* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download A family history of cancer: How to find it and what to do about it.
Survey
Document related concepts
Transcript
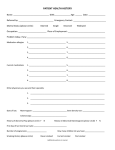
A family history of cancer: How to find it and what to do about it. Lynn Greenhalgh Macmillan Cancer and General Consultant Clinical Geneticist Cancer 1 in 3 of us develop cancer We all know someone who has had cancer Family history of cancer Most us of have a family history of cancer Does is matter? Cancer Genetics Cancer that may have a genetic basis That is there may be an inheritable component to the cancer Cancer Genetics If we know that someone is more likely to develop a cancer then…… Can we offer that person options about how they want to manage that risk? Cancer Genetics 5-10% of cancers have a genetic component Fewer still have a single gene cause How do we identify those at risk of an inherited cancer? We need to ask people about their family history of cancer. Then we need to calculate and stratify their risk. Golden rules of cancer genetics Is there more cancer than we would expect to happen by chance? Are the cancers the same or related cancers? Are the cancers occurring at a younger age than we would expect? Are the cancer seen in different generations? Risk groups Low risk Moderate risk High risk Low risk Approximately that of the general population No extra screening May need emotional support Moderate risk Increased risk above that of the general population Extra screening recommended Gene testing not appropriate (yet) Avoid environmental exposures High risk At high risk of developing cancer Extra screening recommended Gene testing sometimes available Risk reducing surgery sometimes appropriate Management of risk groups Low risk - Primary Care Moderate risk – Secondary Care High risk – Clinical Genetics What sort of cancers can be inherited? Many different sorts. Breast/Ovarian cancer Bowel cancer Endocrine cancers Childhood cancers Many more… Some examples of families Breast cancer family Bowel cancer family Breast Ovarian Cancer Family Tree Died young man Br Ca @late30's Breast Ca @ 36yrs Mutation Positive 18 13 9 Lymphoma @61yrs Recieving Br Screening Heart Attack Heart Attack Ca Ovary @45yrs Mutation Positive Pancreatic Ca@62yrs No information Br CA@50's Double Mastectomy ?cancer Initial observations Cancer happening at a younger age than we would expect In different generations Same or related cancers More than we would expect Assessment This family meets the high risk criteria Put DNA forward for BRCA1 and BRCA2 analysis Results BRCA1 mutation What the results meant for the proband She is now aware that she is at increased risk of developing Another breast cancer Ovarian cancer We discuss how she wants to manage her risk Screening Risk reducing surgery What the result means for family members Mutation confirmed her affected sister Given her access to a chemotherapy trial Other family members can now have predicitve tests if they wish BRCA 1 High risk breast/ovarian cancer predisposition gene 80% lifetime risk of developing breast cancer 40-60% chance of developing ovarian cancer 30-50% chance of developing a second primary – breast or ovary BRCA2 Recognition that this is a much more multisystem disorder than BRCA1 40-60% chance of developing breast cancer 20% ovarian cancer if mutations are found in OCCR 16% chance of prostate cancer 5% chance of male breast cancer HNPCC family tree Ellen Ward d. MI Ca tongue d. 30s Ca colon/stomach d. 70s Ca colon d. early 40s William Minton 1941/1/16 Ca stomach/colon dx. 67 Glen Young Andrew Campbell Ca ovary dx. 47 endometriosis Paula Ward Ca ?cervix/uterus dx. 42 Stefan Himme Johnson Ca ovary dx. 42 (2007) endometriosis & endometrial atypical hyperplasia (2005) benigh fibrocystic breast disease (2001) non-neuropathic neuropathic bladder kidney removed due to reflux d. 32 heart problems Back to basic principles More cancer than we would expect to happen by chance? Younger age? Same or similar cancers? Different generation? Suspicious family……. Gene testing MLH 2 mutation What now for the family? Predicitve gene testing Ensuring that at risk individuals are offered appropriate screening Discussion of risk reducing surgery HNPCC – Modified Amsterdam