours page appropriate company representative P Questions?!? References Biotronik (n.d.). Closed Loop Stimulation (CLS). Retrieved February 16, 2015 from http://www.biotronik.com/wps/wcm/connect/en_us_web/biotronik/sub_top/ healthcareprofessionals/products/bradycardiatherapy?p=http://www.biotr onik.com/wps/wcm/connect/en_us_web/biotronik/sub_top/healthcareprofes sionals/products/bradycardiatherapy/closed_loop_stimulation/page_closed _loop_stimulation&pw=974&pt= Boston Scientific. (2011). Restoring Appropriate Rate for Chronotropic Incompetence. Retrieved February 16, 2015 from http://www.chronotropic- incompetence.eu/en/treatment-of-chronotropic-incompetence Kutalek, S., Sharma, A., McWilliams, M., Wilkoff, B., Leonen, A., Hallstrom, A., & Kudenchuk, P. (2008). Effect of pacing for soft indications on mortality and heart failure in the dual chamber and VVI implantable defibrillator (DAVID) trial. Pacing & Clinical Electrophysiology, 31(7), 828-837 Medtronic, (2013). Clinical gudelines and inidcations. Retrieved February 16, 2015 from http://www.medtronic.com/for-healthcare-professionals/products-therapies/cardiacrhythm/therapies/tachyarrhythmia-management/clincial-guidelines-indications/ The NBG Code, (n.d.). The NBG Code: NASPE?BEPG generic. Retrieved February 16, 2015 from http://www.pacemaker.vuurwerk.nl/info/nbg_code__naspe.htm