* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Incubation period
Toxocariasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Neonatal infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
West Nile fever wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Sarcocystis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Hepatitis C wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hepatitis B wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Leptospirosis wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
FOODBORN INFECTIONS AND
INTOXICATIONS
Mgr. Dana Hrnčířová
Dpt. of Nutrition
3rd Faculty of Medicine
Charles University in Prague
FOODBORNE INFECTIONS AND
INTOXICATIONS
wide group of infectious diseases
spread through contaminated food and water
by contact with vomit or feces
caused by pathogens and toxins
more than 250 infectious agents
INFECTIOUS AGENTS
microorganisms and microbial toxins:
bacteria, bacterial toxins, viruses, fungi, protozoans
enter the body through the gastrointestinal tract, and often causes
the first symptoms there:
nausea, vomiting, abdominal cramps and diarrhea
secreted by faeces and urine
TRANSMISSION
Arthropods and other organisms transmit pathogens to
animals (including humans):
at the end of an incubation period
in the course of an illness
during reconvalescence
Primary contamination
Secondary contamination (cross contamination)
FOODBORNE OUTBREAKS
two or more people get sick from the same food
Size and extent is based on:
which pathogen or toxin is involved
how much food is contaminated
where in the food production chain contamination occurs
where the food is served
how many people eat it
FOODBORNE OUTBREAKS
Sporadic: illnesses that are not part of outbreaks
Small (local) outbreak
Regional, statewide outbreak
Endemic (local limitation)
Epidemic (local and time limitation)
Pandemic (without local and time limitation)
THE MOST COMMON FOODBORN ILLNESSES
US
Pathogen
Estimated No
of illnesses
%
Norovirus
5,461,731
58
Salmonella (nontyphoidal)
1,027,561
11
Clostridium perfringens
965,958
10
Campylobacter spp.
845,024
9
Staphylococcus aureus
241,148
3
Subtotal
Source: CDC's 2011 estimates for foodborne illness
91
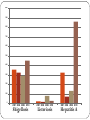
40,000
35,000
33,594
30,724
30,000
25,492
25,102
25,000
22,713
21,653
21,161
20,000
15,000
8,622
10,000
5,000
0
2001
2004
2006
Salmonellosis
2010
2001
2004
2006
2010
Campylobacteriosis
1000
900
800
700
600
500
400
300
200
100
0
2001 2004 2006 2010
Shigellosis
2001 2004 2006 2010
Listeriosis
2001 2004 2006 2010
Hepatitis A
SALMONELLOSIS
2 species Salmonella enterica
Salmonella bongori
intestines of birds, reptiles and mammals
most important in foodborne disease:
S. enterica subspecies enterica (cca 1500 serotypes)
serotype Enteritidis abbreviated to S. Enteritidis
serotype Typhimurium (≠ S. Typhi!)
serotype Infantis
SALMONELLA - growth and survival
Growth: 7 - 48 ºC
pH 3.7- 9.5
Resistant to: drying
low temperatures
survives chill and freezing temperatures
Facultative anaerob
Inactivated by: heat above 70 °C (pasteurization, …)
pH below 3,8
disinfection (sanitizers)
SALMONELLA - infective dose
Infective dose vary widely:
105-106 cells
the young or the elderly: 10 - 100 cells
Period of infectivity: during illness, reconvalescence
SALMONELLA - transmission
Salmonellosis - a zoonotic infection
S. lives in intestines of humans and other animals
- reptiles, chickens, young birds
Feces of infected animals → enviroment (soil, surface water)
↓
Food animals (pigs, polutry) ← feed, infected animals
Fresh produce
Direct contact by hands of an infected food handler
Via food preparation surfaces or equipment
SALMONELLA - occurrence in foods
Foods of animal origin (meat, poultry, eggs and raw milk)
Fresh produce
Cooked ready-to-eat foods (cross contamination)
Processed food
Examples:
Confectionery, pastries (custard, egg white coating)
Cooked ready to eat food containing eggs
Bologna sausage, tripe sausage, meat loaf, liver paste
SALMONELLOSIS - symptoms
non-typhoid salmonellae
incubation period: 12 – 36 hours
1-7 days
diarrhea, abdominal pains, nausea, vomiting, chills
dehydration and headaches
Susceptible individuals: more severe symptoms
septicaemia, or chronic conditions (reactive arthritis)
Salmonella Typhi
Typhoid fever (≠ typhus - rickettsia)
vaccination
SALMONELLOSIS - treatment
Gastroenteric form:
oral fluids
severe diarrhea - rehydration with intravenous fluids
Typhoid form:
ATB (e.g. ampicillin, chloramphenicol)
SALMONELLOSIS - prevention
Raw eggs!