criteria Three individuals with colon cancer First degree relatives of each other One with colon cancer under the age of 50 years Two other HNPCC related cancers Large bowel, small bowel Endometrial, ovarian, stomach, uro-epithelial……… HNPCC genes – MLH1 and MSH2 Male lifetime colon cancer risk of 80% Female lifetime colon cancer risk of 40-60% lifetime endometrial cancer risk of 40-60% lifetime ovarian cancer risk of >10% HNPCC genes – MSH6 Colon cancer lifetime risk of > 10% Endometrial cancer lifetime risk of 7075% How to identify at risk families Ask about a family history of cancer Who and when…. Wait for a patient to ask Wait for a cancer to occur Be proactive… Be proactive where.. When a patient presents with a cancer? When a patient presents with other problems? When a patient presents for screening? Cancer Genetics Wish List Equitable opportunity for all patients to consider their family history of cancer Guidelines about who has a significant family history of cancer Clear patient pathway for those with a significant family history of cancer Sefton Cancer Family History Project Sarah Reynolds, Commissioning Manager, NHS Sefton Finding out about family histories? Patient initiated enquires Known high risk families in general practice Symptomatic patients Other consultations eg hormonal contraception Best opportunity to be proactive…….. THE NEW PATIENT QUESTIONNAIRE AND INTERVIEW But should we be asking? NICE clinical guideline 41 familial breast cancer “healthcare professionals…. should not in most instances actively seek to identify women with a family history of breast cancer” Why make changes ? Some practices ask new patients about cancer FH Variation in what happened next Lack of clear guidance for primary care Why make changes? continued Breast FH clinics, NICE guidance Referrals made to Genetics, Gynaecology, Colorectal surgeons Need to verify reported histories Aims for the Project Use the new patient questionnaire /consultation to ask the right cancer FH questions Provide primary care with tools to make a broad assessment- to refer or not? Aims for the Project cont… Put consistent referral criteria and simple pathways in place Provide supportive patient information TRAINING PACKAGE CATH KIGHTLEY LIAISON GENETIC COUNSELLOR CONTEXT (review) The Cancer Family History Project-pilot across several practices Standarised New Patient Questionnaire, focused questions One of three assessment forms used-based on referral guidelines Pathway written for equity of service delivery May result in an enquiry or referral with patients consent Evaluate TRAINING NEEDS? New Knowledge Forms and pathways Patient anxiety How much to say Limits of knowledge What happens next? COMPETENCIES Already in place -7 in total (Kirk et al) A framework for practice-standards for practice What do practitioners feel they need- asking first E.g Genetics of cancer Managing issues arising Anxiety Ethical dilemmas e.g Confidentiality DELIVERING TRAINING (For the project) Overall Aim; Competent and Confident Practitioners in use of genetics knowledge and skills for benefit of all patients Modular Utilising already developed resources-genetics education centreBirmingham Face to Face-based around documents developed so far Include assessment Evaluate and improve package- DELIVERING TRAINING (After the project) Developing an e-learning package-Whats already in place? We don’t want to re-invent the wheel Ideas Different learning approaches-e.g videos Fitting with own role pressures Modular and with ?online assessment tools Evaluation and constant development POSSIBLE CONTENT OF TRAINING PACKAGE Introduction to Genetics Taking a targeted family history-eg Jewish ancestry Basic Genetics of breast and/ or ovarian cancers Genetics of bowel cancer and related cancers Genetics of other relevant cancers Use of the forms/ Pathway Communication re genetics Issues arising-e.g confidentiality The future in genetics There are resources out there –Centre for genetics educationBirmingham EXPECTED OUTCOMES Newly registering patients have opportunity to clarify risk Clear pathway across practices Standardised approach Awareness raising across practices Equity of access to training across practices for patient benefit Training package transferable to other areas of practice