* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Protein Synthesis Inhibitors
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Magnesium transporter wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Ciprofloxacin wikipedia , lookup
Levofloxacin wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
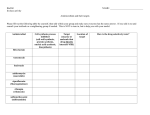
Protein Synthesis Inhibitors BY S.Bohlooli, PhD School of Medicine, Ardabil University of Medical Sciences Protein Synthesis Inhibitors Tetracyclines Amimoglycosides Macrolides Clindamycin Chloramphenicol Streptogramines Oxazolidinones Tetracycline First compound, chlortetracycline introduced in 1948 Highly effective against rickettsiae, gm + and – bacteria, chlamydia Inhibit protein synthesis by reversibly binding to 30 S subunit of bacterial ribosome, preventing binding of aminoacyl tRNA to mRNA ribosomal complex Bacteriostatic Chemical Structure Chemical Structure Inhibition of bacterial protein synthesis by tetracyclines. Resistance Wide resistance limits clinical uses Most penicillinase-producing staphylococci are resistant Absorption Incomplete GI absorption: tetracycline (6080%), doxycycline (95%), minocycline (100%) Dairy foods decrease absorption by forming nonabsorbable chelates with calcium ions; also Mg, Fe, Al (antacids) Distribution Widely distributed in body Bind in tissues undergoing calcification (teeth, bones) or tumors with high calcium content (gastric carcinoma) All cross placenta and concentrate in fetal bones and teeth Minocycline best CSF penetration Concentrated in saliva and gingival fluid Excretion Concentrate in liver and partially metabolized Secreted into bile and excreted in urine Doxycycline and minocycline largely excreted in feces Use in renal insufficiency General Therapeutic Uses Lyme disease Mycoplasma pneumonia Young adult pneumonia Rocky mountain spotted fever Spirochete (Borelia burgdorferi) tick bite Skin lesions, headache, fever, meningioencephalitis, arthritis Fever, chills, bone and joint aches Acne General Therapeutic Uses Chlamydia Lymphogranuloma venereum- lymph node hypertrophy, obstruction, elephantiasis Psittacosis- pneumonia, hepatitis, myocarditis, coma Cholera Ingested fecally contaminated food or water Organism multiplies in GI tract and secretes enterotoxin producing diarrhea Doxycycline reduces organism Fluid replacement Adverse Effects GI discomfort Hepatic injury Anorexia, epigastric pain, abdominal distention, nausea, vomiting, diarrhea, sore mouth, perianal irritation Increased during pregnancy Nephrotoxicity Adverse Effects Teeth Depression of bone growth Deposition in fetal and growing bones, stunted growth Photosensitization Discoloration enamel and hypoplasia of teeth Severe sunburn in sun; doxy/demeclocycline Superinfections Candida or GI staphylococcus Contraindications Pregnancy Children Renal insufficiency Can use doxycycline Drug Interactions Do not give with other antibiotics unless establish synergy Increased effects of anticoagulants Not absorbed by cations like Ca, Mg, Fe, Al H2 blockers may depress tetracycline uptake Aminoglycosides Contain amino sugars linked to aminocyclitol by glycosidic bonds Binds to 30 S ribosomal subunit (streptomycin) or 50 S (gent/others), interfering with assembly of functional ribosomal apparatus or misreading of genetic code Aerobic gram negative bacteria Bactericidal or static Typical Minimal Inhibitory Concentrations of Aminoglycosides That Will Inhibit 90% (MIC90) of Clinical Isolates for Several Species MIC90, mg/ml SPECIES KANAMYCIN GENTAMICIN NETILMICIN TOBRAMYCIN AMIKACIN Citrobacter freundii 8 0.5 0.25 0.5 1 Enterobacter spp. 4 0.5 0.25 0.5 1 Escherichia coli 16 0.5 0.25 0.5 1 Klebsiella pneumoniae 32 0.5 0.25 1 1 Proteus mirabilis 8 4 4 0.5 2 Providencia stuartii 128 8 16 4 2 Pseudomonas aeruginosa >128 8 32 4 2 Serratia spp. >64 4 16 16 8 Enterococcus faecalis æ 32 2 32 ≥ 64 Staphylococcus aureus 2 0.5 0.25 0.25 16 * Adapted from Wiedemann, B., and Atkinson, B.A., 1991. Resistance Decreased uptake Altered receptor Absent oxygen-dependent transport 30S ribosomal subunit binding site has lower affinity for aminoglycosides Enzymatic modification Plasmid R factors that synthesize enzymes to modify and inactivate antibiotic Administration Inadequate absorption when oral All parenteral, except neomycin Neomycin Severe nephrotoxicity Only topical use to reduce intestinal bacteria Distribution Good body fluid penetration, except CSF Accumulation in renal cortex and inner ear lymph All cross placenta Metabolism Rapidly excreted into urine Alter dose in renal insufficiency General Therapeutic Uses Streptomycin Bacterial endocarditis (+ Pen) Tuberculosis (combination) Tularemia- hunters