Undercooked poultry and meat!
Raw or unpasteurized milk
Produce – washed thoroughly
Prevent cross-contamination!
Hand washing
….
CAMPYLOBACTERIOSIS
Bacteria C. jejuni (birds)
C. coli (pigs)
Low resistance to enviroment:
Microaerophilic (require reduced levels of oxygen) to grow
Heat sensitive: destroyed at temperatures above 48 °C
Sensitive to salt: 1 % or more – bactericidal
Inactivation: pH < 4.0
Can survive for a short time at refrigeration temperatures!
CAMPYLOBACTERIOSIS
- transmission and sources
Intestines of warm-blooded animals (esp. birds – poultry)
Poor hygiene (faecal/oral route)
Fresh poultry and related products
Other fresh meats
Raw milk
Shellfish
Salads, …
CAMPYLOBACTERIOSIS
Incubation period: 3 – 5 days
Length of infection: 1-7 days
Infective dose: 103
Symptoms: diarrhea, cramping, abdominal pain, and fever
SHIGELLOSIS
Shigella - a family of bacteria that causes diarrhea in humans
Shigella sonnei (" Group D" Shigella) over 2/3 of shigellosis
in the US, in CR over 90 % of cases
Shigella flexneri ("group B" Shigella) almost all the rest
Other types, e.g. Shigella dysenteriae type 1 – developing
world
SHIGELLOSIS
highly infective disease, infective dose 200 cells
incubation period 1-3 days
duration: 5-7 days
SYMPTOMS:
diarrhea (distal part of colon) – with mucus and blood
fever
stomach cramps
risk of dehydration and perforation of colon
SHIGELLOSIS
Sources of infection:
infected person (diarrheal stools – poor hygiene)
contaminated food
contaminated water
LISTERIOSIS
bacteria Listeria monocytogenes syrotype 1/2a, 1/2b and 4b
grows at chill temperatures
tolerant of high sodium chloride levels
grows well in aerobic and anaerobic conditions
inactivated at temperatures above 70 ºC
Infectious dose:
healthy persons: 103
LISTERIOSIS
Incubation period: 1 to 90 days (mean 30 days)
SYMPTOMS:
flu-like symptoms, nausea, vomiting, diarrhea
meningitis, septicaemia
Pregnant women: mild flu-like ilness (fever, headache)
! infection of the fetus → miscarriage, stillbirth, birth
of an infected infant (meningitis)
Overall mortality rate: 30 %
LISTERIOSIS - sources of infection
Row foods (vegetable)
Cooked foods – post-process contamination
Processed foods:
soft cheeses
unpasteurized milk
confectionery, pastries
cooked meat products
pâtés, ice cream
smoked and lightly processed fish/seafood products
ESCHERICHIA COLI (VTEC, STEC)
verocytotoxin producing (Shiga-like toxin-producing ) E. coli
subset of serotypes: enterohaemorrhagic E. coli (EHEC)
highly pathogenic
haemorrhagic colitis, HUS
outbreaks of severe foodborn disease in many countries (serotype
Escherichia coli O157:H7, Germany 2011- O104:H4)
Foods derived from cattle (minced beef – Hamburger disease)
Dairy products derived from raw milk
TOXOPLASMOSIS
protozoan parasite Toxoplazma gondii
Foodborne transmission (undercooked, contaminated meat)
Animal-to-human transmission (cat’s feces)
Mother-to-child transmission
Mothers often without symptoms
Miscarriage, stillborn child
Congenitally infected infants - later in life: mental disability,
potential eye loss
Incubation period: 5 – 23 days
TOXOPLASMOSIS – life cycle
TAENIASIS
parasitic infection
tapeworm species:
Taenia saginata (beef tapeworm) – e. Africa
Taenia solium (pork tapeworm) – India, s. Africa, s. America
Taenia asiatica (Asian tapeworm) – Republic of Korea, China,
Taiwan, Indonesia, Thailand
raw or undercooked beef or pork!