skinning infected animals Gentamycin: combination with Pen/Ceph Urinary tract infections (E coli, enterobacter) Pneumonia (pseudomonas, E coli, kleb) Meningitis Peritonitis General Therapeutic Uses Tobramycin Same as gentamycin Poor activity against enterococci Amikacin Initial treatment of serious nosocomial gram negative bacilli infections when resistance to gentamycin and tobramycin General Therapeutic Uses Netilmicin Kanamycin Serious infections with enterobacteriaceae and other aerobic gram negative bacilli Few indications Neomycin Topical skin and mucosa infections Adverse Effects Ototoxicity Nephrotoxicity Neuromuscular paralysis High peak levels and long duration Intraperitoneal/intrapleural high dose; myasthenia gravis patients at risk Contact dermatitis- neomycin topical Monitor peak and trough plasma levels Macrolides Many membered lactone ring where sugars or amino acids are attached Erythromycin Azithromycin Clarithromycin- more strep and staph Dirithromycin Troleandomycin Telithromycin Mechanism of Action Bind to 50 S subunit of bacterial ribosome, inhibiting translocation step of protein synthesis Bacteriostatic activity Better intracellular concentration with gram + bacteria Clarithro and Azithro more anaerobic Inhibition of bacterial protein synthesis by the macrolide antibiotics erythromycin, clarithromycin, and azithromycin Resistance Inability of organism to take up antibiotic Decreased affinity of binding site for antibiotic Administration Adequate oral absorption Intravenous: thrombophlebitis Intramuscular: painful Distribution Well into body fluids, except CSF Diffuses into prostatic fluids Accumulates in macrophages Concentrated in liver Penetrate well into abscesses Metabolism Inhibits oxidation of other drugs through interaction with cytochrome P-450 system Excretion Concentrated and excreted in an active form in the bile Partial reabsorption through enterohepatic circulation General Therapeutic Uses Mycoplasma pneumonia Syphilis- in penicillin allergic Chlamydia- alternative to tetracycline; during pregnancy Legionellosis pneumonia Corynebacterium diptheriae- carriers Ureaplasma- urethritis General Therapeutic Uses Alternative to penicillin in allergic patients Clarithromycin (Biaxin) and Azythromycin (Zithromax) COPD, pneumonia Pharyngitis, tonsillitis Acute maxillary sinusitis Lower respiratory tract infections Adverse Effects Epigastric distress Cholestatic jaundice Nausea, vomiting, pain, diarrhea When estolate form is used Ototoxicity High doses Interactions Increases plasma concentration of digoxin Inhibits hepatic metabolism of drugs Theophylin Warfarin Carbamazepine Cyclosporin Methylprednisolone Terfenadine Do not use in liver disease patients Clindamycin Introduced in 1970 Semisynthetic derivative of lincomycin, isolated from soil near Lincoln, Nebraska in 1965 Clindamycin produced by exchange of hydroxyl group with chlorine atom at C7 of lincomycin molecule Clindamycin Binds to 50 S subunit of bacterial ribosomes to inhibit protein synthesis Bacteriostatic activity, but cidal action against susceptible organisms in vivo Spectrum Similar to erythromycin Increased activity against gram + and anaerobes, staph aureus Bacteroides fragilis Pharmacokinetics Well absorbed orally Distributes well into body fluids, not CSF Good bone penetration Excreted into bile or urine Therapeutic Uses Strep, Staph, pneumococci, anaerobic infections Purulent osteitis or other bone infection caused by anaerobes Adverse Effects GI distress Diarrhea Pseudomembranous colitis- caused by clostridium difficile Superinfections Fungal overgrowth in oral cavity, intestine, vagina Chloramphenicol Binds to 50 S ribosomal subinit Bactericidal or static Broad spectrum Mechanism of inhibition of bacterial protein synthesis by chloramphenicol. Pharmacokinetics IV or orally Complete oral absorption Excretion depends on conversion in liver to glucuronide, then secretion in kidney Therapeutic Uses Severe odontogenic infections threatening orbital contents or brain Penetrates well into brain and CSF Typhoid fever- salmonella Refractory meningitis by h. influenza, s. pneumonia, n. meningitidis, rickettsia, brucella, bacteroides Adverse Effects Anemias Hemolytic, reversible/mild, aplastic Gray baby syndrome Neonates if doses not adjusted Low capacity to glucoronidate antibiotic and underdeveloped renal function Decreased excretion ability Poor feeding then cyanosis then death Streptogramins Quinupristin-dalfopristin Rapidly bactericidal for most organisms except Enterococcus faecium Significantly inhibit CYP3A4 Oxazolidinones Linezolid Active against gram-positive organisms Bacteriostatic Inhibits protein synthesis