TAENIASIS - symptoms
Most people – no / mild symptoms:
abdominal pain, loss of appetite, weight loss, upset stomach
T. saginata: more symptoms because of the size (up to 10 meters)
T. solium: cysticercosis
neurocysticercosis (epileptic seizures)
eye damage
in muscles – often asymptomatic
TAENIA – life cycle
TRICHINELA
parasitic infection
Roundworms (nematodes), genus Trichinella
classical agent T. spiralis (worldwide, carnivorous and
omnivorous animals)
other species
T. pseudospiralis (mammals and birds
worldwide)
T. nativa (Arctic bears)
T. nelsoni (African predators and scavengers)
T. britovi (carnivores of Europe and western Asia)
Row, undercooked meat!
TRICHINELA - life cycle
VIRAL INFECTIONS
Hepatitis A, E
Tick-borne encephalitis
Norovirus and rotavirus (small children up to 5 yrs)
Norovirus - Norwalk-like virus (Norwalk, Ohio in 1968)
- extremely infectious enteric virus
- acute viral gastroenteritis
- infected persons, contaminated food/water/ surfaces
HEPATITIS A
Hepatitis A virus
Foodborne hepatitis
Transmission:
direct person-to-person contact via the faecal-oral route
foodborne transmission
infected food handler
foods faecally contaminated (water)
Long incubation period (aprox. 4 weeks)
Often asymptomatic (esp. Children – source of the virus!)
Shellfish, fresh fruits/ vegetable, iced beverages, milk products etc.
resistant at 70°C for up to 10 mins, inactivated at 85°C for 1 min.
HEPATITIS E
Foodborne disease
No chronic infection
Contaminated water!
Countries with poor sanitation
No approved vaccination in US and Europe
Hepatitis A and E
1800
1600
1400
1200
Hepatitis A
1000
Hepatitis E
800
600
400
200
0
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
FOODBORNE INTOXICATIONS
Intoxication
consumption of toxins produced by bacteria in food
Staphylococcus aureus, Clostridium botulinum,Vibrio parahemoliticus
Toxin-mediated infection
toxin is produced in the intestine
Clostridium perfringens type A
Bacillus cereus: two types of toxins
1. Type A - heat resistent toxin, produced in food (staphylococ-like
symptoms)
2. Type B - heat labile toxin, produced in GIT (clostridium-like
symptoms)
Staphylococcal intoxication
Staphylococcus aureus
heat resistant toxin
produced in food
incubation period: 1-6 hours
Symptoms: nausea, abdominal cramps, vomiting, exhaustion
Source: people (nose, throat, infected skin wounds, pimples)
Cream fillings (esp. with eggs), potato and meat salads,
processed meats, minced meats
Clostridium perfringens type A
heat labile toxin
produced in the intestine
incubation period: 10-12 hours
Symptoms: diarrhea, abdominal cramps, nausea
holding meats at warm room temperature for several hours or cooling
large pots of meat or gravy too slowly in the refrigerator
Bacillus cereus
Type A toxin (emetic form)
heat resistant toxin
produced in food
staphylococcus-like symptoms (nausea, vomiting)
incubation period:1-5 hours
cooked pasta, rice
Type B toxin (diarrheal form)
heat labile toxin
produced in the intestine
clostridium-like symptoms (watery diarrhea, abdominal cramps)
incubation period: 5-16 hours
meat, milk, vegetable
Botulism
heat labile paralytic neuro-toxin
produced in food
incubation period: 12-36 hours
Three main types:
foodborne botulism (food)
wound botulism (toxin produced in a wound)
infant botulism (consumed botulinum spores release toxin in GIT)
Spores – destroyed at 120 °C for 20 min.
Toxin – inactivated by boiling for 10 min.
Botulism
Growth of C. botulinum:
Acidity - inhibited at a pH of 4.6 or lower
Oxygen – anaerobic organism
Home-canned and home-cooked food (meat and vegetable)
Symptoms:
blurred double vision, difficulty in swallowing and speaking
Paralysis (respiratory muscles, peristalsis, urination)
Botulism
Treatment:
remove any unabsorbed toxin in GIT
neutralize the circulating toxin with an antitoxin
keep a patient breathing by a mechanical respirator as necessary
Recovery – weeks to months
Use of toxin (BOTOX):
Strabismus
wrinkles and frown lines
underarm sweating etc.
THANK YOU FOR YOUR ATTENTION.